Introduction
According to statistical data, bladder cancer is considered to be worldwide one of the most frequently diagnosed cancer. If taking in account only the male population, it is the sixth most frequently diagnosed cancer among the diagnosed worldwide cancers. If taking in consideration both genders, it is the tenth one. Very demonstrative are the data of the year 2018, when 549,000 new cases of bladder cancer worldwide were diagnosed, and 200,000 deaths were registered [1].
The intensive development of new technologies and approaches to the diagnosis of bladder cancer, such as ultrasound, magnetic resonance imaging and multislice computed tomography, makes the diagnosis of the disease at stages Ta and T1 usually possible. Approximately 75–80% of all newly diagnosed bladder tumors are non-muscle invasive (Ta, T1, carcinoma in situ) tumors [2].
According to literature data the recurrence rate of NMIBC is reported in the frames of 50–70% [3]. Following the guidelines, the current treatment for primary NMIBC is the transurethral resection of bladder tumor (TURBT) which is combined with postoperative intravesical instillation [4]. It has been proven that the rate of disease recurrence depends on the quality of the primary surgical operation [5].
The surgical technique remains practically unchanged since its introduction into practice. The main principles consist in the gradual removal of the protruding part of the tumor, following by the removal of the base using a resectoscope loop. In this case, the resected tumor fragments float freely in the bladder cavity. In this context many authors have repeatedly suggested that a relapse of bladder cancer may occur as a result of implantation of floating tumor cells [6]. Another suggestion consists in missing the bladder detrusor muscle [7, 8]. According to various data, the incidence of relapses after TUR of the bladder wall with a tumor in muscular-non-invasive bladder cancer is up to 50–80%, the incidence of T1 tumors after TUR is 33–53%, and TaG3 is 41.4% [9, 10]. These values show the necessity for searching an alternative for the standard method in order to correspond to modern requirements and to reduce the frequency of recurrence development.
In 1978 G. Staehler et al. first described the successful removal of a bladder tumor using a neodymium:YAG laser [11]. In fact, it was the vaporization of the tumor, but its disadvantage is the lack of data about the tumor’s morphology and the degree of its invasion. Very high interest is towards the method of bladder tumor resection in a single block (en-bloc), which was successfully performed for the first time by T. Kawada et al. in 1997 using monopolar resection and a special hook-electrode [12]
Due to the transurethral en bloc technique it is possible to remove the tumor together with the bladder detrusor below its bed. Another advantage of this emerging technique is that the bladder detrusor is clearly displayed. Important to mention is that the en bloc resection makes possible to obtain excellent morphological specimens. It leads to reducing as well of the tumor spread as also the recurrence [13, 14].
The basic principle of en bloc resection is to perform a circular resection of the bladder wall (mucous membrane, submucosal and muscle layers) with an indentation of 5-10 mm from the tumor edge, while the tumor is excised together with the base in a circle and is removed entirely from the wall. The main goals pursued when performing en-bloc resection are to improve the quality of material for morphological investigation and, consequently, to a correct staging of the tumors, reduction of the free floating of tumor cells, and finally to a reduction of the incidence of disease recurrence and tumor progression [4, 5, 7, 13, 14].
Due to the development of laser surgery, the appearance of holmium (Ho:YAG) and later, in the 1990s, the appearance of thulium (Tm:YAG) lasers, the en-bloc laser resection was possible. Further studies show its high efficacy and safety [15]. The aim of the study is to compare results after Thulium laser En-bloc transurethral resection and transurethral resection of non-muscular invasive urinary bladder tumors.
Material and methods
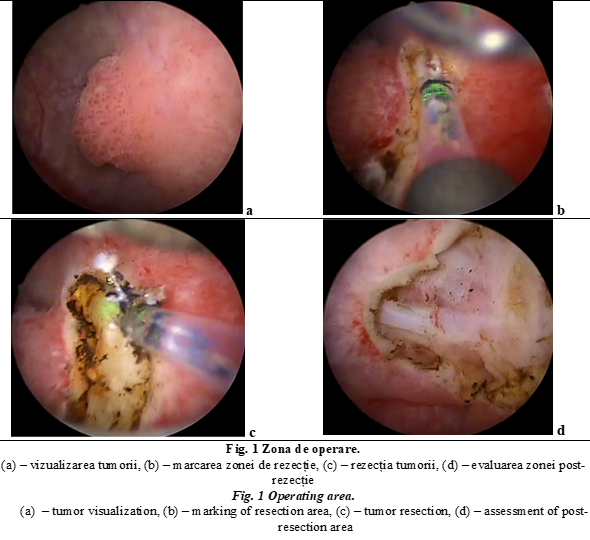
The study was performed between February 2017 and May 2019, within the department of Urology and Surgical Nephrology of the Nicolae Testemițanu State University of Medicine and Pharmacy, in the Timofei Moşneaga Republican Clinical Hospital . 65 patients with bladder tumor pathology were surgically treated. A transversal descriptive study was performed. Study protocol was approved by University Ethics committee (№ 4 at 16 December 2019). The 65 patients were divided in two groups: Main group includes 32 patients treated by Thulium laser En-bloc transurethral resection of bladder tumors (TmLRBT) and the control group includes 33 patients treated by transurethral resection of bladder tumors (TURBT). All patients were selected according to the following criteria. The inclusion criteria were primary non-muscular invasive bladder cancer, patients over 18-year-old and the Eastern Cooperative Oncology Group (ECOG) score 0-2. The exclusion criteria were identified as follows: severe comorbidities, other non-urothelial tumors, ECOG score ≥ 3 and pregnancy. The obtained data were comparatively analyzed. Descriptive statistic was applied. In this study the results are demonstrated as absolute and relative values. For Thulium laser En-bloc transurethral resection RevoLix DUO (LISA laser Germania) were used.
Tabelul 1. Date demografice ale pacienților și tumorilor. Table 1. Patient and tumor demographics. | ||||
Parametrii Parameters | Categorii Categories | TmLRBT (n=32) | TURBT (n=33) | Total (n=65) |
Sex Gender | Bărbați, n (%) Men, n (%) | 25 (78%) | 25 (76%) | 50 (77%) |
Femei, n (%) Women, n (%) | 7 (22%) | 8 (24%) | 15 (23%) | |
Vârstă, ani Age, years | Vârsta medie (CI 95%) Mean age (CI 95%) | 64,8 (25-84) | 65,4 (27-87) | 65,1 (25-87) |
Grupă de vârstă Age group: | 18-30 ani, n (%) 18-30 years, n (%) | 2 (6%) | 2 (6%) | 4 (6%) |
31-60 ani, n (%) 31-60 years, n (%) | 9 (28%) | 10 (30%) | 19 (29%) | |
60 de ani și mai mult, n (%) 60 years and more, n (%) | 21 (66%) | 21 (64%) | 42 (65%) | |
Tutun/Fumat Tobacco/Smoking | Da, n (%) Yes, n (%) | 15 (47%) | 14 (42%) | 29 (45%) |
Numărul de tumori Number of tumors | Tumori unice, n (%) Single tumors, n (%) | 22 (69%) | 20 (61%) | 42 (65%) |
≥ 2 tumori, n (%) ≥ 2 tumors, n (%) | 10 (31%) | 13 (39%) | 23 (35%) | |
Dimensiunea tumorii Tumor size | < 3 cm, n (%) | 24 (75%) | 22 (67%) | 46 (71%) |
≥ 3 cm, n (%) | 8 (25%) | 11 (33%) | 19 (29%) | |
Notă: CI – Interval de încredere; TmLRBT – en-bloc rezecția transuretrală cu thulium laser a tumorii vezicii urinare; TURBT – rezecția transuretrală a tumorii vezicii urinare; n — numărul. Note: CI – Confidence Interval; TmLRBT – thulium laser en-bloc transurethral resection of bladder tumor; TURBT – transurethral resection of bladder tumor; n — number. | ||||
Results
During the procedures intraoperatively occurred some not significant hemorrhages, so no blood transfusion was required. Between these two groups some clinical and pathological characteristics were compared: age, gender, tumor grade, tumor size, number of tumors, postoperative complications, oncological and histological outcomes (Table 1, Table 2).
According to gender repartition, from the 65 patients included in the study, 50 (78%) were men and 15 (23%) women. The mean age was 65,1 years, age varies between 25 years to 87 years and the majority of the patients were over 60 years (65%).
The results of the analysis of tumors showed (table 1) that in most cases, tumors were localized on the lateral walls of the bladder, a tumor up to 3 cm in size was detected in 71% of cases (46 patients) and single bladder tumors were detected in 65% of cases (42 patients) included in the study. In the development of bladder cancer, the use of tobacco/smoking is considered as an important risk factor, which was present in 29 patients (45% of cases).
Histopathological analysis showed that the groups of patients included in the study are homogeneous according to TNM 2017 classification of urinary bladder cancer and according to 2004/2016 WHO (World Health Organization) histopathology grade classification system (table 2).
Regarding the Clavien-Dindo's classification of surgical complications only grade I and grade II complications occurred in each group (table 2). Obturator nerve reflex during the operation has occurred in 15% of cases in the TURBT group and no one was observed in the TmLRBT group. The reason therefore is the use of non-electrical source of energy, so it led to less bladder perforation (more controlled perforation) in TmLRBT group, with only one observed case (3%) of grade II bladder perforation. In TURBT group bladder perforation had occurred in 3 patients (9%), it was managed by catheterization for a frame of tome of 3-4 days. The histopathological examination reveals the detection of detrusor muscle in both groups: 73% in the TURBT group and 97% in the TmLRBT group.
Tabelul 2. Rezultatele chirurgicale și histologice. Table 2. Surgical and histological outcomes. | ||||
Parametrii Parameters | Categorii Categories | TmLRBT (n=32) | TURBT (n=33) | Total (n=65) |
Gradul de histopatologie 2004/2016 OMS Histopathology grade 2004/2016 WHO | Grad scăzut, n (%) Low-grade, n (%) | 19 (59%) | 18 (55%) | 37 (57%) |
Grad crescut, n (%) High-grade, n (%) | 13 (41%) | 15 (45%) | 28 (43%) | |
TNM 2017 clasificare TNM 2017 classification | Ta, (Tis), n (%) | 21 (66%) | 20 (61%) | 41 (63%) |
T1, n (%) | 11 (34%) | 13 (39%) | 24 (37%) | |
Stratul muscular detrusor Detrusor muscle | n (%) | 31 (97%) | 24 (73%) | 55 (85%) |
Clavien-Dindo | CD grad I | 2 (6%) | 3 (9%) | 5 (8%) |
CD grad II | 4 (12%) | 6 (18%) | 10 (15%) | |
Complicații Complications | ONR, n (%) | 0 (0%) | 5 (15%) | 5 (8%) |
BP, n (%) | 1 (3%) | 3 (9%) | 4 (6%) | |
Rata de recurență Recurrence rate | n (%) | 5 (15%) | 13 (39%) | 18 (28%) |
Zona implicată în recurență (localizare) Area involved in recurrence (localization) | Zona de rezecție inițială Initial resection area | 1 (20%) | 7 (54%) | 8 (44%) |
Alta localizare Other localization | 4 (80%) | 6 (46%) | 10 (56%) | |
Notă: TmLRBT – en-bloc rezecția transuretrală cu Thulium laser a tumorii vezicii urinare; TURBT – rezecția transuretrală a tumorii vezicii urianre; OMS – Organizația Mondială a Sănătății; Grad scăzut – carcinom urotelial papilar cu grad scăzut de malignitate; Grad crescut – carcinom urotelial papilar cu grad crescut de malignitate; Tis (CIS) – carcinoma in situ, “flat tumor; Ta – tumora papilară non-invazivă; T1 – invadează țesutul conjunctiv subepitelial; CD – Clavien-Dindo; ONR – reflexul nervului obturator; BP – perforația vezicii urinare; n — numărul. Note: TmLRBT – Thulium laser En-bloc transurethral resection of bladder tumor; TURBT – transurethral resection of bladder tumor; WHO – World Health Organization; Low-grade – low-grade papillary urothelial carcinoma; High-grade – high-grade papillary urothelial carcinoma; Tis (CIS) – Carcinoma in situ, “flat tumor”; Ta – noninvasive papillary tumor; T1 – invades subepithelial connective tissue; CD – Clavien-Dindo; ONR – obturator nerve reflex; BP – bladder perforation; n — number. | ||||
All surgical procedures were performed as a one-step intervention with a following patients’ follow-up during 12-months. The majority of recurrences during the follow-up occurred in the TURBT group 39% (13 cases) in initial resection area 54% (7 cases). For TmLRBT group recurrence rate was 15% (5 cases) and a big part of recurrences occurred in the non-primary resection area 80% (4 cases).
Discussion
The traditional TURBT technique still remains the golden standard which is applied according to the guidelines of EAU and NCCN for the diagnosis and treatment of initial NMIBC. Still remains the problem of recurrences in patients with NMIBC treated even by TURBT. The report of Kikuchi E. et al. shows that the 1-year, 3-year, and 5-year RFS rate of patients with NMIBC were 77.0%, 61.3%, and 52.8% [16]. In order to prevent the recurrence of NMIBC the intravesical instillation was regarded as an efficient treatment. Important to mention is that until now there is still no consensus regarding an optimal protocol for intravesical instillation [17].
Recently a common opinion is that the absence of detrusor muscle observed in the specimens which were obtained by TURBT means a significantly higher risk for an early recurrence [7]. Nowadays it is ascertained that the en-bloc resection done with high quality specimens show the presence of detrusor muscle in 96 – 100% of cases [15].
The en-bloc laser resection method has significant advantages in comparison with traditional TUR procedure. To markable advantages count: the complete absence of an obturator reflex and, therefore, a lower probability of unexpected perforations and bleeding, a decrease in the contact of the resected tumor with an unchanged bladder wall, as well as obtaining high-quality material for pathomorphological examination [15, 18].
The results of the histopathological examination according to TNM 2017 classification and 2004/2016 WHO histopathology grade classification system show similar results in booth groups: stage Ta was detected in 63% (41 patients) of cases and stage T1 was in 37% (24 patients) of cases, low-grade papillary urothelial carcinoma in 57% (37 patients) of cases and high-grade papillary urothelial carcinoma in 43% (28 patients) of cases included in the study. The presence of detrusor muscles was detected in 74% (24 patients) cases in the TURBT group and 97% (31patients) cases in the TmLRBT group.
In the macropreparations obtained after traditional TUR, there is a high thermal damage of the cellular and intercellular structures. This makes not only the differentiation of the tumor itself complicated (sometimes it also requires the use of an expensive immunohistochemical study), but also the determination of invasion into the muscle layer (T staging). According to the literature data, the presence of detrusor elements after TUR is observed in 50–86% of cases. The absence of elements of the muscle layer, especially in high-grade papillary urothelial carcinoma, makes the radicality of the primary operations uncertain, leading to the consequence that in some cases an early reoperation is required. In contrast to electrosurgery, the penetrating power of laser energy is evident lower (0,2–0,4 mm) and, therefore, less damage of the macropreparation. The en-bloc laser resection ensures a detection rate of detrusor elements, which is about 96–100%. This fact obviously improves the diagnosis and treatment results [19].
Bleeding and perforation of the bladder wall hinder an immediate intravesical instillation of the chemotherapy drug after surgery, consequently it reduces the oncological effectiveness of the combined treatment. According to EORTC, a single postoperative intravesical chemotherapy improves the 5-year survival without recurrence by 14% [15].
According to the Clavien-Dindo classification of complications, in both groups was recorded complication grade I and II (Table 2). The list of complications includes: urinary tract infection, urinary retention, hematuria of different intensity, obturator nerve reflex and bladder perforation which was managed whit a standard approach, without additional complexities. The recurrence rate in the TURBT group is about 39% and in the TmLRBT group about 15%, so it shows the benefit of laser En-bloc resection.
In 2016 Y.P. Wu et al. published interesting meta-analysis data. This meta-analysis of literature data is based on the results of 7 studies and includes 886 patients, 438 were treated by en bloc resections and 448 by TUR. The results showed that en-bloc resection was significantly more efficient in comparison with TUR regarding terms of bladder catheterization time, hospital stay, complications, and recurrence rates. In addition, it was noted that the quality of the macropreparation was also significantly better [20].
Conclusions
TheThulium laser En-bloc transurethral resection of non-muscle-invasive bladder tumor proved to be an effective and safe method of treatment compared with the conventional transurethral resection. This technique allows the obtaining of tumor samples in a higher quality (detrusor muscle is present in more cases), contributing to a correct diagnosis and staging of the disease. Finally, it leads to a more favorable results and reduction of recurrence rate.
Competing interests
None declared
Authors' contribution
All authors contributed equally to the research, data analysis, and writing of the manuscript. All authors read and approved the final article.
Authors’ ORCID IDs
Ivan Vladanov - https://orcid.org/0000-0002-9703-2775
Alexei Pleșacov - https://orcid.org/0000-0002-0139-4772
Ghenadie Scutelnic - https://orcid.org/0000-0003-1399-8183
Vitalii Ghicavîi - https://orcid.org/0000-0002-2130-9475
References
Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin., 2018; Nov; 68 (6): 394-424.
Ridge C.A., Pua B.B., Madoff D.C. Epidemiology and staging of renal cell carcinoma. Semin. Intervent. Radiol., 2014; Mar; 31 (1): 3-8.
Sylvester R.J., van der Meijden A.P., Oosterlinck W., Witjes J.A., Bouffioux C., Denis L., Newling D.W., Kurth K. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur. Urol., 2006; Mar; 49 (3): 466-5; discussion 475-7.
Babjuk M., Böhle A., Burger M., Capoun O., Cohen D., Compérat E.M., Hernández V., Kaasinen E., Palou J., Rouprêt M., van Rhijn B.W.G., Shariat S.F., Soukup V., Sylvester R.J., Zigeuner R. EAU Guidelines on Non-Muscle-invasive Urothelial Carcinoma of the Bladder: Update 2016. Eur Urol., 2017; Mar; 71 (3): 447-461.
Мартов А.Г., Ергаков Д.В., Байков Н.А. и др. Трансуретральное удаление опухолей мочевого пузыря единым блоком. Онкоурология, 2015; (1): 41–9. [Martov A.G., Ergakov D.V., Baykov N.A. et al. Transurethral en bloc resection of bladder tumors. Onkourologiya = Cancer Urology, 2015; (1): 41–9. (In Russ.)].
Bryan R.T., Collins S.I., Daykin M.C., Zeegers M.P., Cheng K.K., Wallace D.M., Sole G.M. Mechanisms of recurrence of Ta/T1 bladder cancer. Ann R. Coll. Surg. Engl, 2010; Sep; 92 (6): 519-24.
Mariappan P., Zachou A., Grigor K.M. Edinburgh Uro-Oncology Group. Detrusor muscle in the first, apparently complete transurethral resection of bladder tumour specimen is a surrogate marker of resection quality, predicts risk of early recurrence, and is dependent on operator experience. Eur. Urol., 2010; May; 57 (5): 843-9.
Gontero P., Sylvester R., Pisano F., Joniau S., Vander Eeckt K., Serretta V., Larré S., Di Stasi S., Van Rhijn B., Witjes A.J., Grotenhuis A.J., Kiemeney L.A., Colombo R., Briganti A., Babjuk M., Malmström P.U., Oderda M., Irani J., Malats N., Baniel J., Mano R., Cai T., Cha E.K., Ardelt P., Varkarakis J., Bartoletti R., Spahn M., Johansson R., Frea B., Soukup V., Xylinas E., Dalbagni G., Karnes R.J., Shariat S.F., Palou J. Prognostic factors and risk groups in T1G3 non-muscle-invasive bladder cancer patients initially treated with Bacillus Calmette-Guérin: results of a retrospective multicenter study of 2451 patients. Eur. Urol., 2015; Jan; 67(1): 74-82.
Kamat A.M., Bağcıoğlu M., Huri E. What is new in non-muscle-invasive bladder cancer in 2016? Turk. J. Urol., 2017; Mar; 43 (1): 9-13.
Grimm M.O., Steinhoff C., Simon X. et al. Effect of routine repeat transurethral resection for superficial bladder cancer: a long-term observational study. J. Urol., 2003; 170 (2 Pt 1): 433–7.
Staehler G., Schmiedt E., Hofstetter A. Destruction of bladder neoplasms by means of transurethral neodym-YAGlaser coagulation. Helv. Chir. Acta., 1978; 45 (3): 307–11.
Kawada T., Ebihara K., Suzuki T. et al. A new technique for transurethral resection of bladder tumors: rotational tumor resection using a new arched electrode. J. Urol., 1997; 157 (6): 2225–6.
Kramer M.W., Bach T., Wolters M., Imkamp F., Gross A.J., Kuczyk M.A., Merseburger A.S., Herrmann T.R. Current evidence for transurethral laser therapy of non-muscle invasive bladder cancer. World J. Urol., 2011; Aug; 29 (4): 433-42.
Kramer M.W., Altieri V., Hurle R., Lusuardi L., Merseburger A.S., Rassweiler J., Struck J.P., Herrmann T.R.W. Current Evidence of Transurethral En-bloc Resection of Nonmuscle Invasive Bladder Cancer. Eur. Urol. Focus, 2017; Dec; 3 (6): 567-576.
Kramer M.W., Rassweiler J.J., Klein J., Martov A., Baykov N., Lusuardi L., Janetschek G., Hurle R., Wolters M., Abbas M., von Klot C.A., Leitenberger A., Riedl M., Nagele U., Merseburger A.S., Kuczyk M.A., Babjuk M., Herrmann T.R. En bloc resection of urothelium carcinoma of the bladder (EBRUC): a European multicenter study to compare safety, efficacy, and outcome of laser and electrical en bloc transurethral resection of bladder tumor. World J. Urol., 2015; Dec; 33 (12): 1937-43.
Kikuchi E., Fujimoto H., Mizutani Y., Okajima E., Koga H., Hinotsu S., Shinohara N., Oya M., Miki T. Cancer Registration Committee of the Japanese Urological Association. Clinical outcome of tumor recurrence for Ta, T1 non-muscle invasive bladder cancer from the data on registered bladder cancer patients in Japan: 1999-2001 report from the Japanese Urological Association. Int. J. Urol., 2009; Mar; 16 (3): 279-86.
Sylvester R.J., Oosterlinck W., Witjes J.A. The schedule and duration of intravesical chemotherapy in patients with non-muscle-invasive bladder cancer: a systematic review of the published results of randomized clinical trials. Eur. Urol., 2008; Apr; 53 (4): 709-19.
EAU Guidelines on lasers and technologies. European Association of Urology. Guidelines, 2016; Pp. 6–55.
EAU Guidelines on non-muscle-invasive bladder cancer (Ta, T1 and CIS). European Association of Urology. Guidelines, 2017; Pp. 4–40.
Wu Y.P., Lin T.T., Chen S.H., Xu N., Wei Y., Huang J.B., Sun X.L., Zheng Q.S., Xue X.Y., Li X.D. Comparison of the efficacy and feasibility of en bloc transurethral resection of bladder tumor versus conventional transurethral resection of bladder tumor: A meta-analysis. Medicine (Baltimore), 2016; Nov; 95 (45): e5372.

