Introduction
Overactive bladder (OAB) is a common and chronic symptom complex that increases in prevalence with advancing age and has a known adverse effect on quality of life. OAB is a highly prevalent condition affecting 16.6% of the European population. Women are more commonly affected, and there is an increased incidence with age. Studies in the United States suggest a prevalence of up to 43% in women and 27% in men older than 40 years of age. There are significant differences in racial/ethnic groups with OAB being highest in African Americans. The International Continence Society (ICS) has recently defined OAB as urgency with or without urgency urinary incontinence (UUI), usually with frequency and nocturia. This definition is based on symptoms and does not require urodynamic investigation (UDS). It is important to note that many clinicians use urodynamics to diagnose detrusor overactivity (DO) before initiating treatment. OAB is often defined clinically by urodynamic variables thought to be responsible for the symptoms [1, 2].
A focused history is paramount in diagnosing OAB. It is critical to assess onset of symptoms as well as aggravating and alleviating factors and 24/h pad use. Physical examination should include the assessment of the genitourinary system, as well as digital rectal and prostate examination and in men and vaginal examination in women. Urinalysis, by dipstick initially, should be performed to rule out hematuria and infection. Validated questionnaires are available to assess effects on quality of life as well as symptoms. Bladder diaries or frequency-volume charts provide an accurate and reliable measure of voiding patterns. Imaging of the urinary tract is not required for diagnosis but may be used as sadditional test in those patients with suspected bladder outflow obstruction [2, 3].
The use of urodynamics in the diagnosis of OAB remains controversial. Although the gold standard diagnostic test for detrusor overactivity, it is an invasive procedure and therefore should be limited to those with refractory OAB. The National Institute for Health and Care Excellence (NICE) advises urodynamics prior to third-line therapy, European Urological Association (EAU) only if findings may change management and the American Urological Association (AUA) for patients with complicated OAB (such as those with concurrent urethral dysfunction or in those in whom the diagnosis is not clear [2, 4].
In the UK, a nationally funded National Institute for Health Research superiority trial has just finished recruitment looking at the usefulness of urodynamics prior to treatment for refractory OAB syndrome [2].
The consensus is that UDS is not indicated in patients with OAB prior to conservative or medical therapy. The main area of debate is that many clinicians believe that UDS is indicated in refractory OAB and only when initial therapy fails and it should be performed prior to any surgical intervention including minimally invasive procedures, such as sacral neuromodulation or onabotulinum toxin type A injection. They support this opinion with studies that showed that UDS is an invasive expensive tool, time consuming, and does not influence the initial management strategies [5].
Combination therapy (antimuscarinic and beta3-agonist) may be considered in patients refractory to monotherapy. Co-administration appears to improve efficacy with minimal increase in the side effect profile. Solifenacin and Mirabegron combination therapy (in doses of 5mg and 25mg or 5mg and 50mg, respectively) is reported to have a statistically significant decrease in number of incontinence episodes and micturition compared with Solifenacin or Mirabegron alone [2, 4, 6].
The aim of the present study was to analyze whether patients with OAB need different treatment management and if it is dependent on establishing on urodynamics study presence of overactive detrusor contractions.
Material and methods
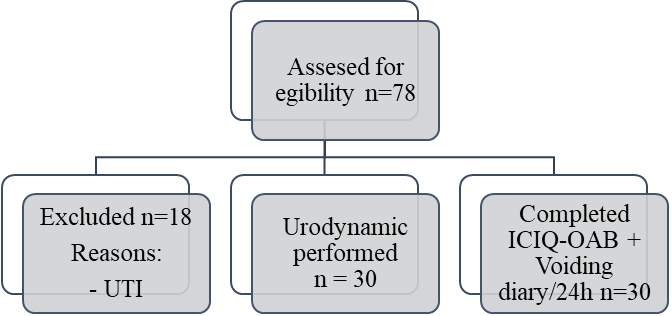
A prospective and randomized study was performed in 60 patients with OAB symptoms who followed behavioral therapy without any effect. The study cohort was divided in two groups. 30 patients (group A) with the mean age of 40 years were treated without a prior urodynamic study, and 30 patients (group B) with a mean age of 41.5 years with overactive detrusor, underwent a urodynamic testing prior to pharmacotherapy based on EAU guidelines that recognize the benefit from addition of Mirabegron 50 mg/day to Solifenacin 5 mg/day, and on the AUA guidelines that recommends combination therapy in patients with OAB. The study was performed during 2019-2022, at the Department of Urology and Surgical Nephrology, Nicolae Testemitanu State University of Medicine and Pharmacy, Chisinau, Republic of Moldova.
In this study, fundamental ethical principles of research have been respected. All patients gave informed consent before study entry. The study protocol was endorsed positively by Nicolae Testemitanu University Research Ethics Committee (Minutes No. 24, 05.03.2021). Patients who underwent the surgical procedure, were asked to explain that they understood the nature of the surgical procedure and after they gave the agreement for operation by signing the informed consent.
|
Fig. 1 Flowchart of prospective study design |
All patients had moderate and severe clinical manifestations according to ICIQ-OAB. At 3-month follow-up, patients in both groups underwent the ICIQ-OAB questionnaire and voiding diary/24h.
The urodynamics were carried out in accordance with the trust standard operating procedures, which were based on the good urodynamic practice. Uroflowmetry was performed with women voiding in a private room on a flowmeter. Filling cystometry was performed in sitting position at 100 mLs/min rate, followed by provocation maneuver and ended with voiding cystometry. The clinician who performed the UDS recorded the findings and diagnosis on the UDS report and inside the patient’s notes.
Urodynamic studies were commonly performed for the diagnosis of OAB and DO using urodynamic equipment Medica S.P.A. Memphis Division (Medolla-Italy). Women with infravesical obstruction, detrusor underactivity and detrusor overactivity with inadequate contractility were excluded from this study.
Urodynamic parameters were PVR from ultrasound, maximum cystometric capacity (MCC), maximum detrusor pressure (MDP), maximum urinary flow pressure (PdetQmax), maximum urinary flow rate (Qmax) and bladder compliance (BC). BC was calculated using the ratio of urine volume to detrusor pressure, being considered low when ΔV/ΔPdet was ≤ 30-40 ml/cmH2O, despite unexplained and insufficient data on the presence of normal values.
The actual procedure was explained to all patients in a clear manner by providing a scenario, instructions on how to report the 4 sensations during the cystometry. Patients signed the informed consent before the procedure.
Rectal urodynamic catheter was inserted ~10 cm depth, after what the urethra was catheterized using a 7Fr double lumen urodynamic catheter. The bladder was emptied after confirmation of the lack of residual urine based on the urodynamic investigation. Patients placed in a sitting position after the filler wires have been connected. The transducers were placed at reference heights according to ICS standards with the respective calibration of atmospheric pressures. The working of transducers was confirmed after patients’ cough and the filling of the bladder was performed with saline solution prepared at room temperature (filling speed 20 ml/min). The filling was stopped once the patient reached the maximum cystometric capacity, then the patient urinated.
Statistical data analysis was performed using unifactorial dispersion analysis designed in Microsoft Excel 2019 database and IBM SPSS Statistics 22 software, using the standard and paired t-tests, with a significance level of 0.05. The categorical data were presented as absolute and relative values and the continuous data – in the form of mean and standard error, or as a percentage of results, comparing results before and after procedure.
Results
Urodynamics appears to influence treatment decisions made by clinicians and patients in determining treatment algorithms in women presenting with OAB. Women with DO were three times more likely than women with normal diagnosis to have been prescribed bladder relaxants. This could be interpreted as those who were shown to have DO either received prescribed bladder relaxant tablets more or patient compliance with taking the treatment was better. Women with a diagnosis of DO were 15 times more likely to have onabotulinum toxin type A injection than no treatment, which may at least partly explain the improved ICIQ-OAB scores in this group compared with group A.
Factors identified in this analyses that may influence the result of therapy include age, previous continence surgery, previous use of medication for bladder symptoms, menopausal status and parity. Studies in the past have shown that pelvic floor symptoms have a different impact on women of different ages. Progesterone and estrogen may exert or influence the female nerves, as well as influencing bladder contractions and voiding frequency.
Table 1. Voiding diary parameters in patients with overactive bladder symptoms. | ||||
Voiding diary parameters | Group A | Group B | ||
Pre-treatment (n = 30) | Post-treatment (after 3 months) (n = 30) | Pre-treatment (n = 30) | Post-treatment (after 3 months) (n = 30) | |
TVV / 24h (ml) | 1314 ± 645 | 1565 ± 168 | 1280 ± 635 | 1679 ± 168 |
FBC (ml) | 163.1 ± 123.9 | 338 ± 69 | 157.1 ± 115.5 | 378 ± 76 |
IN | 2.86 | 0.7 ± 0.1 | 2.75 | 0.5 ± 0.1 |
IPN (%) | 28.7 ± 9.4 | 15.8 ± 5.1 | 27.6 ± 7.4 | 11.8 ± 3.1 |
DV | 11.3 ± 1.68 | 5.1 ± 2 | 14.1 ± 1.45 | 6.1 ± 2 |
TUFS | 31.7 ± 7.8 | 7.7 ± 3.8 | 35.2 ± 6.2 | 5.7 ± 3.2 |
Note: TVV – total voided volume; FBC – functional bladder capacity; IN – Index of nocutia; IPN – Index of nocturia polyuria; DV – daytime voiding; TUFS – total urgency and frequency score. | ||||
Based on voiding diary, before and after treatment, there were analyzed indices of total voided volume, functional bladder capacity, nocturia index and nocturia polyuria index, number of daytime voiding and total index of urgency and frequency urination.
After 3 months of treatment, in both groups, patients obtained normal ranges of indices, and this correlates with the disappearance of clinical manifestation. We have observed what bladder voiding diary results were with respect to urgency, total voided volume, average voided volumes, and maximum functional capacity in relation to clinical and urodynamic diagnoses.
Table 2. ICIQ-OAB values in patients with overactive bladder symptoms. | ||||
ICIQ-OAB Domain | Group A | Group B | ||
Pre-treatment (n = 30) | Post-treatment (after 3 months) (n = 30) | Pre-treatment (n = 30) | Post-treatment (after 3 months) (n = 30) | |
Urinary frequency | 100% | 75% | 100% | 50% |
Urinary urgency | 100% | 75% | 100% | 20% |
Nocturia | 100% | 50% | 100% | 0% |
Urge urinary incontinence | 100% | 25% | 100% | 0% |
OAB-QoL | Severe | Mild | Severe | Light |
Note: ICIQ-OAB – International Consultation on Incontinence Questionnaire Overactive Bladder Module; OAB-QoL – International Consultation on Incontinence Questionnaire Overactive Bladder Quality of Life Module. | ||||
All validated self-report questionnaires quantifying OAB symptoms (daytime urinary frequency, nocturia, urinary urgency and urge urinary incontinence) and quality of life were completed by all women prior and after conservative treatment. A significant decrease of symptoms in patients from group B and of negative impact of LUTS/OAB on daily indoor and outdoor activity, physical and social activity was reported by patients following the urodynamic tests.
The ICIQ-OAB questionnaire indices and their improvements after pharmacotherapy in group B are shown in table 3. According to the results of the questionnaire, the clinical manifestations have improved after treatment, however in 50% of cases of urinary frequency and in 20% of urinary urgency remained unchanged.
Table 3. The effect of pharmacotherapy in patients with overactive bladder symptoms. | ||
| Group A | Group B |
Success | 61% | 81% |
Failure | 39% | 19% |
The success rate (61%) in the group A of patients was lower than in group B (81%). The proportion of patients who had urge urinary incontinence (OAB wet) rather than frequency-urgency (OAB dry) in this series was high (50%), and this may have had a significant impact on our success rate.
Table 4. The effect of pharmacotherapy in patients with overactive bladder symptoms compared by ICIQ-OAB questionnaire. | ||||
| Group A | Group B | ||
ICIQ-OAB | ICIQ-OAB | |||
Pre-treatment (n = 30) | Post-treatment (after 3 months) (n = 30) | Pre-treatment (n = 30) | Post-treatment (after 3 months) (n = 30) | |
Solifenacin + Mirabegron | Severe (100%) | Severe (25%) Mild (75%) | Severe (100%) | Severe (19%) Mild (70%) Absence of symptoms (11%) |
Note: ICIQ-OAB – International Consultation on Incontinence Questionnaire Overactive Bladder Module. | ||||
Patients from group A did not continue the conservative treatment for a long period due to lack of results and persistence of OAB symptoms after 2-3 weeks of treatment, but patients from group B having a confirmation of diagnosis of OAB with overactive detrusor were more confident in their treatment ant continued for longer period administration of pharmacotherapy.
The behavioral therapy was combined with pharmacotherapy in both groups for obtaining better results after 3 months of conservative treatment.
Both groups improved well during antimuscarinic treatment associated with Mirabegron, the severe manifestation of symptoms from baseline in urinary frequency or UUI episodes disappearing after 3 months.
Table 5. Urodynamic parameters in whom pharmacotherapy was successful and in whom it failed. | |||
| Success | Failure | |
Female | 16 (81%) | 4 (19%) | |
Urodynamic parameters | |||
Uroflowmetry | Maximum voided volume (ml) | 132.7 ± 136.7 | 95.2 ± 83.8 |
Qmax (ml/s) | 9.8 ± 4.1 | 8.4 ± 6.1 | |
Qave (ml/s) | 2.2 ± 1.6 | 2.1 ± 1.9 | |
Cystometry | FS (ml) | 79.8 ± 56.3 | 65.5 ± 45.7 |
FDV (ml) | 117.8 ± 103.2 | 101.8 ± 100.2 | |
SDV (ml) | 162 ± 125 | 134 ± 109 | |
MCC (ml) | 183.4 ± 139.8 | 141.1 ± 138.2 | |
MDP (cmH2O) | 45.9 ± 23.9 | 32.6 ± 21.9 | |
Number of contractions | 3.9 ± 1.1 | 5.6 ± 2.1 | |
BC (ml/cm H2O) | 10.6 ± 11.5 | 11.7 ± 12.8 | |
CI | 124.6 ± 39.4 | 133.4 ± 36.3 | |
PVR (ml) | 4.9 (0 - 10) | 2.4 (0 - 10) | |
Note: Qmax – maximum flow rate; Qave – average flow rate; FS – first sensation of bladder filling; FDV– first desire to void; SDV – strong desire to void; MCC– maximum cytometric bladder capacity; MDP – maximum detrusor pressure; BC – bladder compliance; CI – Index of detrusor contractility; PVR – post-void residual urine volume. | |||
Standard filling phase urodynamic parameters did not predict a successful response to pharmacotherapy although there is suggestion that sensory data is important. In patients from group B that failed the treatment, the urodynamic values were lower and the drug was less efficient than in subjects that had higher urodynamic values.
The symptomatology and urodynamic data did not display different values between the groups. The mean post-treatment score for group A was 11.7 ± 3.27 and for group B was 15.32 ± 2.14.
Ten subjects (eight receiving pharmacotherapy from group A and two from group B) presented adverse events. The most frequent adverse events reported were dry mouth (15%), dyspepsia (6%), and headache (9%). Other than dry mouth, no adverse event occurred in >10% of subjects.
Discussion
There are many studies that have utilized questionnaires and voiding diary for treatment response and success, however, this is a study that evaluates the importance of accuracy of urodynamic values in predicting the good result of treatment. The results of this study demonstrate that the UDS has an objective ability to establish a diagnosis of DO and predict a better result after pharmacotherapy.
The study was prospective, recruited consecutive women presenting with lower urinary tract symptoms and achieved its target sample size. The prevalence of DO in our study was in all women from group B. Ambulatory UDS was offered to 100% of women who presented OAB symptoms, all the criteria for a high-quality test accuracy evaluation have been met. Women were only included in group B if they had accepted the disclaimer at the end of the completing the ICIQ-OAB questionnaire.
The usefulness of UDS has been challenged in clinical practice. Some may question the relevance of DO when there are many women who have DO without any urgency or incontinence. The diagnosis of DO does not alter treatment outcomes for interventions like antimuscarinics, but the results from our study reveal the success rate of treatment.
According to the latest recommendations of the ICS and International Consultation for Incontinence (ICI) in 2016, UDS have an overall accepted indication to assess LUTS function and LUTD, especially when it may have a therapeutic consequence, and may change the therapeutic options or when it is performed as part of lower urinary tract assessment or research. It is considered the “gold standard” functional test to assess LUTS [5].
Cho et al. (2015) investigated the role of UDS in female patients with OAB. Clinical and urodynamic data of 163 women with OAB were analyzed. They concluded that OAB symptoms were not useful for predicting presence of voiding dysfunction and for this UDS may be necessary for accurate diagnosis in women with OAB symptoms [7, 8].
Many researchers believe that UDS is indicated only in patients with OAB symptoms after failure of first-line therapy. They believe that UDS will not change the initial management strategies in such patients in addition to its cost and invasiveness [5].
Conversely, many others believe that UDS is still mandatory in female patients with OAB, as treatment based on symptoms alone may lead to under diagnosis of DO and storage symptoms that can be detected by UDS which will ultimately alter the diagnosis and management plan. One retrospective single-center study confirmed that there is no association between subjective symptoms severity in patients with OAB and objective measures. This confirmed the role of UDS as an objective measure that is needed for better assessment [5, 8, 9].
When considering pretreatment UDS prior to third-line therapies, there are several questions to consider: (1) Does UDS predict treatment outcomes? (2) Do treatments have an impact on UDS findings? (3) If there is an impact, does it matter? Urodynamics should be used judiciously in such patients. However, for patients with known or suspected voiding phase dysfunction, those with rapidly changing symptoms, those in whom the diagnosis is not clear, those who have medical or urological histories that can affect outcomes of treatment, and in those with known or suspect neurological disease, urodynamics is often indicated, useful, and in some cases essential [8, 10, 11].
The role of UDS continues to be a heavily debated subject for assessing female patients with LUTS. Nonetheless, UDS remains a valuable diagnostic test that provides vital information, to both the surgeon and the patient prior to invasive treatment, with minimal morbidity.
Mirabegron is a beta-agonist that acts to facilitate bladder detrusor relaxation. Mirabegron has demonstrated sustained improvements in number of micturition and incontinence. Intolerable side effects, such as dry mouth, are statistically less compared with antimuscarinic therapy. In addition, although there are concerns regarding blood pressure rises, this remains small and Mirabegron is efficacious and safe, with no difference in treatment-emergent hypertension compared with placebo. The Medicine and Healthcare products Regulatory Agency recommends the use of Mirabegron with caution in those patients with stage 2 hypertension (systolic blood pressure ≥160 mmHg and/or diastolic ≥100 mmHg). It is contraindicated in patients with severe uncontrolled hypertension (systolic blood pressure ≥180 mmHg and/or diastolic ≥100 mmHg) [2, 9, 12, 13].
Combination therapy with 10 mg Solifenacin greatly increased its side-effect profile with only marginal benefits in efficacy. Although EAU guidelines recognize there may be more benefit from addition of Mirabegron to Solifenacin 5 mg, rather than increasing Solifenacin to 10mg, currently only the AUA recommends combination therapy in patients who are refractory to either in the treatment algorithm [6, 14, 15].
Subsequent treatment was found to be highly associated with diagnosis in both groups and had a good improving of symptoms and quality of life.
Conclusions
Urodynamics may influence the treatment decisions in determining treatment pathways in women presenting with OAB. Women treated based on UDS diagnoses appear to have greater reductions in symptoms than those who did not.
Urodynamics should be used especially for patients with known or suspected voiding phase dysfunction, those with rapidly changing symptoms, those in whom the diagnosis is not clear, those who have medical or urological histories that can affect outcomes of treatment, and in those with known or suspected neurological disease.
Abbreviations
AUA – American Urological Association; BC – bladder compliance; DO – detrusor overactivity; EAU – European Urological Association; ICI – International Consultation for Incontinence; ICIQ–OAB – International Consultation on Incontinence Questionnaire Overactive Bladder Module; ICS – International Continence Society; LUTD – lower urinary tract dysfunction; LUTS – lower urinary tract symptoms; MCC – maximum cystometric capacity; MDP – maximum detrusor pressure; NICE – National Institute for Health and Care Excellence; OAB – Overactive bladder; PdetQmax – maximum urinary flow pressure; PVR – post–void residual urine volume; Qmax – maximum urinary flow rate; UDS – urodynamic investigation; UK – United Kingdom; UUI – urgency urinary incontinence.
Competing interests
None declared
Authors' contribution
Both authors contributed equally to the development of the manuscript and approved its final version.
Authors’s ORCID ID
Mihaela Ivanov - https://orcid.org/0000-0002-5990-320X
Emil Ceban - https://orcid.org/0000-0002-1583-2884
References
Malone-lee J.G., Al-Buheissi A.S. Does urodynamic verification of overactive bladder determine treatment success? Results from a randomized placebo-controlled study. BJU International, 2009; 103(7): 931-937.
Fontaine C., Papworth E., Pascoe J., Hashim H. Update on the management of overactive bladder. Ther Adv Urol, 2021; 13: 1-9.
Gormley E., Lightner A.D., Burgio K.L., Chai T.C., Clemens J.Q., Culkin D.J., Das A.K., Foster H.E., Scarpero H.M., Tessier C.D., Vasavada S.P. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. Journal of Urology, 2012; 188(6): 2455-2463.
Lightner D.J., Gomelsky A., Souter L., Vasavada S.P. Diagnosis and Treatment of Overactive Bladder (Non-Neurogenic) in Adults: AUA/SUFU Guideline Amendment 2019. Journal of Urology, 2019; 202(3): 558-563.
Al Mousa R.T., Al Dossary N., Hashim H. The role of urodynamics in females with lower urinary tract symptoms. Arab Journal Of Urology, 2019; 17(1): 2-9.
Gormley E.A., Lightner D.J., Faraday M., Vasavada S.P. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment. Journal of Urology, 2015; 193(5): 1572-1580.
Cho., K.J., Kim H.S., Koh J.S., Kim J.C. Evaluation of female overactive bladder using urodynamics: Relationship with female voiding dysfunction. International Braz J Urol, 2015;41(4): 722-728.
Lin F.C., Nitti V.W. The Role of Urodynamic Testing Prior to Third-Line OAB Therapy. Springer. Current Bladder Dysfunction Reports, 2020; 1-7.
Kopp Kallner H., Elmér C., Altman D. Urodynamics as a Prognosticator of Mirabegron Treatment Outcomes. Gynecologic and Obstetric Investigation, 2019; 84(5): 472-476.
Abdel-Fattah M., Chapple C., Guerrero K., Dixon S., Cotterill N., Ward K., Hashim H., Monga A., Brown K., Drake M.J., Gammie A., Mostafa A., Bladder Health U.K., Breeman S., Cooper D., Maclennan G., Norrie J. Female Urgency, Trial of Urodynamics as Routine Evaluation (FUTURE study): a superiority randomized clinical trial to evaluate the effectiveness and cost-effectiveness of invasive urodynamic investigations in management of women with refractory overactive bladder symptoms. Trials, 2021; 22(1): 745.
Chen S.L., NG S.C., Huang Y.H., Chen G. Are patients with bladder oversensitivity different from those with urodynamic proven detrusor overactivity in female overactive bladder syndrome? Journal of the Chinese Medical Association, 2017; 80(10): 644-650.
Giarenis I., Mastoroudes H., Srikrishna S., Robinson D., Cardozo L. Is there a difference between women with or without detrusor overactivity complaining of symptoms of overactive bladder? B.J.U. International, 2013; 112(4): 501-507.
Diamond P., Hassonah S., Alarab M., Lovatsis D., Drutz H.P. The prevalence of detrusor overactivity amongst patients with symptoms of overactive bladder: A retrospective cohort study. International Urogynecology Journal, 2012; 23(11): 1577-1580.
Verghese T.S., Middleton L.J., Daniels J.P., Deeks J.J., Latthe P.M. The impact of urodynamics on treatment and outcomes in women with an overactive bladder: a longitudinal prospective follow-up study. International Urogynecology Journal, 2018; 29(4): 513-519.
Frenkl T.L., Railkar R., Palcza J., Scott B.B., Alon A., Green S., Schaefer W. Variability of urodynamic parameters in patients with overactive bladder. Neurourology and Urodynamics, 2011; 30(8): 1565-1569.