Introduction
Thyroid cancer is the most common endocrine neoplasm, with an upward trend in global incidence. According to the latest report of the World Health Organization, in 2018, 567,233 new cases of thyroid cancer were diagnosed worldwide, of which 78,418 in Europe and with a global mortality rate of 41,071 cases [1]. In Republic of Moldova, the thyroid cancer morbidity index in 1985 was 1,35 new cases per 100,000 population annually, in 2000 – 2.5 new cases, and in 2011 – 6.8 new cases of disease per 100,000 population. In 2016, 12.8 new cases of disease per 100,000 population were registered in the Republic of Moldova [2].
The precise reasons for the increased incidence are not clearly elucidated, but may be related, at least in part, to the introduction of an improved diagnostic methodology (ultrasonography, thyroid scanning and fine-grained biopsy) and improved cancer registration [2].
Also considered as risk factors for thyroid cancer are several etiological factors:
ionizing radiation is the main etiological factor in the development of thyroid cancer. Persons come from irradiated geographical areas following the production of non-nuclear aids, persons undergoing radiotherapy in order to treat other types of non-neoplastic diseases; people undergoing ionizing radiation in the treatment of various conditions such as tonsillic hypertrophy, anesthesia, impetigo, thymic hypertrophy, ionizing radiation used in imaging,repeated repatriation or abuse of imaging investigations using ionizing radiation, radiation present at the site of the work are increased risk of developing thyroid cancer. Studies conducted among the population diagnosed with thyroid neoplasm have shown that a large part of this has been subjected to treatment and ionizing radiation. Radiation emitted from the production of nuclear aids has been the trigger for many types of neoplastic diseases, including arthritis and thyroid neoplasm. The risk of thyroid neoplasm is directly proportional to the number of exposures to ionizing radiation.
Peculiarities of the female reproductive system. Studies have shown that women over a period of years have had more than two years and are predisposed to the development of thyroid neoplasm, due to the activation of thyroid hormones during pregnancy. Medieval ablation is associated with the risk of thyroid cancer. Spontaneous abortions can lead to the appearance of tumor lesions at the thyroid level. Studies conducted among women diagnosed with benign thyroid disease have shown antecedents of miscarriage. Late menopause, total hysteresis, oral antidepressants, oral administration (or Slomid, medium used in the treatment of infertility) are associated with the risk of developing thyroid disease [12, 13].
Age. The age of the patient diagnosed is a well-established prognostic factor for thyroid cancer survival; is included in the Joint Thyroid Cancer System of the American Joint Cancer Committee (AJCC). In the eighth edition of the AJCC staging system for thyroid carcinoma, the age limit was increased from 45 to 55 years [10]. Studies have shown that the patient's age at the clinical presentation is a variable independently associated with the prognosis of the disease, although for reasons that are not fully understood, younger individuals usually have better survival rates. Apparently, something intrinsic to cancer or treatment depends on the patient's age. Some studies have shown that the clinicopathological presentation does not necessarily follow the prognosis of patients. Younger people usually have clinical and pathological factors traditionally associated with poorer outcomes, despite belonging to the group with better survival.
Gender. Women are seven times more exposed to the risk of developing thyroid neoplasm due to the mechanism of action of endogenous hormones. In men, cardiac affections can favor the appearance of thyroid neoplasm [13].
Blood type. Studies conducted several decades ago have shown a relationship between inherited human ABOs and Rhesus blood groups and the risk of developing various malignancies [6]. Another study by Abbas Ali Tam et al. in 2019 – ABO blood groups, Rh factor and thyroid cancer risk: at “B” or not at “B”, showed that patients with blood group B had a higher risk of extrathyroid enlargement and advanced stage compared to patients with non-B blood group. The risk of thyroid cancer in blood group B was significantly higher compared to the combination of all other blood groups [21].
Conditions affecting thyroiditis, thyroid nodules, acromegaly are associated with a reduced risk of thyroid cancer. Lymphocytic thyroiditis is the most common autoimmune thyroid disease and the most common cause of hypothyroidism. The main cause of the autoimmune process is still unknown and the direct one can be any process that affects the integrity of the thyroid gland and contributes to the passage of thyroglobulin into the blood. The coexistence of autoimmune thyroiditis and thyroid carcinoma has a frequency of 1.0 - 75% according to different authors [14-20]. A link between thyroid cancer and autoimmune thyroid disease has long been recognized, although the exact relationship between the two diseases remains unclear. Epidemiological and histological data indicate that malignant thyroid pathology occurs frequently in the context of autoimmune thyroiditis, which is one of the most common autoimmune thyroid diseases and that it is frequently infiltrated by inflammatory-immune cells [4]. The increased incidence of carcinomas in patients with autoimmune thyroiditis suggests that the latter may be a precancerous condition.
In medical practice, the early diagnosis of thyroid cancer is difficult because the neoplasm coexists or develops against the background of thyroid nodulo-inflammatory pathologies, which have a slow evolution.
In conclusion, the main problem related to autoimmune thyroiditis with clinical suspicion of malignancy is to confirm the preoperative oncological element in order to assess the volume of subsequent surgical treatment performed. In most cases, starting from the dimensions, ultrasound, clinical aspect, a true result is not obtained and the study of the epidemiology of tumor diseases will contribute to the knowledge of the dynamics and specificity of the oncological patient of thyroid profile, later with the development of personalized prophylactic measures to combat cancer.
Material and methods
The research was conceived as a prospective, selective study. 234 patients were enrolled, who were treated in the scientific laboratory tumors of the head and neck region of the Oncological Institute. The study was conducted during the years 2017-2020 with the approval of the Research Ethics Committee of the „Nicolae Testemitanu” State University of Medicine and Pharmacy of the Republic of Moldova, minutes № 76 from 14.11.2016. Patients met the criteria for inclusion in the study (patient consent with informed consent, age, patients with thyroid cancer developed on a healthy background and on the background of autoimmune thyroiditis).
The cases were divided into 2 groups, group 1 was in turn divided into 2 groups:
Lot CT (thyroid carcinoma) + TA (autoimmune thyroiditis) (PE +) (eco-guided puncture)
Lot CT + TA (PE-)
Lot CT + FS (healthy background)
All patients in group I group 1 underwent ultrasound-guided puncture of thyroid nodules.
In order to distribute the patients according to the territorial administrative unit, we consulted the national statistics office. According to which the administrative-territorial units were distributed in the northern, central and southern areas of the country:
in the northern area were included the districts: Balti, Briceni, Donduseni, Drochia, Edinet, Falesti, Floresti, Glodeni, Ocnita, Riscani, Singerei, Soroca;
in the center area: Chisinau, Calarasi, Criuleni, Dubasari, Hincesti, Ialoveni, Nisporeni, Orhei, Rezina, Straseni, Soldanesti, Telenesti, Ungheni, Anenii Noi;
in the southern area: Basarabeasca, Cahul, Cantenir, Caușeni, Cimișlia, Leova, Ștefan-Vodă, Taraclia, U.T.A Găgăuzia.
Statistical analysis performed
Data series analysis was performed using the statistical applications of Microsoft Excel and the specialized software SofaStats ver. 1.4.6 (freeware). The data are presented in the form of absolute and relative values.
Results
During these years (2017-2019), in the National Cancer Registry were registered 810 primary patients with confirmed histopathological diagnosis of thyroid carcinoma, of which 163 patients were with thyroid cancer associated with autoimmune thyroiditis, 215 have were patients with thyroid cancer developed on a healthy background and 432 patients had thyroid carcinoma developed on the background of other pathologies in Table 1.
Tabelul 1. Dinamica cazurilor de carcinom tiroidian în Republica Moldova (2017 - 2019. Table 1. Dynamics of cases of thyroid carcinoma in the Republic of Moldova (2017 - 2019). | ||||||
| 2017 | 2018 | 2019 | |||
Abs. | % | Abs. | % | Abs. | % | |
Tumori maligne Malignant tumors | 264 | 47,5 | 252 | 33,2 | 238 | 41 |
Din ele: From them: | ||||||
CT + FS CT + FS | 85 | 32,2 | 56 | 22,2 | 74 | 31,1 |
CT + TA CT + TA | 45 | 17 | 49 | 19,4 | 69 | 29 |
CT asociat cu alte boli CT associated with other diseases | 134 | 50,8 | 147 | 58,3 | 95 | 39,9 |
Notă: CT + FS – cancer tiroidian la persoane anterior sănătoase; CT+ TA - cancer tiroidian la pacienți tiroidită autoimună. Note:CT + FS thyroid cancer in patients prevously healphy; CT + TA - thyroid cancer in patients with autoimmune thyroiditis. | ||||||
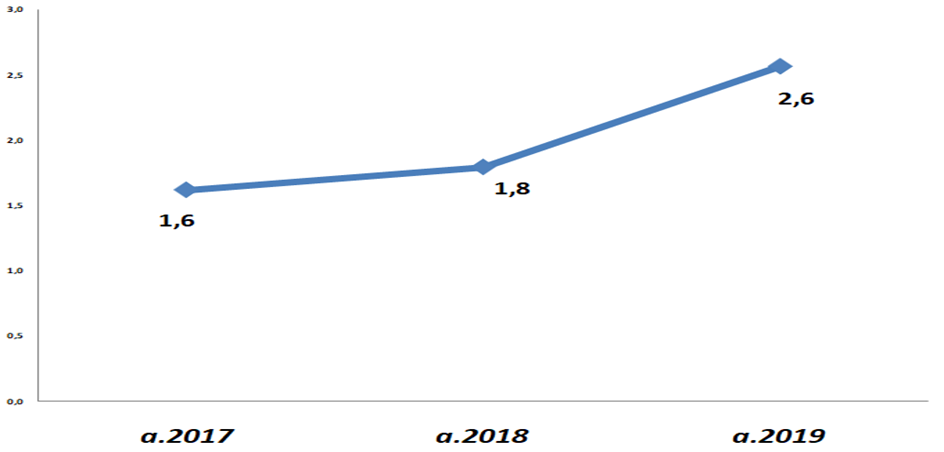
The study included only primary patients, who had as a substrate for healthy background development and association with autoimmune pathology, the latter registering a continuous increase during the years 2017-2019 (Figure 1).
|
Fig. 1 Dinamica cazurilor de carcinom tiroidian asociat cu tiroidita autoimună (incidența la 100 mii populație cu reședință obișnuită). Fig. 1 Dynamics of thyroid carcinoma associated with autoimmune thyroiditis (incidence per 100 thousand population with habitual residence). |
According to the data following the distribution by gender, we observe an identical percentage distribution for the cases included in the CT + TA group in both groups, where female patients predominate, constituting 96,4%, which represents 108 cases, and in the CT + FS group they constitute 80.3%, which represents 98 cases. The ratio of women / men in the CT + TA group constituting 27/1 and, in the CT + FS group 4/1. The gender distribution reveals a higher incidence of the disease in women compared to men, especially in the case of the association of thyroid carcinoma with autoimmune thyroiditis.
Tabelul 2. Repartizarea pacienților incluși în studiu conform vârstei. Table 2. Distribution of patients included in the study according to age. | ||||||
| Lotul CT+TA (Lot I) | Lotul CT+FS (Lot II) | ||||
n=112 | n=122 | |||||
PE+ | % | PE- | % | Abs. | % | |
< 55 ani <55 years | 29 | 52,7 | 29 | 50,9 | 84 | 68,9 |
> 55 ani > 55 years | 26 | 47,3 | 28 | 49,1 | 38 | 31,1 |
Total | 55 | 100 | 57 | 100 | 122 | 100 |
Notă:CT-cancer tiroidian, TA-tiroidită autoimună,FS-fundal sănătos, PE-puncţie ecoghidată Note: CT-thyroid cancer, TA-autoimmune thyroiditis, FS-healthy background, PE-ultrasound-guided puncture | ||||||
According to the data following the distribution by gender, we observe an identical percentage distribution for the cases included in the CT + TA group in both groups, where female patients predominate, constituting 96,4%, which represents 108 cases, and in the CT + FS group they constitute 80,3%, which represents 98 cases. The ratio of women / men in the CT + TA group constituting 27/1 and, in the CT + FS group 4/1. The gender distribution reveals a higher incidence of the disease in women compared to men, especially in the case of the association of thyroid carcinoma with autoimmune thyroiditis.
According to the distribution by living environment, the comparative data are practically identical by lots. In the CT + TA group, from the rural area, came 50 (44,7%) patients from the total, respectively from the urban area 62 (55,2%) cases included in the study. In the CT + FS group, from the rural area, came 55 (45,1%) patients from the total, respectively from the urban area 67 (54,9%) cases included in the study.
Assessing the territorial-administrative region of origin of the patients, a predominance of the inhabitants of the central and southern region of the Republic of Moldova was found among the patients included in the study (Table 3).
Tabelul 3. Repartizarea pacienților conform unității administrativ teritoriale (incidența la 100 mii populație cu reședință obișnuită). Table 3. Distribution of patients according to the territorial administrative unit (incidence per 100 thousand population with habitual residence). | |||
Lotul CT + TA (Lot I) n=112 | Lotul CT + FS (Lot II) n=122 | ||
PE+ | PE- | ||
NORD NORTH | 1,8 | 2,4 | 3,8 |
CENTRU CENTER | 2,5 | 2,1 | 4,7 |
SUD SOUTH | 2,1 | 2,3 | 6,8 |
Notă:CT-cancer tiroidian, TA-tiroidită autoimună,FS-fundal sănătos, PE-puncţie ecoghidată Note: CT-thyroid cancer, TA-autoimmune thyroiditis, FS-healthy background, PE-ultrasound-guided puncture | |||
Discussions
According to the literature, thyroid carcinoma is associated with autoimmune thyroiditis in an average of 1% to 75% of cases. Respectively Dailey, 1955, USA – 12,6%; Siriweera, 2010, Sri Lanka – 9,46%; Kim, 2011, South Korea – 29,9%; Okayasu, 1995, Japan – 46,2-76,0%; Yoon, 2012, South Korea – 28,7%; Consorti, 2010, Italy – 36.2%; Cipolla, 2005, Italy – 27,6% [14-20]. The results of our study show a growing association per year of these pathologies from 17-29%.
Tabelul 4. Repartizarea pacienților în dependență de grupa sanguină. Table 4. Distribution of patients according to blood type. | ||||||
| Lotul CT + TA (Lot I) n = 112 | Lotul CT + FS (Lot II) | ||||
n = 122 | ||||||
PE+ | % | PE- | % | Abs. | % | |
O | 19 | 34,5 | 29 | 50,9 | 43 | 35,2 |
A | 27 | 49,1 | 18 | 31,6 | 40 | 32,8 |
B | 5 | 9,1 | 8 | 14 | 27 | 22,1 |
AB | 4 | 7,3 | 2 | 3,5 | 12 | 9,8 |
Total | 55 | 100 | 57 | 100 | 122 | 100 |
Notă: CT-cancer tiroidian, TA-tiroidită autoimună,FS-fundal sănătos, PE-puncţie ecoghidată Note: CT-thyroid cancer, TA-autoimmune thyroiditis, FS-healthy background, PE-ultrasound-guided puncture | ||||||
Throughout the literature, the highest incidence of thyroid carcinoma is in the second, third and fourth decades of life. However, in the last two decades, there has been an increase in the incidence of thyroid cancer in the fourth and fifth decades of life. Increased diagnosis can be attributed to accidental discoveries of tumors in imaging studies, such as ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET), performed for other reasons, young patients up to 55 years of age also prevailed [13].
An obvious difference between men and women is in terms of sex hormones and their influence on different systems in the body. The fluctuation of sex hormones during a woman's menstrual cycle and pregnancy has been hypothesized as a reason for gender disparity in thyroid cancer [11, 12]. Thyroid cancer had an incidence rate 2.9 times higher in women (female: male ratio 16.3: 5.7-2006) [13]. According to the data of A. Ţîbîrnă in the 2010 study “Epidemiological, clinical-morphological and surgical features of adenoma and thyroid cancer” - the ratio of women / men is 8:1 [5]. The distribution of patients by sex reveals a higher incidence of the disease in women, compared to men, a fact present in the case of the association of thyroid carcinoma with autoimmune thyroiditis - also demonstrated in the present study.
According to A. Ţîbîrnă 's data, in the study conducted in 2010 in the Republic of Moldova, after the distribution of thyroid cancer patients according to the living environment, patients from urban areas prevailed – 63%, this prevalence was observed in the present study.
In order to investigate the incidence of cancer of the thyroid gland in the Republic of Moldova depending on the territorial-administrative unit, these data were analyzed. The distribution of patients according to the territorial administrative unit (incidence per 100 thousand population with habitual residence) reported a higher prevalence of patients from the southern and central region of the country. The study performed by A. Ţîbîrnă in 2010 showed a higher prevalence in the northern and center administrative units of the Republic of Moldova [15].
Conclusions
Thyroid carcinoma associated with autoimmune thyroiditis is on the rise in the Republic of Moldova. This nosology mostly affects young people up to the age of 55 and predominates in females. southern Republic of Moldova. According to the distribution of patients by blood type, we observe a predominance of „O” blood group.
Competing interests
None declared
Author’s ORCID ID
Ina Sclifos -https://orcid.org/0000-0003-3820-559X
References
Globocan 2018 [Internet]. 2019. p. 2018–9. Available from: https://gco.iarc.fr/today/data/factsheets/cancers/32-Thyroid-fact-sheet…
Registrul Naţional de Cancer al Republicii Moldova
Cancerul glandei tiroide , PCN 200 , Chişinău 2013
Трапезникова Н.Н. М., Онкология ,Медицина, 1981
Negri E., Dal Maso L., Ron E. et al. O analiză combinată a studiilor caz-control ale cancerului tiroidian. II. Factori menstruali și reproductivi. Controlul cauzelor cancerului. 1999; 10: 143–155.
Perrier N.D., Brierley J.D., Tuttle R.M. Carcinom tiroidian diferențiat și anaplazic: modificări majore în comitetul mixt american pentru cancer, ediția a opta, manualul de stadializare a cancerului CA Cancer J Clin. 2017; 68: 55-63
Kilfoy B.A., Devesa S.S., Ward M.H. et al. Sexul este un modificator de efect specific vârstei pentru cancerele papilare ale glandei tiroide. Cancer Epidemiol. Biomarkeri Prev. 2009; (18) : 1092–1100.
Rahbari R., Zhang L., Kebebew E. Thyroid cancer gender disparity, Future Oncol, 2010 Nov; 6(11): 1771–1779.
Abbas Ali Tam, Didem Özdemir, Sevgül Fak, Muhammet Cüneyt Bilginer, Reyhan Ersoy, Bekir Çakır Grupurile sanguine ABO, factorul Rh și riscul de cancer al tiroidei: la „B” sau nu la „B” Noiembrie 2019 Cercetare endocrină 45 (2): 1-10.
Dailey M. E., Lindsay S., Skahen R. Relation of thyroid neoplasms to Hashimoto disease of the thyroid gland. AMA Arch Surg, 1955;70: 291–297.
Okayasu I., Fujiwara M., Hara Y., Tanaka Y., Rose N.R. Association of chronic lymphocytic thyroiditis and thyroid papillary carcinoma. A study of surgical cases among Japanese, and white and African Americans. Cancer. 1995;76: 2312–2318.
Kim K.W., Park Y.J., Kim E.H., Park S.Y., Park do J., Ahn S.H., Park do J., Jang H.C., Cho B.Y. Elevated risk of papillary thyroid cancer in Korean patients with Hashimoto's thyroiditis. Head Neck. 2011;33: 691–695.
Yoon Y.H., Kim H.J., Lee J.W., Kim J.M., Koo B.S. The clinicopathologic differences in papillary thyroid carcinoma with or without co-existing chronic lymphocytic thyroiditis. Eur Arch Otorhinolaryngol. 2012;269: 1013–1017.
Cipolla C., Sandonato L., Graceffa G., Fricano S., Torcivia A., Vieni S., Latteri S., Latteri M.A. Hashimoto thyroiditis coexistent with papillary thyroid carcinoma. Am Surg. 2005;71: 874–878.
Teza de doctor în medicina ale d-lui Ţîbîrnă A. Particularităţile epidemiologice, clinico-morfologice şi chirurgicale ale adenomului şi cancerului glandei tiroide, Chișinău, 2010.