Introduction
The deontological code of the pharmacist states: ”In his or her activity, the pharmacist must respect the honor and dignity of the patient, with the obligation to assist all patients visiting the community pharmacy equally and to correctly inform them about the requested medications” [1]. Effective communication between the patient and the pharmacist, as well as with other healthcare professionals, is important for enabling patients to make informed decisions regarding their medication and to ensuring the rational use of medications. This principle is regulated by the Good Pharmacy Practice Rules [2] and is part of the continuous evolution of the pharmacist's role in the healthcare system. Communication is an extremely complex field that involves not only the transmission of content but also interpersonal relationships and social processes. Researching the principles of communication in pharmaceutical practice allows for improving and ensuring the quality of pharmaceutical services provided in community pharmacies and other patient care settings [3]. Effective communication is one of the professional standards of the pharmacist, promoted by various international organizations in the field [4-8], which contribute to improving the health, safety, and well-being of patients. Interpersonal communication skills are considered so important that they are an essential component in educational programs/curricula developed by the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties [9].
According to the General Pharmaceutical Council, „Communication can take many forms and manifest in different ways. Effective communication is essential for providing person-centered care and collaborating with others. It helps people to be involved in decisions related to their health, safety, and well-being. Communication means more than just providing information, asking questions, and listening. It involves the exchange of information between people. Body language, tone of voice, and the words used by pharmaceutical professionals all contribute to effective communication.” [8].
Effective communication in the community pharmacy requires each interaction to include a clear and concise message from the pharmacist, as well as a patient who can understand and interpret that message. The patient also provides feedback to the pharmacist in response to the received message [10].
Effective verbal communication is defined as the exchange of information using words understood by the receiver, in a way that conveys professional care and respect [11]. In addition to verbal communication, the pharmacist must also be aware of the messages conveyed through non-verbal communication, which can have a significant impact on the communication experience and can sometimes be more powerful than the verbal message itself. Adhering to principles and rules–such as demonstrating appropriate verbal, non-verbal, and paraverbal communication, practicing assertive communication, respecting personal space, and overcoming communication barriers–will contribute to effective communication with the patient in the community pharmacy [12, 13].
Nowadays, the notion of therapeutic communication is increasingly used. It involves the interpersonal transmission of information through words and behaviors, based on the knowledge, attitudes, and professional skills of the healthcare specialist, aimed at facilitating the patient's understanding and participation in making decisions about their health. Therapeutic communication techniques are specific methods used to provide patients with support and information, focusing on their concerns [14]. Applying therapeutic communication techniques for the pharmaceutical setting would enhance the image of the pharmacist as a medication specialist. Pharmacists can support patients in using medication–especially in outpatient settings–according to their needs, values, abilities, and specific characteristics. Depending on the patient category and their needs, appropriate terminology should be used to promote understanding and build a relationship of trust.
Lack of communication or ineffective communication is the most common cause of medication errors reported at all three levels: prescribing, dispensing, and administration [15, 16]. To minimize the impact of ineffective communication and ensure a correct and efficient communication process, healthcare providers can rely on the Guide on the Application of the Procedure for Patient Communication and Counseling, approved by the Order No. 425 of the Ministry of Health, Labor and Social Protection of the Republic of Moldova, dated March 20, 2018. This guide represents a valuable resource for professionals seeking to develop their patient counseling skills through the use of the described techniques and tools [17].
The study conducted by Stela Adauji (2023) highlights that „pharmacists possess verbal communication skills and are involved in the patient counseling process when dispensing medications, including those on the Rx list, through various methods. They also have the appropriate knowledge and skills to determine and assess the health problems of patients in the case of self-medication and can be involved in monitoring these processes.” [18]. The pharmaceutical care provided by pharmacists varies across different patient categories and depends on several factors, with age being one of the most significant. The characteristics of elderly individuals as medication consumers underscore the need for specialized pharmaceutical care [19, 20], especially through the lens of therapeutic communication in the community pharmacy, considering that pharmacists have previously viewed elderly patients as only partially communicative and unlikely to seek additional information [21].
In this context, the aim of the study was to highlight the principles and general rules adapted to support effective communication tailored to the needs of elderly individuals as beneficiaries of specialized pharmaceutical care and to ensure the quality of pharmaceutical services provided to them in the community pharmacy. Highlighting communication principles will provide support pharmacists in creating a favorable environment during counseling sessions with elderly and in meeting their needs and expectations.
Material and methods
The research conducted was descriptive in nature, with the research instrument being a questionnaire that included 8 closed-ended questions addressing aspects of information exchange between pharmacists and elderly patients during medication dispensing. The study involved a survey of 406 respondents, with the representative sample size calculated using Cochran's formula based on the following data: the number of pharmacists in 2023 according to the National Bureau of Statistics (BNS) – 1873, confidence level – 1.96, margin of error – 0.05, and estimated population proportion – 0.5. Thus, the corrected sample size for a population of 1873 pharmacists was approximately 319. Statistical analysis included the calculation of the confidence interval using Excel software. The methodological framework for analysis and the development of recommendations was based on the provisions of the Deontological Code of Pharmacists of the Republic of Moldova, the Good Pharmacy Practice Rules, the Deontological Code of Medical and Pharmaceutical Workers, and the Guide on the Application of the Procedure for Patient Communication and Counselling.
Results and discussions
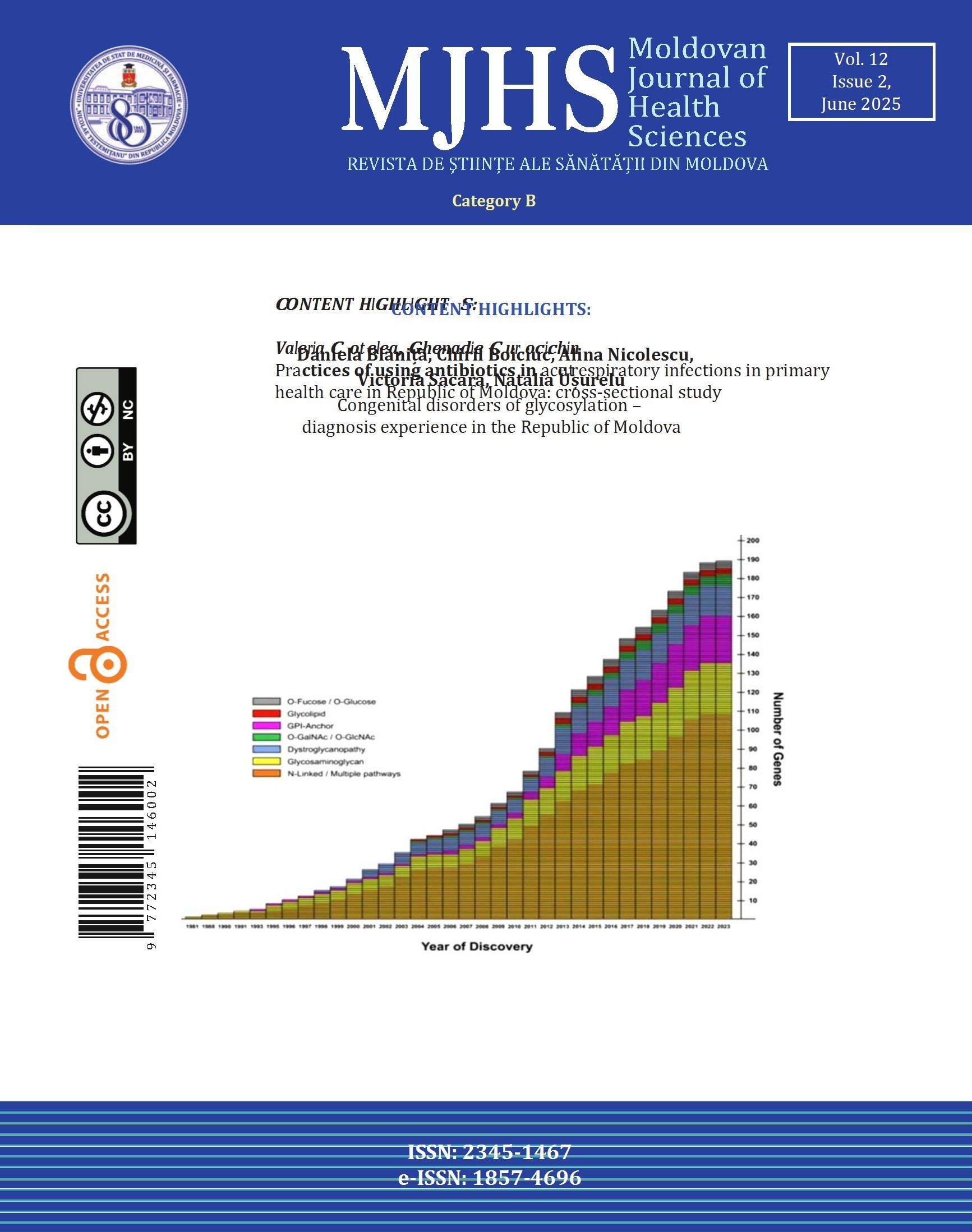
The majority of pharmacist respondents identified doctors' or nurses' recommendations as the main sources about medications (81.5%, 95% CI: 77.75-85.30), followed by pharmacists' recommendations (70%, 95% CI: 65.49-74.41) (Fig. 1). Professional differences, as well as their place in the healthcare system, highlight the importance of each specialist in promoting the rational use of medication. They ensure that the recommended medication is appropriate for the patient and the condition they are suffering from. On the one hand, the fact that specialists remain the main source for choosing the elderly patient's medication contributes to reducing and avoiding many problems related to medication management. On the other hand, the fact that other sources of medication choice include medication advertising provided through various means (77.6%, 95% CI: 71.52-81.64), advice from others (66.5%, 95% CI: 61.91-71.09), family members' experiences (60.8%, 95% CI: 56.08-65.58), or television shows (56.2%, 95% CI: 51.33-60.98) highlights the need for effective communication between the specialist and the elderly patient. This ensures an objective level of information about medications and limits the influence of aggressive medication promotion. The concept of rational use of medications is a priority in the pharmaceutical system, and communication is the primary tool for promoting it.
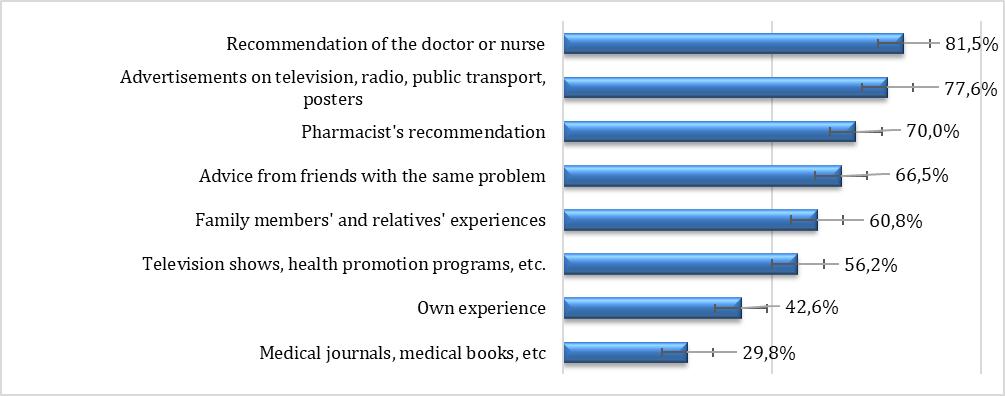 |
Fig. 1 The sources from which elderly patients gather information influencing their choice of medications. Each source is represented as a percentage of the total responses. The data highlight the most to least influential sources: Medical journals, books, etc. (29.8%); Own experience (42.6%); Television shows and health promotion programs (56.2%); Family members’ and relatives’ experiences (60.8%); Advice from friends with similar conditions (66.5%); Pharmacist’s recommendation (70.0%); Advertisements on television, radio, public transport, posters (77.6%); Recommendation of the doctor or nurse (81.5%). |
In the case of the elderly, their ability to manage their own medications is influenced by the severity of their illness or illnesses and the treatment regimens, which are often complicated, thereby increasing the risk of medication misuse. Specialized pharmaceutical care, in this sense, aims to reduce the burden of polypharmacy typical among the elderly by counseling and helping them understand how, when, and why to administer medication. Clear and accessible communication in this regard is indispensable. In their interactions with the elderly, pharmacists provide the informational support that the latter need, taking into account the vulnerability of elderly patients and their specific needs. The needs of the elderly are often determined by the deficiencies that arise with aging, such as memory loss, decreased visual and auditory acuity, decreased muscle strength and mobility, etc. For the communication process, these become barriers that the pharmacist must recognize and accommodate by adapting the information exchange to each individual patient.
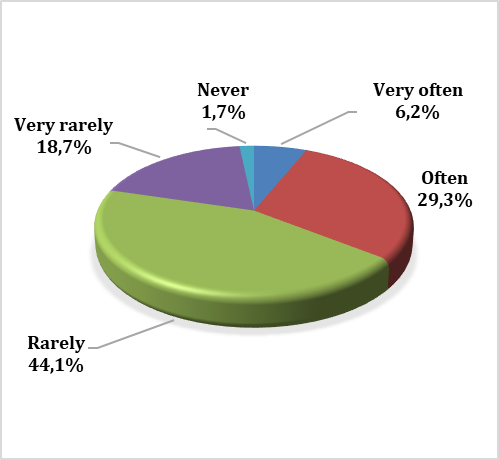 |
Fig. 2 Communication barriers experienced during counseling sessions with elderly patients. Each category reflects the percentage of respondents who identified the respective frequency of these barriers: Very often: 6.2%; Often: 29.3%; Rarely: 44.1%; Very rarely: 18.7%; Never: 1.7%. |
 |
Fig. 3 Frequency of erroneous information elderly individuals had about requested medications Each frequency category is represented as follows: Very often: 9.1%; Often: 47.3%; Rarely: 35.2%; Very rarely: 6.4%; Never: 1.7%. |
Thus, the majority of respondents, 44.1% (95% CI: 39.25-48.91), indicated that they rarely encounter communication barriers with the elderly during counseling (Fig. 2). A smaller number, 29.3% (95% CI: 24.88-33.73), stated that they often do, and only 6.2% (95% CI: 3.81-8.49) – very often. Identifying and overcoming communication barriers in the pharmacist-elderly patient relationship depend on the techniques and tools applied by pharmacists in practice. In this sense, implementing a counseling algorithm for elderly patients in community pharmacies would have a significant impact on the quality of communication between them.
Furthermore, the majority of respondents indicated that often (47.4%, 95% CI: 42.43-52.14), the elderly had erroneous information about the requested medications; only 6.4% (95% CI: 4.02-8.78) indicated “very rarely”, and 1.7% (95% CI: 0.45-2.99) – “never” (Fig. 3). Thus, open and effective communication, as well as adapting the language to the elderly’s level of understanding, can make a difference in assimilating accurate information about medications provided in the community pharmacy.
When elderly individuals have erroneous information about the medications they are about to administer or do not receive complete and clear information about them from the specialist, the rate of administration errors increases. Responses provided by pharmacists indicate that the most common errors made by the elderly are related to not following the prescribed treatment duration (80.3%, 95% CI: 76.42-84.16), followed by missed doses (70.0%, 95% CI: 65.49-74.41) and administering medications without consulting the doctor or pharmacist and receiving the necessary recommendations (64.3%, 95% CI: 59.62-68.94) (Fig. 4).
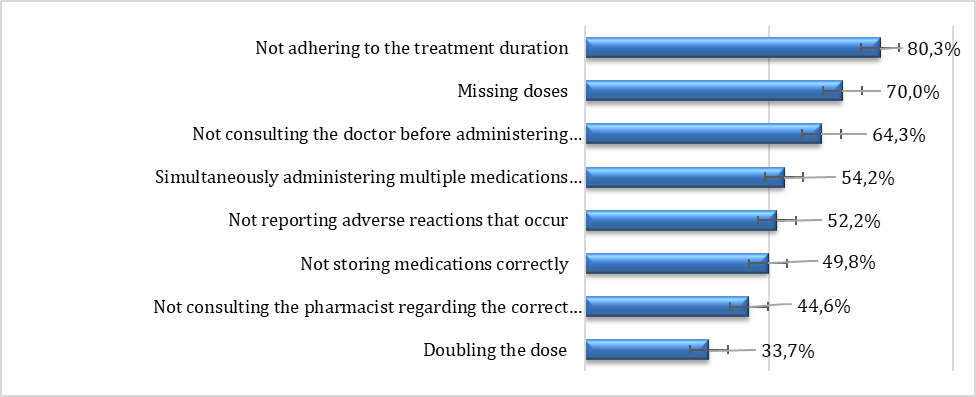 |
Fig. 4 Frequency of errors committed by the elderly regarding medication treatment, %. Each error category is represented as follows: Not adhering to the treatment duration: 80.3%; Missing doses: 70.0%; Not consulting the doctor before administering medications: 64.3%; Simultaneously administering multiple medications from the same therapeutic group: 54.2%; Not reporting adverse reactions: 52.2%; Not storing medications correctly: 49.8%; Not consulting the pharmacist regarding correct administration: 44.6%; Doubling the dose: 33.7%. |
To prevent medication errors, pharmacists are encouraged to ask elderly patients questions and to speak openly with them about any difficulties or uncertainties they may have regarding their medication. This helps build trust in the pharmacist and ensures that patients are properly informed about their treatment.
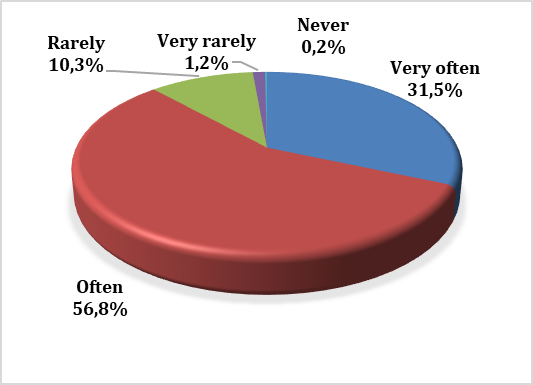 |
Fig. 5 The frequency of questions asked to elderly patients about the medications they take during their visit to the pharmacy. The data is categorized as follows: Very often: 31.5%; Often: 56.7%; Rarely: 10.3%; Very rarely: 1.2%; Never: 0.2%. |
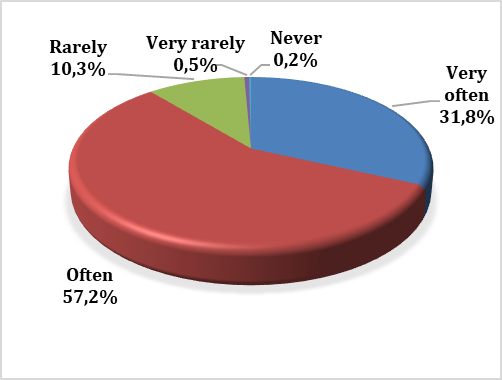 |
Fig. 6 The frequency of questions asked to elderly patients about the ailments they suffer from during their visit to the pharmacy. The data is categorized as follows: Very often: 31.8%; Often: 57.2%; Rarely: 10.3%; Very rarely: 0.5%; Never: 0.2%. |
Thus, the majority of respondents indicated that they often (56.8%, 95% CI: 51.82-61.47) and very often (31.5%, 95% CI: 27.0-36.04) ask elderly individuals questions regarding the medications they administer (Fig. 5), and similarly about the ailments they suffer from (Fig. 6).
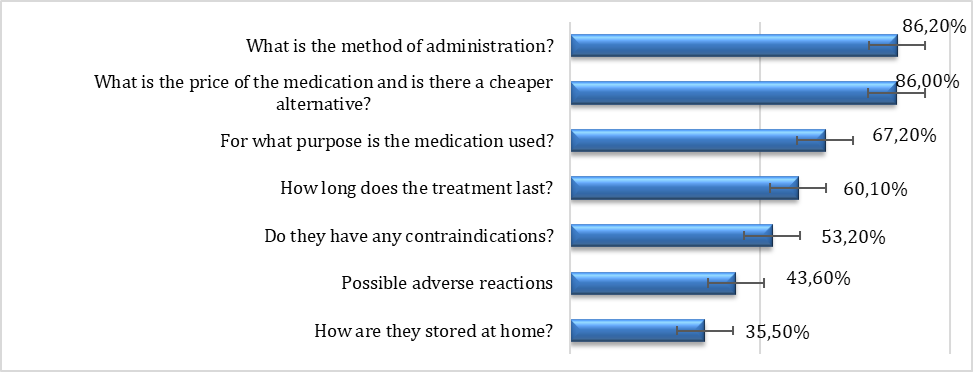 |
Fig. 7 Type of questions asked by the elderly to pharmacists regarding the requested/dispensed medications, %. Each question type is represented as follows: What is the method of administration? 86.2%; What is the price of the medication and is there a cheaper alternative? 86.0%; For what purpose is the medication used? 67.2%; How long does the treatment last? 60.1%; Do they have any contraindications? 53.2%; Possible adverse reactions: 43.6%; How are they stored at home? 35.5%. |
Pharmacists can structure interactions with patients by asking a series of open and closed questions, ideally starting with a broad open-ended question followed by a few specific closed questions, to find out about the medications and ailments the elderly suffer from and to engage them in the discussion. Pharmacists who avoid leading and loaded questions can ensure that the elderly feel comfortable and help create a pleasant environment. As a result, the latter will provide truthful information. In addition, pharmacists who ask elderly patients „why?” may appear critical and sometimes indifferent, which is why it is recommended that, instead of asking „why?”, pharmacists request information using phrases such as, „Please, in your view, explain your decision to ...?”. In this context, it is relevant that most pharmacists have indicated that the elderly ask various questions regarding the requested medications (Fig. 7).
Thus, community pharmacists can assert their position as the primary specialist in the field of medication and provide pharmaceutical care based on medication therapy management: educate elderly patients about dispensed medications, prevent drug interactions and polypharmacy, increase treatment adherence, and collect information about adverse drug reactions, etc.
Interaction with elderly patients in the community pharmacy has many challenges, but also opportunities. Besides focusing on pharmacists ensuring that patients understand the treatment regimens recommended by doctors, an important aspect is also establishing treatment plans for minor ailments. In this case, pharmacists are the ones who recommend and select over-the-counter medications suitable for the elderly patient. Respondents indicated that the elderly ask them for advice regarding the treatment of ailments such as muscle pain (92.4%, 95% CI: 89.78-94.94), insomnia (86.4%, 95% CI: 82.85-89.56), constipation (79.8%, 95% CI: 75.89-83.70), and cough (57.6%, 95% CI: 52.82-62.44), etc. (Fig. 8).
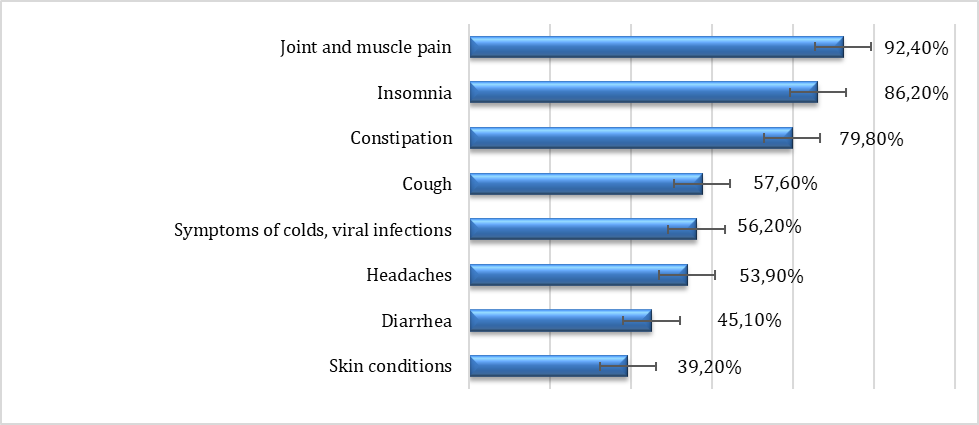 |
Fig. 8 Ailments/symptoms for which the elderly seek the pharmacist's advice, %. Each condition is represented by the following percentages: Joint and muscle pain: 92.4%; Insomnia: 86.2%; Constipation: 79.8%; Cough: 57.6%; Symptoms of colds and viral infections: 56.2%; Headaches: 53.9%; Diarrhea: 45.1%; Skin conditions: 39.2%. |
The application of effective communication principles allows for providing the elderly with the necessary information regarding the medication for these minor ailments. Nonverbal components, including eye contact, smiling, posture, the presence or absence of privacy space, and external appearance, are important for effective communication and properly guiding the elderly about the ailments they suffer from. Verbal communication should also be carefully controlled and designed by the pharmacist. Verbal components, such as reflective listening, asking questions, referencing, and using appropriate terminology, can greatly influence the success of a conversation with elderly patients.
Empathy conveyed through smiling, a warm voice, head tilting, and eye contact is correlated with increased receptiveness and information sharing from elderly patients. Additionally, applying standardized communication techniques, such as a counseling algorithm centered on the elderly patient, would allow for correct and rational decision-making about their medication, especially in cases of minor ailments.
Conclusions
1. An analytical synthesis of the literature on communication principles was conducted, and those necessary for application in the process of counseling patients in community pharmacies were highlighted.
2. The principles and communication rules that must be followed in specialized geriatric pharmaceutical care have been highlighted.
3. The counseling algorithm for geriatric patients in the community pharmacy was developed based on the results obtained from surveying pharmacists, which will be included in the guide for the management of specialized pharmaceutical care for high-risk patients.
Competing interests
None declared.
Ethics approval
The study protocol was approved by the Research Ethics Committee of Nicolae Testemiţanu State University of Medicine and Pharmacy (minutes No. 52 to 62, from 18.06.2015).
Acknowledgements and funding
No external funding.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Author’s ORCID ID
Tatiana Șchiopu – https://orcid.org/0000-0001-6550-2261
References
Codul deontologic al farmaciştilor din Republica Moldova [Code of ethics for pharmacists in the Republic of Moldova [Internet]. Chisinau; 2014 [cited 2024 Dec 14]. Available from: https://farmaciesociala.usmf.md/wp-content/blogs.dir/168/files/sites/16….
Guvernul Republicii Moldova [Government of the Republic of Moldova]. Hotărârea nr. 599 din 28.08.2024, cu privire la aprobarea Regulilor de bună practică de farmacie [Decision no. 599 of 28.08.2024 on the approval of the Rules of good pharmacy practice]. Monitorul Oficial al Republicii Moldova [Internet]. 2024;(414-417):art. 781 [cited 2025 Ian 15] Available from: https://www.legis.md/cautare/getResults?doc_id=145226&lang=ro.Romanian.
Guvernul Republicii Moldova [Government of the Republic of Moldova]. Hotărârea nr. 192 din 24.03.2017, cu privire la aprobarea Codului deontologic al lucrătorului medical şi al farmacistului [Decision no. 192 of 24.03.2017, on the approval of the Code of ethics of the medical worker and the pharmacist]. Monitorul Oficial al Republicii Moldova [Internet]. 2017;(92-102):art. 265 [cited 2025 Ian 15]. Available from: https://www.legis.md/cautare/getResults?doc_id=98572&lang=ro. Romanian.
Council on Credentialing in Pharmacy. Scope of contemporary pharmacy practice: roles, responsibilities, and functions of pharmacists and pharmacy technicians [Internet]. Washington: CCP; 2009 [cited 2025 Ian 15]. Available from: https://www.pharmacycredentialing.org/Files/Scope_of_Contemporary_Pharmacy_Practice.pdf.
National Association of Pharmacy Regulatory Authorities (NAPRA). Professional competencies for Canadian pharmacists at entry to practice [Internet]. Ottawa: NARPA; 2014 [cited 2025 Ian 15]. Available from: https://napra.ca/wp-content/uploads/2022/09/NAPRA-Comp-for-Cdn-PHARMACISTS-at-Entry-to-Practice-March-2014-b.pdf.
Pharmaceutical Society of Australia. National competency standards framework for pharmacists in Australia [Internet]. Deakin: PhSA; 2010 [cited 2025 Ian 16]. Available from: https://www.psa.org.au/wp-content/uploads/2018/06/Competency_standards_2010.pdf.
Pharmacy Council of New Zealand. Competence standards for the pharmacy profession [Internet]. Wellington: The Council; 2015 [cited 2025 Ian 16]. Available from: https://pharmacycouncil.org.nz/wp-content/uploads/2021/04/CompStds2015Web.pdf.
General Pharmaceutical Council. Standards for pharmacy professionals, May 2017 [Internet]. London: The Council; 2017 [cited 2025 Ian 15]. Available from: https://assets.pharmacyregulation.org/files/standards_for_pharmacy_professionals_may_2017_0.pdf.
Accreditation Council for Graduate Medical Education (ACGME). Interpersonal skills and communication - ACGME Competencies [Internet]. Baltimore: University of Maryland Medical Center; c2025 [cited 2025 Ian 18]. Available from: https://www.umms.org/ummc/pros/gme/acgme-competencies/interpersonal-skills-communication.
Kälvemark Sporrong S, Kaae S. Trends in pharmacy practice communication research. Pharmacy (Basel). 2018;6(4):127. doi: 10.3390/pharmacy6040127.
O’Daniel M, Rosenstein AH. Professional communication and team collaboration. In: Hughes RG, editor. Patient safety and quality: an evidence-based handbook for nurses [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008. Chapter 33. [cited 2025 Ian 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2637/.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing fundamentals. Chapter 2: Communication [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021 [cited 2025 Ian 18]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK591817/.
Naughton CA. Patient-centered communication. Pharmacy (Basel). 2018 Feb 13;6(1):18. doi: 10.3390/pharmacy6010018.
Abdolrahimi M, Ghiyasvandian S, Zakerimoghadam M, Ebadi A. Therapeutic communication in nursing students: a Walker & Avant concept analysis. Electron Physician. 2017;9(8):4968-4977. doi: 10.19082/4968.
Bartlett G, Blais R, Tamblyn R, Clermont Rj, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. doi: 10.1503/cmaj.070690.
Swift M. The impact of poor communication on medical errors. 2017 May 12 [cited 2025 Ian 16]. In: The Doctor Weighs In [Internet]. Available from: https://thedoctorweighsin.com/impact-poor-communication-on-medical-errors/.
Gîlca B, Gramma R, Paladi A. Ghid privind aplicarea procedurii de comunicare și consiliere a pacienților [Guidelines for applying patient communication and counseling procedures] [Internet]. Chisinau: The Ministry of Health of the Republic of Moldova; 2018 [cited 2025 Ian 15]. Available from: https://ms.gov.md/wp-content/uploads/2024/12/GHID-privind-aplicarea-procedurii-de-comunicare-și-consiliere-a-pacienților.pdf. Romanian.
Adauji S. Information support of the pharmacist's communication in the process of pharmaceutical assistance of the population. Sănătate Publică, Economie şi Management în Medicină [Public Health Econ Manag Med] (Chisinau). 2023;(2):20-27. https://doi.org/10.52556/2587-3873.2023.2(95).03.
Şchiopu T, Sîbii L, Brumărel M, Safta V, Dogotari L, Buliga V, Adauji S. The perception of the concept of rational use of medicines by the elderly in urban and rural environments. Revista Farmaceutică a Moldovei [Mold Pharm J]. 2023;(2):10-18. ISSN 1812-5077.
Şchiopu T. Self-medication with non-steroidal anti-inflammatory drugs in the elderly. In: Congress dedicated to the 75th anniversary of the founding of the Nicolae Testemiţanu State University of Medicine and Pharmacy, October 21-23, 2020, Chisinau, Republic of Moldova: Abstract book [Internet]. Chisinau; 2020 [cited 2025 Ian 15]. Available from: https://ibn.idsi.md/ro/vizualizare_articol/126947. Romanian.
Şchiopu T, Groian A, Diaconu A, Sîbii L, Zgîrcu E, Dogotari L, Adauji S. Medication administration errors by the elderly at home. In: Perspectives of the Balkan medicine in the post COVID-19 era: the 37th Balkan Medical Week and the 8th Congress on urology, dialysis and kidney transplant from the Republic of Moldova “New Horizons in Urology”, 7-9 June 2023 [Internet]. Chisinau; 2023 [cited 2025 Ian 15]. Available from: https://ibn.idsi.md/ro/vizualizare_articol/194119