Introduction
CS is one of the most common abdominal surgeries performed on women in most countries. The CS rate has increased dramatically in recent decades worldwide, particularly in middle- and high-income countries, despite a lack of evidence supporting substantial maternal and perinatal benefits [1-6]. The CS rates varies significantly by geographic region, ranging from less than 10% to more than 50% at the national level, according to the World Health Organization global survey [1, 2, 7].
Multiple CSs, especially elective CSs without medical indications, are associated with short- and long-term risks for both mother and child. There are significant maternal complications, such as visceral injuries, uterine rupture, abnormal placentation, hysterectomy, hemorrhages and blood transfusions, severe adhesions, etc. Cesarean delivery (CD) is also associated with an increased incidence of perinatal complications, such as stillbirth, small-for-gestational-age neonates, and preterm birth. Children born by repeated cesarean sections are prone, in the short term, to breathing difficulties (transient tachypnea of the newborn, respiratory distress syndrome) and the need to be admitted to the neonatal intensive care unit (NICU). There are significant long-term risks associated with immune disorders, obesity, and asthma [2, 3, 5, 7, 8, 9].
The purpose of the study is to assess the fetal and perinatal outcomes of multiple CSs in pregnant women aged 18 to 40 years, as well as their incidence according to the number of cesarean sections performed.
Material and methods
The work was carried out at the Department of Obstetrics and Gynecology, Obstetrics and Gynecology Discipline of the Nicolae Testemitanu State University of Medicine and Pharmacy and the Municipal Perinatological Center of the Gheorghe Paladi Municipal Clinical Hospital. The study protocol was approved by the Research Ethics Committee of the Nicolae Testemitanu State University of Medicine and Pharmacy (minutes No. 2 of 09.06.2021).
To achieve the objective, a retrospective observational case-control study was carried out. The study included 352 pregnant women with a singleton pregnancy and at least one previous CS: 177 pregnant women with two or more previous CSs (experimental group, EG), and 175 with a primary CS (control group, CG). The women were selected in a systematic manner based on an examination of medical records from the Archives of the Gheorghe Paladi Municipal Clinical Hospital, and for greater research accuracy, a series of inclusion and exclusion criteria were followed, making the study more well defined and centered on a specific representative group.
The inclusion criteria for the study were: (1) multiparous pregnant women with at least one CS in their history and an unlimited number of vaginal births; (2) pregnant women aged 18-40 years; (3) women with segmental-transverse hysterotomies; (4) longitudinal position of the fetus; (5) singleton pregnancy; (6) pregnancy without fetal anomalies; (7) pregnancy with a gestational age greater than 35 weeks; (8) patients without serious extragenital diseases (autoimmune diseases, diabetes, cardiovascular diseases, deficiency of coagulation factors); (9) patients who were subject to all investigations according to the study protocol.
The exclusion criteria from the study were: (1) patients with previous gynecological surgery, other than CS, with penetration into the uterine cavity (myomectomy); (2) fetal macrosomia, malformations, or antepartum fetal death; (3) pregnant women over 40 years of age; (4) pregnancy with a gestational age less than 35 weeks; (5) anterior „T” or „J”-shaped hysterotomy; (6) transverse fetal position; (7) multiple pregnancies; (8) patients with severe extragenital diseases (autoimmune diseases, diabetes, cardiovascular diseases, deficiency of coagulation factors); (9) patients with uterine rupture, bleeding tendency, and infections; (10) patients with incomplete data who did not undergo all the investigations according to the study protocol.
The primary data were collected and extracted from the medical documentation (medical records), which included: socio-demographic data (age, occupation, parity, and number of pregnancies); anthropometric parameters; risk factors; medical and obstetrical-gynecological anamnesis; the results of clinical, instrumental, and laboratory investigations; the evolution of previous pregnancies and the current pregnancy; and the newborn`s status (sex, gestational age, weight, and height at birth; the Apgar scores at 1 minute and 5 minutes after birth; and birth injuries in the newborn). The indications for CS were exclusively medical. The collected data were analyzed and compared across study groups (the experimental group and the control group).
The primary study materials were entered into an electronic database and processed on a personal computer using the functions and modules of the programs „Statistical Package for the Social Science” (SPSS) version 16.0 for Windows (SPSS Inc., Belmont, CA, USA, 2008) and Microsoft Excel 2019 through descriptive and inferential statistical procedures. To compare discrete variables, methods such as Pearson's χ², Yates' χ² correction, or Fisher's exact test were used; to determine the statistical difference in mean values between groups, an independent samples t-test (for interval-scaled variables with a normal distribution of values) or non-parametric statistical tests (for ordinal-scaled or interval-scaled variables with a non-normal distribution of values) were used.
Differences that were statistically significant with a bilateral value of p < 0.05 were considered.
Results and discussions
The mean age of pregnant women in the EG was statistically significantly higher as compared to patients in the CG (30.56±0.3 years and 29.31±0.4 years, respectively; p < 0.05). In the CG, there were statistically significantly more women aged between 31 and 40 years (51.4% and 38.3%, respectively; p < 0.05), and in the CG, there were statistically significantly more women aged 18-20 years (3.4% and 0.6%, respectively; p < 0.05). The proportion of women aged 21-30 years was similar in both study groups (48.0% and 58.3%, respectively; p > 0.05). Rehman et al., in a recent study, confirmed that most women who underwent CS were aged 21-30 years (67.1%) [10].
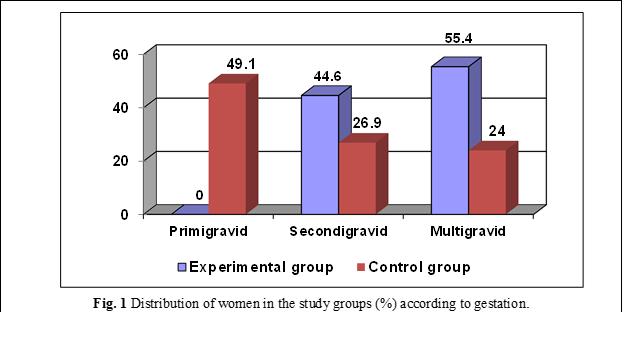
In the study, primigravid women were statistically significantly more prevalent in the CG 85 cases (49.1%, p < 0.001), whereas secundigravid women (79 – 44.6% and 48 – 26.9%, respectively; p < 0.001) and multigravida women (98 – 55.4% and 42 – 24.0%, respectively; p < 0.001) were statistically significantly more prevalent in the EG (Figure 1).
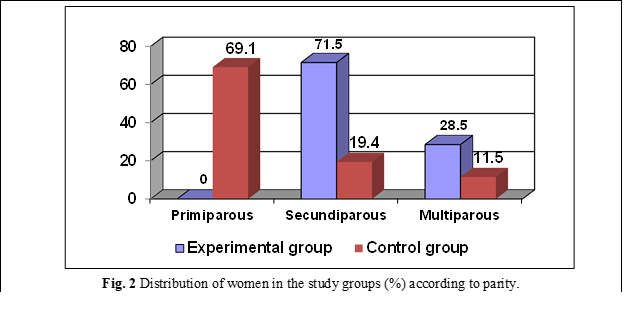
According to parity, primiparous women accounted for 121 cases (69.1%, p < 0.001) significantly predominating in the CG, while secundiparous women accounted for 126 cases (71.5%) and 34 cases (19.4%), respectively, and multiparous women accounted for 51 cases (28.5%) and 20 cases (11.5%), respectively (p < 0.001), significantly predominating in the EG (Figure 2).
Similar results were obtained in other studies. Blotniene et al. [1] found that women with two or more CSs had statistically significantly higher mean ages at birth, gestations, and parities than women with a primary CS in a study of 655 pregnant women with at least one CS and singleton pregnancies [1].
Maternal morbidity increases exponentially with the number of CSs. The risk of injury in infants is low but not absent. A high rate of elective CDs has contributed to the increase of fetal complications: respiratory morbidity (respiratory distress syndrome, transient tachypnea of the newborn), admission to the NICU, and increased length of hospitalization, with a significant medical, social, and financial impact on families and medical institutions [7, 11-15]. The adverse risks of CD at 37-38 weeks of gestation significantly increase, with a magnitude of 9–40% [15].
An increased risk of severe general respiratory morbidity has been identified in infants born by elective CS. Furthermore, the risk increased concurrently with the gestational age decrease: at 37 weeks (odds ratio: OR 3.9; 95% confidence interval: CI 2.4-6.5); at 38 weeks (OR 3.0; 95% CI 2.1-4.3); and at 39 weeks (OR 1.9; 95% CI 1.2-3.0). The risk of severe respiratory morbidity was more likely at 37 (OR 5.0; 95% CI 1.6-16.0) and 38 weeks of gestation (OR 4.2; 95% CI 1.6-11.0). Even after excluding pregnancies complicated by diabetes, preeclampsia, intrauterine fetal growth retardation, or breech presentation, the results remained consistent [14].
The lack of stress hormones associated with labor could explain this association. During spontaneous labor, fetal lung fluid secretion decreases and absorption increases, and stimulation of surfactant release may be mediated by elevated fetal catecholamines in response to rupture of the membranes and delivery. Thus, if CS is performed before the onset of labor, the concentration of catecholamines in the serum does not increase [11, 13, 14]. Studies have found that full-term neonates born via elective CS have significantly lower catecholamine levels and changes in lung function than those born vaginally [14].
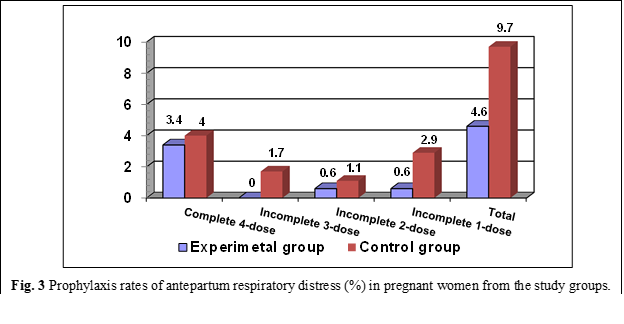
In the cohort study, the rate of antepartum respiratory distress prophylaxis was similar in both study groups, both overall (4.6% in the EG and 9.7% in the CG, respectively; p > 0.05) and by method: complete prophylaxis with 4 doses (3.4% in the EG and 4.0% in the CG, respectively; p > 0.05), incomplete prophylaxis with 3 doses (0% in the EG and 1.7% in the CG, respectively), incomplete 2-dose prophylaxis (0.6% in the EG and 1.1% in the CG, respectively; p > 0.05) and incomplete 1-dose prophylaxis (0.6% in the EG and 2.9% in the CG, respectively; p > 0.05) (Figure 3). According to literature data, women with two or more previous CDs were scheduled for CS between 37 and 38 weeks of gestation. This tactic aims to reduce the risk of uterine rupture associated with spontaneous labor in women with post-cesarean scars [1, 16, 17]. In general, the gestational age of the fetus at birth is lower in pregnant women with multiple CSs. The higher the number of previous CDs, the higher the chances of a preterm birth during the next CS [1].
The newborns delivered by women with a previous CS were associated with a significantly increased risk of NICU admission (adjusted OR 1.31; 95% CI 1.23, 1.39; p < 0.001), neonatal loss (adjusted OR 1.19; 95% CI 1.12, 1.26; p< 0.001) and preterm birth (adjusted OR 1.07; 95% CI 1.01, 1.14; p < 0.05) [7].
A retrospective cohort study conducted on 672 singleton pregnant women without congenital anomalies (343 women delivered by planned repeat cesarean sections and 329 women delivered per vias naturalis) examined newborn data. Newborns delivered by repeat CS without labor had higher rates of NICU admission, primarily for hypoglycemia, compared to the group of newborns delivered vaginally (9.3% and 4.9%, respectively; p = 0.025), higher rates of oxygen supplementation for resuscitation in the delivery room (41.5% and 23.2%, respectively; p < 0.01) and in the NICU (5.8% and 2.4%, respectively; p <0.028). Neonates born by elective repeat CS without labor demonstrated significantly higher rates of NICU admission [13].
In the study, the termination of the current pregnancy by CS in the general study group according to gestational age was as follows: 5.4% at 35 + 0 – 36 + 6 weeks of gestation, 7.4% at 3 7 + 0 – 37 + 6 weeks of gestation, 17.6% at 38 + 0 – 38 + 6 weeks of gestation, 42.0% at 39 + 0 – 39 + 6 weeks of gestation, 18.5% at 40 + 0 – 40 + 6 weeks of gestation, and 9.1% at ≥41 weeks of gestation.
This indicator was almost similar in both study groups: at 35 + 0 – 36 + 6 weeks of gestation (4.5% in the EG and 6.3% in the CG, respectively; p > 0.05), at 37 + 0 – 37 + 6 weeks of gestation (5.6% in the EG and 9.1% in the CG, respectively; p > 0.05) and at 39 + 0 – 39 + 6 weeks of gestation (21.5% in the EG and 13.7% in the CG, respectively; p > 0.05). In the EG, the termination rate of the current pregnancy by CS was statistically significantly higher at 39 + 0 – 39 + 6 weeks of gestation (56.5% and 27.4%, respectively; p < 0.001), and in the CG, it was statistically significantly higher at 40 + 0 – 40 + 6 weeks of gestation (25.7% and 11.3%, respectively; p < 0.001) and at 41 weeks of gestation or more (17.7% and 0.6%, respectively; p < 0.001) (figure 4).
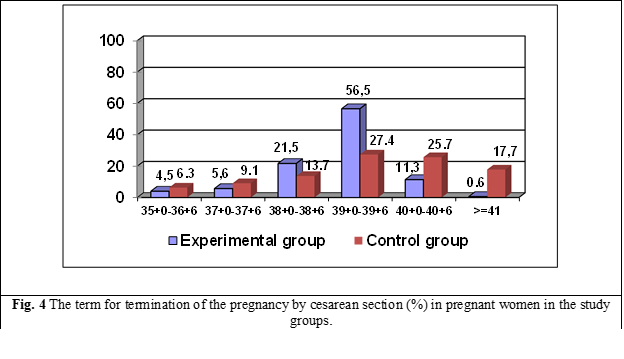
Thus, in the CG, there is a tendency to increase CD at the gestational age of 37 + 0 – 37 + 6 weeks, and in the EG, there is a tendency to increase CD at 38 + 0 – 38 + 6 and 39 + 0 – 39 + 6 weeks of gestation. The medical indications for more severe CS in women with primary CS may explain these findings. Evaluation of medical indications for CS in pregnant women in the study revealed that uterine scarring (57.6% and 0%, respectively; p < 0.001), suspected uterine scar defect (16.9% and 0%, respectively; p < 0.001) and the onset of labor (23.2% and 2.3%, respectively; p < 0.001) were statistically significantly more common in the EG.
The most common indications for CS in the CG were as follows: premature detachment of normally inserted placenta (5.1% and 0.6%, respectively; p < 0.05), pelvic presentation (25.1% and 5.6%, respectively; p < 0.001), post-term pregnancy (2.9% and 0%, respectively; p < 0.05), clinically narrow pelvis (7.4% and 0%, respectively; p < 0.001), primary dynamic uterine dystocia (12.0% and 1.7%, respectively; p< 0.001), secondary dynamic uterine dystocia (9.1% and 0%, respectively; p < 0.001), acute fetal distress during labor (12.0% and 0 .6%, respectively; p < 0.001), failure to induce labor with prostaglandins (10.3% and 0%, respectively; p <0.001), extragenital diseases (7.4% and 1.7%, respectively; p <0.05), complicated obstetric history (in vitro fertilization) (9.1% and 1.1%, respectively; p < 0.01), severe preeclampsia (4.6% and 0%, respectively; p < 0.01) and other indications (10.9% and 0.6%, respectively; p < 0.001) (table 1). In some cases, several medical indications for CS persisted in the same pregnant woman.
Table 1. Medical indications for cesarean section in pregnant women in the study groups | |||||
Parameter | EG | CG | P | ||
abs. | % | abs. | % | ||
Uterine scarring (planned) | 102 | 57.6 | 0 | 0 | < 0.001 |
Suspected uterine scar defect | 30 | 16.9 | 0 | 0 | < 0.001 |
Premature detachment of the normally inserted placenta | 1 | 0.6 | 9 | 5.1 | < 0.05 |
Placenta previa | 3 | 1.7 | 4 | 2.3 | NS |
Pelvic presentation | 10 | 5.6 | 44 | 25.1 | < 0.001 |
Abnormal fetal position | 1 | 0.6 | 1 | 0.6 | NS |
Post-term pregnancy | 0 | 0 | 5 | 2.9 | < 0.05 |
Clinically narrow pelvis | 0 | 0 | 13 | 7.4 | < 0.001 |
Anatomically narrow pelvis | 3 | 1.7 | 5 | 2.9 | NS |
Dynamic uterine dystocia (primary) | 3 | 1.7 | 21 | 12.0 | < 0.001 |
Dynamic uterine dystocia (secondary) | 0 | 0 | 16 | 9.1 | < 0.001 |
Acute fetal distress during labor | 1 | 0.6 | 21 | 12.0 | < 0.001 |
Intrauterine growth retardation of the fetus | 3 | 1.7 | 8 | 4.6 | NS |
Premature rupture of the amniotic sac | 25 | 14.1 | 29 | 16.6 | NS |
Failure to induce labor with prostaglandins | 0 | 0 | 18 | 10.3 | < 0.001 |
Transverse situs | 1 | 0.6 | 0 | 0 | NS |
Extragenital disease | 3 | 1.7 | 13 | 7.4 | < 0.05 |
Complicated obstetric history (in vitro fertilization) | 2 | 1.1 | 16 | 9.1 | < 0.01 |
Isthmic-cervical insufficiency (cervical cerclage) | 0 | 0 | 1 | 0.6 | NS |
Severe preeclampsia | 0 | 0 | 8 | 4.6 | < 0.01 |
Obstetric suction ventouse (cupping) failure | 0 | 0 | 1 | 0.6 | NS |
Deflected presentation | 1 | 0.6 | 3 | 1.7 | NS |
Onset of labor | 41 | 23.2 | 4 | 2.3 | < 0.001 |
Other | 1 | 0.6 | 19 | 10.9 | < 0.001 |
Note: EG – experimental group, CG – control group, NS – statistically insignificant relationship, P – probability. | |||||
A previous CS is the most common indication for the next CS. A cross-sectional retrospective study performed on a group of 602 women with CD found that repeat CS (48.5%), followed by fetal distress (18.9%), oligohydramnios (6.6%), cephalopelvic disproportion (6.5%), failure of labor (5.6%) and malpresentation (3.8%) were the most common major indications for CS [10].
A previous CS is associated with a higher risk of preterm birth in subsequent pregnancies, which is due to an increased risk of subsequent preterm births through unplanned or emergency CS. The risk of preterm birth among women with an unplanned CS after a previous CS increased 5-fold (adjusted OR 5.53; 95% CI 5.25–5.83), compared to women with a planned CS or vaginal delivery [18].
A recent study conducted on a group of 100 women with a singleton pregnancy and a previous CS found that in 74% of cases repeat CS (elective or emergency) was performed at a fetal gestational age of 37 + 0 – 37 + 6 weeks; in 18% of cases, the gestational age of the fetus was 38 + 0 – 38 + 6 weeks. CS was not performed on pregnant women whose fetus had a gestational age greater than 40 weeks. Scholars have noted that elective CS is most commonly performed 2 weeks before the expected date of birth [5]. CSs performed before 39 weeks of gestation may increase the newborn's risk of respiratory disorders and hypoglycemia [9].
There are many reasons to perform a CS. Most CSs are performed for maternal or fetal medical reasons; however, there has been an increase in the number of women requesting a CS without a medical indication [4, 11]. The literature shows that the main indications for CS (about 85% of cases) are previous CD (42.8%), failure to progress during labor, suspected fetal distress (15.5%), fetal malpresentation, and dystocia. In addition, the NICU admission rate is higher in emergency CS cases (fetal distress, neonatal sepsis) [1, 4, 11, 12].
Although emergency CSs are intended to reduce maternal and neonatal mortality and morbidity, CD can be associated with negative short-term and long-term consequences [11]. In the study, the analysis of deliveries revealed that emergency CS in pregnancy (33 - 18.9% and 16 - 9.0%, respectively; p <0.01) and emergency CS during labor (106 - 60.6% and 54 - 30.5%, respectively; p < 0.001) were performed statistically significantly more frequently in the CG, while planned CS during pregnancy (107 – 60.5% and 36 – 20.6%, respectively; p < 0.001) was performed significantly more frequently in the EG (figure 5).
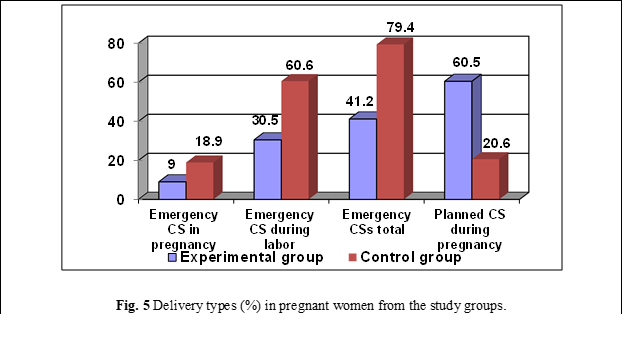
These results are similar to those of a recent study, in which 63.6% of cases were emergency CSs and only 36.4% of cases were planned CSs [10].
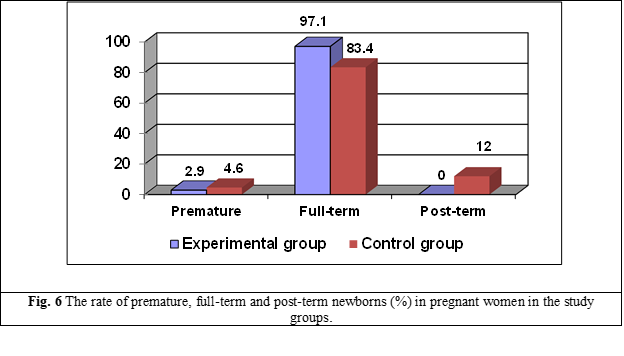
In the study, the rate of full-term neonates was statistically significantly higher in the EG (171 – 97.1% and 146 – 83.4%, respectively; p < 0.001), the rate of post-term neonates was statistically significantly higher in women from the CG (21 – 12.0%; p < 0.001), and the rate of premature newborns was similar in both study groups (6 – 2.9% in the EG and 8 – 4.6% in the CG, respectively; p > 0.05) (figure 6).
The newborns in both study groups did not differ in terms of sex, mass, and length. 90 (50.8%) newborns in the EG and 80 (45.7%) newborns in the CG (p > 0.05) were female; 87 (49.2%) newborns in the EG and 95 (54.3%) newborns in the CG (p > 0.05) were male.
The average mass of the newborns was 3435.37±29.8 g in the EG and 3431.6±38.1 g in the CG (p > 0.05), and the average length of the newborns was 52.19±0.1 cm and 52.25±0.2 cm, respectively (p > 0.05). Similar results have been reported in other studies. In women with a CS, the average mass of the newborn was 3467.40±752.51 g, and the average length of the newborn was 51.88±4.21 cm. In women with 2, 3, 4, and more CSs, these parameters were as follows: 3384.42±730.29 g and 51.09±4.18 cm, 3276.66±833.60 g and 50.20±5.86 cm, 3095.71±726.66 g and 50.00±3.92 cm (p > 0.05) [1].
The study groups were similar (p > 0.05) and according to different groups of mass and length of newborns: 1 (0.6%) newborn from the EG and 4 (2.3%) newborns from the CG had a body mass between 1000-1999 g, 22 (12.4%) newborns from the EG and 24 (13.7%) newborns from the CG had a body mass between 2000-2999 g, 154 (87.0%) newborns in the EG and 147 (84.0%) newborns in the CG had a body mass range of 3000-3999 g, 3 (1.7%) newborns in the EG and 6 (3.4%) newborns from the CG had a body length between 44-46 cm, 24 (13.6%) newborns from the EG and 30 (17.1%) newborns from the CG had a body length between 47-50 cm, 150 (84.7%) newborns from the EG and 139 (79.4%) newborns from the CG had a body length > 50 cm.
The mean values of the weight and length of the newborns were also similar according to the number of previous CSs: 3431.60±38.1 g in women with 1 CS, 3412.43±33.6 g in women with 2 CSs and 3522.16±63.8 g in women with 3-4 CSs (p <0.05), 52.25±0.2 cm in women with 1 CS, 52.18±0.2 cm in women with 2 CSs and 52.22±0.4 cm in women with 3-4 CSs (p< 0.05).
The frequency of children with low body mass (≤2500 g) had an increasing tendency in the CG (10 – 5.7% and 4 – 2.3%, respectively; p > 0.05), but this difference did not reach any statistical certainty.
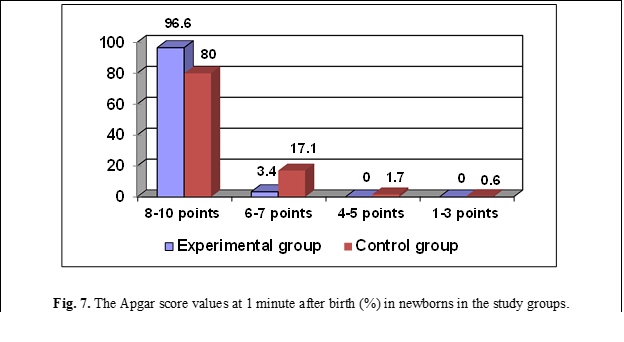
The Apgar score values at 1 minute after birth equal to 8-10 points (171 – 96.6% and 140 – 80.0%, respectively; p < 0.001) were statistically significantly more frequent in the EG, the Apgar score values at 1 minute after birth equal to 6-7 points (29 – 17.1% and 6 – 3.4%, respectively; p < 0.001) and 4-5 points (5 – 1.7% and 0 – 0%, respectively; p< 0.05) were statistically significantly more frequent in the CG; and the Apgar score values 1 minute after birth equal to 1-3 points (0 – 0% in the EG and 1 – 0.6% in the CG; p > 0 .05) were similar in both study groups (figure 7).
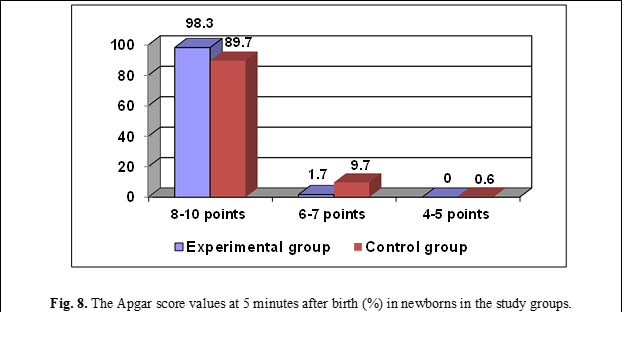
The Apgar score values at 5 minutes after birth equal to 8-10 points (174 – 98.3% and 157 – 89.7%, respectively; p < 0.001) were statistically significantly more frequent in the EG; the Apgar score values at 5 minutes after birth equal to 6-7 points (17 – 9.7% and 3 – 1.7%, respectively; p < 0.01) were statistically significantly more frequent in the CG; and the Apgar score values at 5 minutes after birth equal to 4-5 points (0 – 0% in the EG and 1 – 0.6% in the CG; p > 0.05) were similar in both study groups (figure 8).
Analysis of the Apgar score at 1 minute and 5 minutes after birth according to the presence or absence of acute fetal distress during labor in pregnant women in the CG found that the Apgar score values 1 minute after birth equal to 8-10 points (130 – 84.4% and 10 – 47.6%, respectively; p < 0.001) were statistically significantly more frequent in pregnant women without acute fetal distress during labor, and the Apgar score values 1 minute after birth equal to 1-7 points (11 – 52.4% and 24 – 15.6%, respectively; p < 0.001) were statistically significantly more frequent in pregnant women with acute fetal distress during labor.
Similar results were found in the Apgar score at 5 minutes after birth. The Apgar score values 5 minutes after birth equal to 8-10 points (142 – 92.2% and 15 – 71.4%, respectively; p < 0.05) were statistically significantly more frequent in pregnant women without acute fetal distress during labor, and the Apgar score values 5 minutes after birth equal to 1-7 points (6 – 28.6% and 12 – 7.8%, respectively; p < 0.05) were statistically significantly more frequent in pregnant women with acute fetal distress during labor.
Some studies did not identify significant increased risks of stillbirth, early neonatal death, perinatal death, low Apgar score, and low birth weight between women with and without prior CSs [7]. A recent study, carried out on a group of 655 pregnant women with at least one CS and with singleton pregnancies, found no significant differences in the mean values of the Apgar score at 1 minute and 5 minutes after birth according to the number of CSs: 9.01±1.07 points and 9.65±0.68 points in women with primary CS, 9.05±1.11 points and 9.60±0.84 points in women with 2 previous Cs, 8.60±2.03 points and 9.20±1.86 points in women with 3 previous CSs, 9.14±0.69 points and 9.43±0.53 points in women with 4 or more previous CSs [1].
A systematic literature review revealed a statistically significant difference in the Apgar score <5 points at 5 minutes after birth between the group of women with 1 CS and the groups of women with 2 CSs (9.39% and 2.11%, respectively; p < 0.001), 3 CSs (9.39% and 2.18%, respectively; p < 0.001), 4 and more CSs (9.39% and 4.49%, respectively; p < 0.01) [2].
The evaluation of some parameters according to the delivery type found that in pregnant women with emergency CSs, an increased number of newborns with low body mass (≤2500 g) was determined (10 – 4.8% and 4 – 2.8%, respectively; p > 0.05), an increased Apgar score rate equal to 1-7 points at 5 minutes after birth (16 – 7.7% and 5 – 3.5%, respectively; p > 0.05) and a statistically significant increase in the rate of the Apgar score equal to 1-7 points at 1 minute after birth (35 – 16.7% and 6 – 4.2%, respectively; p <0.001).
The discharge rate of neonates in the study was higher in the EG (165 – 93.2% and 136 – 77.7%, respectively; p < 0.001), and the transfer rate to stage II was higher in the CG (39 – 22.3% and 12 – 6.8%, respectively; p <0.001). The frequency of neonatal trauma (scalpel injury) was low and similar in both study groups: 0 (0%) in the EG and 3 (1.7%) in the CG (p > 0.05).
In general, the literature suggests that the mode and timing of delivery have a greater impact on adverse neonatal outcomes than the number of previous CSs [2].
Conclusions
The termination of the pregnancy by CS at 39 + 0 – 39 + 6 weeks of gestation (56.5% and 27.4%, respectively; p <0.001) was statistically significantly more frequent in the EG, and at 40 + 0 – 40 + 6 weeks of gestation (25.7% and 11.3%, respectively; p <0.001) and at 41 weeks of gestation or more (17.7% and 0.6%, respectively; p < 0.001) was statistically significantly more common in the CG.
Analysis of deliveries revealed that emergency CS in pregnancy (18.9% and 9.0%, respectively; p < 0.01) and emergency CS during labor (60.6% and 30.5%, respectively; p < 0.001) were significantly statistically more frequent in the CG, and planned CS in pregnancy (60.5% and 20.6%, respectively; p< 0.001) was statistically significantly more frequent in the EG.
The rate of full-term neonates was statistically significantly higher in women from the EG (97.1% and 83.4%, respectively; p < 0.001), and the rate of post-term neonates was statistically significantly higher in women from the CG (12.0% and 0%, respectively; p < 0.001).
Neonates in both study groups were similar in terms of sex, mass, and length. However, the Apgar score values equal to 8-10 points at 1 minute after birth (96.6% and 80.0%, respectively; p <0.001) and at 5 minutes after birth (98.3% and 89.7%, respectively; p <0.001) were statistically significantly more frequent in the EG; the Apgar score values equal to 6-7 points at 1 minute after birth (17.1% and 3.4%, respectively; p < 0.001) and at 5 minutes after birth (9.7% and 1.7%, respectively; p < 0.01) and the Apgar score values equal to 4-5 points at 1 minute after birth (1.7% and 0%, respectively; p <0.05) were statistically significantly more frequent in the CG.
Abbreviations
CD – cesarean delivery; CDs – cesarean deliveries; CI – confidence interval; CS – cesarean section; CSs – cesarean sections; CG – control group; EG – experimental group; NICU – neonatal intensive care unit; OR – odds ratio; SPSS – Statistical Package for the Social Science.
Competing interests
None declared
Authors’s ORCID ID
Oleg Potacevschi - https://orcid.org/0000-0001-9934-031X
References
Blotnienė P, Žitkutė V, Volochovič J, Domža G. Multiple repeat cesarean sections – incidence and consequences: a review of 3 years in a tertiary hospital experience. J Med Sciences. 2019 Oct 31; 7(12): 1-8. ISSN: 2345-0592
Zwergel C, Kaisenberg C. Maternal and Fetal Risks in Higher Multiple Cesarean Deliveries. In: Recent Advances in Cesarean Delivery (ed. Georg Schmolzer). London: IntechOpen, 2020. doi: 10.5772/intechopen.86334
Lyell DJ. Adhesions and perioperative complications of repeat cesarean delivery. Am J Obstet Gynecol. 2011 Dec; 205(6 Suppl): S11-8. doi: 10.1016/j.ajog.2011.09.029
Gee M, Dempsey A, Myers J. Caesarean section: techniques and complications. Obstet Gynaecol Reprod Med. 2020; 30: 4. doi: 10.1016/j.ogrm.2020.02.004
Ganiga P, Rudrappa S. A prospective study of maternal and fetal outcome in repeat LSCS mother. Int J Reprod Contracept Obstet Gynecol. 2019; 8(4): 1327-1330. doi: https://dx.doi.org/10.18203/2320-1770.ijrcog20190979
Venturella R, Quaresima P, Micieli M, Rania E, Palumbo A, Visconti F. et al. Non-obstetrical indications for cesarean section: a state-of-the-art review. Arch Gynecol Obstet. 2018 Jul; 298(1):9-16. doi: 10.1007/s00404-018-4742-4.
Kietpeerakool C, Lumbiganon P, Laopaiboon M, Rattanakanokchai S, Vogel J, Gülmezoglu A. Pregnancy outcomes of women with previous caesarean sections: Secondary analysis of World Health Organization Multicountry Survey on Maternal and Newborn Health. Sci Rep. 2019; 9(1): 9748. doi: 10.1038/s41598-019-46153-4
Clark EA, Silver RM. Long-term maternal morbidity associated with repeat cesarean delivery. Am J Obstet Gynecol. 2011 Dec;205(6 Suppl): S2-10. doi: 10.1016/j.ajog.2011.09.028.
Sandall J, Tribe R, Avery L, Mola G, Visser G, Homer C. et al. Short-term and long-term effects of caesarean section on the health of women and children. Lancet. 2018 Oct 13;392(10155):1349-1357. doi: 10.1016/S0140-6736(18)31930-5.
Rehman B, Gul H. Indication and complication of caesarean section at tertiary care hospital: a retrospective study. Int J Reprod Contracept Obstet Gynecol. 2019; 8(4): 1646-1649. doi: 10.18203/2320-1770.ijrcog20191235
Khasawneh W, Obeidat N, Yusef D, Alsulaiman J. The impact of cesarean section on neonatal outcomes at a university-based tertiary hospital in Jordan. BMC Pregnancy Childbirth. 2020 Jun 1;20(1):335. doi: 10.1186/s12884-020-03027-2
Vishwakarma K, Yadav G, Waddar P. Maternal and perinatal outcomes of delivery after previous one or two cesarean section. Indian J Obstet Gynecol Res. 2020 Sept; 7(3): 308-314. doi: 10.18231/j.ijogr.2020.067
Kamath B, Todd J, Glazner J, Lezotte D, Lynch A. Neonatal outcomes after elective cesarean delivery. Obstet Gynecol. 2009 Jun;113(6):1231-1238. doi: 10.1097/AOG.0b013e3181a66d57
Hansen A, Wisborg K, Uldbjerg N, Henriksen T. Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. BMJ. 2008; 336: 85-91. doi: https://doi.org/10.1136/bmj.39405.539282.BE
Salemi JL. Elective Early Term Delivery and Adverse Infant Outcomes in a Population-Based Multiethnic Cohort. In: Dissertation. University of South Florida, 2014. 211 p. https://scholarcommons.usf.edu/etd
Nisenblat V, Barak S, Griness O, Degani S, Ohel G, Gonen R. Maternal complications associated with multiple cesarean deliveries. Obstet Gynecol. 2006 Jul;108(1):21-6. doi: 10.1097/01.AOG.0000222380.11069.11
Osman S, Farid G, Kamal R, Ali S, Swaraldahab M. Perinatal Morbidity & Mortality following repeat Cesarean section due to five or more previous Cesarean Section done in Tertiary centre in KSA. Clin J Obstet Gynecol. 2018; 1: 045-051. doi: 10.29328/journal.cjog.1001007
Yasseen A, Bassil K, Sprague A, Urquia M, Maguire J. Late preterm birth and previous cesarean section: a population-based cohort study. J Matern Fetal Neonatal Med. 2019 Jul;32(14):2400-2407. doi: 10.1080/14767058.2018.1438397