Introduction
Osteitis condensans ilii (OCI) is a condition characterized by benign sclerosis of the iliac bone in the portion adjacent to the sacroiliac joints, which is radiologically manifested by triangular opacities at this level. It is usually determined bilaterally, and in very rare cases unilaterally, the diagnosis being established exclusively radiologically [1]. The causes of the disease have not been completely elucidated, however, it is assumed that the influence of mechanical actions and instability (laxity of ligaments) of the sacroiliac joints, causes their overstrain, which is a chronic response to stress. Some sources stipulate that the enlargement of the uterus in size during pregnancies could compress some branches of the iliac arteries, thus causing a transient local ischemia of the distal ileum. It is mainly found in multipara women, but cases have also been encountered in nulliparous women and men. Among the clinical manifestations, localized low back or lumbosacral pain is often attested, which is found in the gestational or post-partum period. The pain may worsen during physical exertion or during menstruation and may be accompanied by myalgia and morning redness. At the objective examination there is pain on palpation of the lumbar region and sacroiliac joints [2]. The data of the laboratory examination do not reveal specific changes, so the markers of inflammation (CRP, ESR) are normal. Also compared to spondylarthritis (SpA), HLA-B27 is negative in most cases [3]. It is important to know about the condition in order to be able to differentiate sacroiliitis from SpA, since both have similar clinical manifestations. Two cases of imaging-diagnosed OCI will be presented, which were initially diagnosed with seronegative spondyloarthritis. Through them, we would determine the varieties between the OIC forms and their differential diagnosis with SpA.
Materials and methods
This article reports three clinical cases of 3 women, who were admitted to the Timofei Mosneaga Republican Clinical Hospital in the Arthrology unit. The clinical and paraclinical data were retrieved from the inpatient medical records (lab tests included CRP, ESR, blood count, HLA-B27, 25-hydroxyvitamin D, rheumatoid factor, anti-nuclear antibodies). According to medical records, the patients were confirmed with osteitis condensans ilii. X-ray of sacroiliac joints and axial skeleton, abdomen ultrasound, neurologist consultation and gastroenterologist-hepatologist consultation, as well as at the specific infectious disease (for reactive arthritis) specialist were carried out.
Results
Clinical case No. 1.
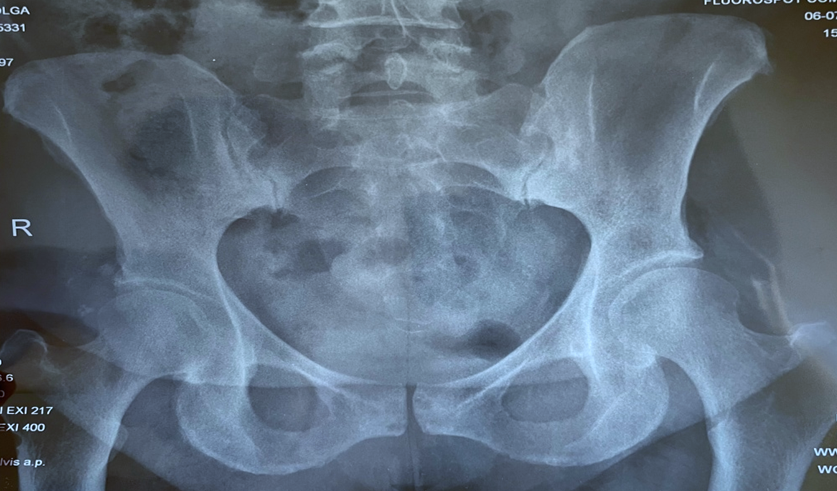
A 48 year-old (multipara, 7 pregnancies, 6 births, 1 medical abortion) woman has addressed to the Timofei Moşneaga Republican Clinical Hospital. The patient is obese, obesity class I according to World Health Organization. The disease started with intense low back pain, immediately after the 5th birth, in 2007. The patient addressed to the neurosurgeon, who excluded radiculopathy and recommended the consultation of the rheumatologist, following treatment with NSAIDs, muscle relaxants, to relieve the symptoms. She administered the treatment, with beneficial effects, the general condition with positive course, so the patient postponed the visit to the rheumatologist. Over the years, migratory joint pain has associated, with a mechanical character. In 2015, patient went to the rheumatologist, was investigated, performed the radiography of the bones of the pelvis and the radiologist described the presence of bilateral sacroiliitis. In 2015, the diagnosis of undifferentiated seronegative arthritis was established, and it was recommended to initiate immunosuppressive treatment with methotrexate 10 mg. The patient administered the DMARD treatment for a short period of time, after which she abandoned it on her own. In 2019 she was hospitalized again to the Timofei Moşneaga Republican Clinical Hospital, due to the worsening of the low back pain and arthralgia, the diagnosis was reassessed, the diagnosis of psoriatic arthritis was assumed given the clinical picture, the radiological image of the pelvis, and the presence of hyperkeratosis in the elbows, plants and nail pitting. It was recommended to resume the DMARD treatment with methotrexate and to consult the dermatologist to specify the diagnosis. The patient neglected the recommendations of the rheumatologist, did not administer treatment, but was periodically hospitalized in the department of internal medicine at the place of living hospital, administered treatment with NSAIDs, muscle relaxants, vascular drugs, while her general condition was satisfactory. In 2021, the patient gave birth to her 6th child, after which the low back pain has worsened again, she had difficulties in performing daily activities and always required a break when walking. Thus, in June 2022, the patient was again hospitalized at the Timofei Moşneaga Republican Clinical Hospital. The laboratory tests excluded the presence of a generalized inflammatory process (table 1). Radiography of the lumbar region and bones of the pelvis was performed (Figure 1), where sclerosis of the subcortical joint surface of the iliac bone, which extends into the adjacent medullary space was outlined. The diagnosis of osteitis condensans ilii was established by clinical and instrumental results and excluding any kind of SpA, it was recommended treatment with NSAIDs, periodically, at the worsening of the dolor syndrome.
Table 1. Laboratory examination data of patient A., a 48-year-old woman | |
Lab indices | Values |
Leukocytes | 7.00 x 103/µL |
ESR | 19 mm/h |
CRP | 3.70 mg/L |
Rheumatoid factor | 7.80 IU/ml |
Anti-nuclear antibodies | 0.4 < 1.0 S/CO |
25-hydroxyvitamin D | 15.8 ng/ml |
HLA-B27 | Negative |
Chlamydia trachomatis – DNA | Negative |
Mycoplasma hominis – DNA | Negative |
Mycoplasma genitalium – DNA | Negative |
Ureaplasma urealyticum – DNA | Negative |
Note: ESR – erythrocyte sedimentation rate, CRP – C-reactive protein, HLA – human leucocyte antigen, DNA – deoxyribonucleic acid. | |
|
Fig. 1. X-ray of the pelvis – clinical case no. 1. The joints surfaces, the articular fissures are congruent, regular coxofemoral joints. In the sacroiliac joints sclerosis of the articular surfaces, unevenly narrowed articular fissures (sacroiliitis grade 2-3). Osteoarthritis in the joint of pubic symphysis with subchondral cystic reconstruction. Entesopathies in the regions of iliac bones. |
Clinical case No. 2.
Patient B., 46 years old, presents with low back pain, which appeared approximately during the 4th birth and became persistent at the onset of menopause. She mentions that they also worsened during the next 2 pregnancies. Patient is known to be multiparous, having 6 children, natural births, 2 of which were postterm births. Physiological menopause set in at the age of 40. She is overweight. According to the patient, she also had migratory peripheral polyarthralgia mainly at the level of the knees, talocrural and plantar joints, which made establishing the diagnosis more difficult. The lab tests were normal (table 2). Objective signs of spinal root damage have not been determined. No limitation has been observed in the hip joints. The X-ray of the pelvis was evaluated to determine the degree of sacroiliitis, but on the image we can definitely see the bilateral congruent, net articular surfaces, with sclerosis of the articular portion of the iliac bone in the form of a triangle, thus excluding the spondyloarthritis (Figure 2), establishing the OCI according to the image, the history of disease and the objective data.
Table 2. Laboratory examination data of patient B., a 46-year-old woman | |
Lab indices | Values |
Leukocytes | 6.82 x 103/uL |
ESR | 5 mm/h |
CRP | 0.09 mg/L |
Rheumatoid factor | 12.60 IU/ml |
Anti-nuclear antibodies | 0.3 < 1.0 S/CO |
25-hydroxyvitamin D | 17.1 ng/ml |
HLA-B27 | Negative |
Chlamydia trachomatis – DNA | Negative |
Mycoplasma hominis – DNA | Negative |
Mycoplasma genitalium – DNA | Negative |
Ureaplasma urealyticum – DNA | Negative |
Note: ESR – erythrocyte sedimentation rate, CRP – C-reactive protein, HLA – human leucocyte antigen, DNA – deoxyribonucleic acid. | |
|
Fig. 2. X-ray of the pelvis – clinical case no. 2. The congruent, net articular surfaces, with sclerosis of the articular portion of the iliac bone in the form of a triangle, bilaterally, thus excluding the spondyloarthritis. |
Clinical case No. 3.
In contrast to these 2 classic cases, we report a patient C. who addressed the Republican polyclinic. The patient aged 43 years, had pain in the lumbosacral region. Physiological history: 3 pregnancies, 2 births, the last pregnancy was stagnant in evolution at 16 weeks. Menstruation is present, regular. From the history of the disease, it is known that the pain syndrome at the level of the lumbosacral region appeared after the third pregnancy in which it presented with a mild urinary infection. Given the fact that the patient is on record at the nephrologist with chronic pyelonephritis, in order to exclude low back pain due to kidney damage, she performed ambulatory US of internal organs and kidneys, excluding the renal diseases. The patient was consulted by the rheumatologist, who has performed physical examination with following signs: no costovertebral tenderness, normal mobility in the preserved hip joints, and lumbar region mobility insignificantly reduced. No other joints changes or swellings were attested. A set of lab tests was recommended, which included the investigation for the presence of urogenital infections, radiography of the lumbar region and pelvis. According to the laboratory results (table 3), the lack of urogenital infections was determined, at the radiography of the lumbar region – without signs of vertebral damage, at the radiography of the pelvis – sclerosis signs of the iliac bone in the shape of a triangle on the right, without affecting the sacroiliac joints, specifically by unilateral OIC (Figure 3).
|
Fig. 3. X-ray of the pelvis – clinical case no.3. Sclerosis signs of the iliac bone in the shape of a triangle on the right, without affecting the sacroiliac joints. |
Table 3. Laboratory examination data of patient C., a 43-year-old woman | |
Lab indices | Values |
Leukocytes | 7.12 x 103/uL |
ESR | 8 mm/h |
CRP | 1.30 mg/l |
Rheumatoid factor | 8.40 IU/ml |
Anti-nuclear antibodies: | 0.1 < 1.0 S/CO |
25-hydroxyvitamin D | 16.9 ng/ml |
HLA-B27 | Negative |
Chlamydia trachomatis – DNA | Negative |
Mycoplasma hominis – DNA | Negative |
Mycoplasma genitalium – DNA | Negative |
Ureaplasma urealyticum – DNA | Negative |
Note: ESR – erythrocyte sedimentation rate, CRP – C-reactive protein, HLA – human leucocyte antigen, DNA – deoxyribonucleic acid. | |
Discussions
In relation to the aforementioned clinical cases, the dependence of this condition on the female sex, on pluriparous and its mechanical action on the bones of the pelvis was highlighted. Taking into account the more frequent description of radiological changes manifested by periarticular sclerosis of bilateral iliac bones, however, there are also cases with imaging and unilateral manifestations, with the same clinical picture mentioned in case no. 3. Among the most common clinical manifestations were the lumbosacral pain, which is triggered mainly by the mechanical action of the fetus on the bones of the pelvis and the laxity of the periarticular ligaments.
The pain worsens with physical exertion and improves at rest, has a localized character, not involving other joints. Often it can be confused with axial spondyloarthritis, due to similar clinical manifestations, but the radiological manifestations are different for these conditions: in the axial spondyloarthritis, the presence of sacroiliitis is attested, characterized by changes in the sacroiliac joints (from the narrowing of the spaces, to ankylosis), in the OIC the sacroiliac joints are not involved, only the iliac bones are involved with their subchondral sclerosis. To differentiate OIC from an axial spondyloarthritis, clinical criteria proposed by the European Spondylarthropathy Study Group (ESSG) are used for the classification of spondylarthropathy. Clinical criteria include a history of inflammatory pain in the spine or synovitis in the lower limbs, along with any of the following: psoriasis, inflammatory bowel disease; alternative buttock pain and enthesopathy or a positive family history of spondylarthropathy. In addition to clinical and imaging manifestations, in laboratory manifestations of patients with OCI, the presence of inflammation or any marker specific to this condition is not attested.
In the management of these patients, treatment with NSAIDs, analgesics and physical therapy was initiated. The effect of which proved to be beneficial after about 2 weeks, with improvement of the local pain syndrome and the general condition of the patients. An equally important therapeutic measure is the weight loss down to normal BMI, also stretching exercises and strengthening of the pelvic muscles caused a decrease in the recurrences of the pain syndrome.
Conclusions
OCI is a condition, which can only be diagnosed radiologically in asymptomatic patients. It is more frequently identified in patients who have low back pain. According to the results of the presented clinical cases, it is often confused with sacroiliitis, which leads to misdiagnosing and the initiation of erroneous treatment methods. Thus, in order to establish a true diagnosis, it is necessary to collect the detailed history, perform a comprehensive physical examination, which includes information regarding the character of the pain and its triggers, the lack of inflammatory indices at the laboratory examination and the radiological presence of the sclerosis areas at the level of the iliac bone, not involving the sacroiliac joints. When the picture is complete, the final diagnosis and therapeutic tactics specific to the condition can be established.
Abbreviations
BMI – body mass index, CRP – C-reactive protein, DNA – deoxyribonucleic acid, ESR – erythrocyte sedimentation rate, HLA – human leucocyte antigen, NSAIDs – non-steroidal anti-inflammatory drugs, OCI – Osteitis condensans ilii, SpA – spondyloarthritis, USG – ultrasonography.
Competing interests
None declared.
Authors’ contributions
The authors contributed equally to the search of scientific literature, the selection of bibliography, the reading, and analysis of biographical references, the writing of the manuscript and its peer review. All authors read and approved the final version of the article.
Authors’ ORCID IDs
Liliana Groppa , https://orcid.org/0000-0002-3097-6181
Marinela Homițchi, https://orcid.org/0000-0002-1357-2388
Valeria Stog, https://orcid.org/0000-0001-6318-4490
Eugeniu Russu, https://orcid.org/0000-0001-8957-8471
Lia Chișlari, https://orcid.org/0000-0002-7088-568X
References
Jenks K, Meikle G, Gray A, Stebbings S. Osteitis condensans ilii: a significant association with sacroiliac joint tenderness in women. Int. J. Rheum. Dis., vol. 12, no. 1, pp. 39–43, Apr. 2009, doi: 10.1111/J.1756-185X.2009.01378.X.
Parperis K, Psarelis S, Nikiphorou E. Osteitis condensans ilii: current knowledge and diagnostic approach. Rheumatol. Int., vol. 40, no. 7, pp. 1013–1019, 2020, doi: 10.1007/s00296-020-04582-9.
Poddubnyy D. et al. Clinical and imaging characteristics of osteitis condensans ilii as compared with axial spondyloarthritis. Rheumatology, vol. 59, no. 12, pp. 3798–3806, Dec. 2020, doi: 10.1093/RHEUMATOLOGY/KEAA175.