Introduction
Ureteropelvic junction obstruction (UPJO) is a well-known clinical entity that represents an obstruction to the urine evacuation from the renal pelvis into the ureter, which, if not properly diagnosed and treated, can lead to the complete loss of function of the affected kidney [1]. It may be caused by intrinsic or extrinsic factors, which may be congenital or acquired. UPJO is most caused by congenital causes that result in primary obstruction of the ureteropelvic junction, but it can also be caused by extrinsic compression by an aberrant vessel or by high ureter insertion [2]. Secondary UPJO can be caused by previous surgeries, recurrent stone passages, or inflammatory diseases [3].
Since its first description, Hynes-Anderson dismembered pyeloplasty has become the standard of surgical treatment for patients with UPJO [4]. The technique includes complete removal of the UPJ and performing with absorbable wires a new, wide anastomosis. A key element of the operations is urinary drainage, which aims to decompress the renal pelvis, maintain the caliber of the ureter, and maintain the anastomotic alignment [5].
There are several methods of urinary drainage described. The external drainage (ED) method involves decompressing the renal collecting system using various catheters externalized through the renal parenchyma, the most used being nephrostomy, uretero-pyelo-nephrostomy, or a combination of both [6]. Internal urinary drainage is accomplished by inserting a double-J (DJ) ureteral stent from the renal pelvis into the urinary bladder [7]. Both DJ and ED have been widely used for many years and have proven their effectiveness during pyeloplasty; however, each method is associated with its advantages and disadvantages [4].
The ED procedure allows for the assessment of the repair in pyeloplasty and, if necessary, allows a pyelography to be performed. They can be simply removed without the need for sedation [8]. However, they have several potential unfavorable conditions, such as increased risk of renal parenchyma damage, bleeding, flank pain, urinary tract infections, and reduced quality of life [4]. In addition, the presence of an external drain increases the risk of urinary infection.
The use of the DJ offers advantages, especially for the postoperative period; it is associated with better cosmetic results and a shorter hospital stay [9]. The disadvantage of this method is the risk of dysuria, suprapubic pain, and terminal hematuria [10, 11].
Most of the publications related to the topic of urinary drainage methods address particular aspects of DJ or ED. There is a lack of data concerning intraoperative or postoperative particularities, postoperative complications, types of complications, and the overall success rate of pyeloplasties in adults comparing two different techniques. A better understanding of all these particularities would allow us to identify the risk factors associated with each method of urinary drainage and, in the end, would help us better plan our surgery and obtain better surgical results.
The aim of the current research was to assess the efficacy and safety of two different types of urinary drainage on adult pyeloplasty.
Material and methods
The retrospective and prospective clinical controlled study was conducted at the Urology Clinic of the “Timofei Mosneaga” Republican Clinical Hospital and the Department of Urology and Surgical Nephrology of the Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova. The research protocol was positively approved by the Research Ethics Committee of Nicolae Testemitanu State University of Medicine and Pharmacy of the Republic of Moldova (Protocol No. 29/54 of 06.05.2014).
We reviewed 118 consecutive adult pyeloplasties for ureteropelvic junction obstruction. The information was gathered from medical records (Form 003/e) with the ICD-10 code N13.0 between 2008 and 2016. The retrospective part included the period between 2008 and 2014; the prospective part included the period between 2012 and 2016. All cases were evaluated clinically and by ultrasound at 6 and 12 months after the surgery.
In all cases, the diagnosis of UPJO was confirmed based on renal ultrasound, intravenous urography, or contrast-enhanced computed tomography. For the standardization and reporting of the pre- and postoperative ultrasound data, we used the Nguyen [12] urinary tract dilatations classification from 2014, as shown in Table 1.
Table 1. Classification of upper urinary tract dilatations. | |
Grade | Imaging aspect |
Grade I | Renal pelvis dilatation |
Grade II | Central and peripheral caliceses dilated |
Grade III | Parenchyme thin |
All patients underwent Hynes-Anderson dismembered pyeloplasty. Depending on the urinary drainage method, all subjects were divided into two groups:
Group I (the DJ group) consisted of 62 (52.54%) patients, in whom we used Double-J ureteral stent insertion.
Group II (the ED group): 56 (47.46%) patients in whom we used different types of external drainage (ED), namely nephrostomy (3.57%, n = 2), uretero-pyelo-nephrostomy (46.42%, n = 26), or a combination of both (48.21%, n = 27).
The following aspects were evaluated: epidemiological data; intraoperative particularities, highlighting operation time and intraoperative complications; postoperative particularities, including the assessment of postoperative hospital stay duration, analgesic consumption, the number and type of postoperative complications, the need for reintervention and hospitalization within the next 12 months, and the overall success rate. Surgical success was defined as the absence of flank pain and the absence of progression of hydronephrosis after 12 months.
PSPP 1.6.2 and MS Excel 2016 were used for statistical data processing, and standard statistical analysis methods were applied. Different statistics were used for group comparisons depending on the type of data. For the frequencies and percentage values, the Pearson χ2 statistic and the degrees of freedom (gl) applicable to the analyzed table were calculated, and based on these values, the p value was deduced. In cases where the minimum conditions of the χ2 test were not met (fewer than 5 observations in one of the cells of the tested table), to confirm the conclusions, the Fisher Exact test was also applied, which does not have such limitations and directly calculates the p value. For the analysis of the quantitative (measured) data, the mean, the standard deviation, the median, and the minimum and maximum values were observed, and the ANOVA (analysis of variance) procedure was applied with the calculation of the F statistic and the deduction of the applicable p-value. The statistical significance threshold was set at the widely accepted level of p < 0.05, but this level was interpreted with caution if p-values were slightly higher.
Results
A general characterization of the study lots is shown in Table 2.
The average age of the patients enrolled in the research was 36.88±14.24 years, with a median of 34 years and values between 18 and 74 years, without a statistically significant difference between the groups, determining the homogeneity of the groups. The mean age in the DJ group was 37.97±14.12 years, ranging from 19 to 74 years; the median was 37 years; in the ED group, the mean age was 35.68±14.39 years, ranging from 18 to 64 years, with a median of 30 years and oscillations between 18 and 64 years. Distribution by age groups also did not identify differences between the researched groups. The distribution by gender identified a slight male predominance of 69.64% (39) in the ED group, compared to 38.71% (24) in the DJ group (x2 = 11.3, gl = 1, p = 0.001). The distribution according to place of residence did not identify statistically significant differences between the researched groups, with residence in an urban environment in the DJ group being 45.16% (28) vs. 41.07% (23) in the ED group, and from rural areas in the DJ group being 54.84% (34) vs. 58.93% (33) in the ED group.
The analysis of the etiology of UPJO identified that in both groups the most frequent cause of UPJO was its congenital obstruction – 59.32% (70), followed by the presence of aberrant vessels – 31.36% (37), without statistically significant differences between the groups, which once again confirmed the homogeneity of the study groups. The results are presented in Table 2.
Most frequently, patients complained of dull pain located in the lumbar region. In the DJ group, this sign was present in 60 (96.67%) patients, and in the ED group, in 55 (98.21%) patients. The left-right location of the disease is presented in Table 2.
Table 2. Comparative analysis of registered parameters according to study groups. | |||
Parameters | DJ group (n = 62) | ED group (n = 56) | p |
Age, years | 37.97±14.12 (19-74) | 35.68±14.39 (18-64) | p > 0.05 |
Grouping by age: | |||
18-30 years, n (%) | 23 (37.10) | 29 (51.79) | p > 0.05 |
31-40 years, n (%) | 12 (19.35) | 6 (10.71) | p > 0.05 |
41-59 years, n (%) | 22 (35.48) | 17 (30.36) | p > 0.05 |
≥ 60 years, n (%) | 5 (8.06) | 4 (7.14) | p > 0.05 |
Grouping by gender: | |||
Men, n (%) | 24 (37.81) | 39 (69.64) | p = 0.001 |
Women, n (%) | 38 (61.29) | 17 (30.36) | p > 0.05 |
Residency: | |||
Urban, n (%) | 28 (45.16) | 23 (41.07) | p > 0.05 |
Rural, n (%) | 34 (54.84) | 33 (58.93) | p > 0.05 |
Etiology of UPJO: | |||
UPJ stenosis, n (%) | 38 (61.29) | 32 (57.14) | p > 0.05 |
aberrant vessel, n (%) | 19 (30.65) | 18 (32.14) | p > 0.05 |
uretero-pelvic implantation defect, n (%) | 1 (1.61) | 5 (8.93) | p > 0.05 |
stenosing periurethritis, n (%) | 1 (1.61) | 0 (0.00) | p > 0.05 |
cicatricial uretero-pelvic retraction, n (%) | 3 (4.84) | 0 (0.00) | p > 0.05 |
combination (uretero-pelvic implantation defect + aberrant vessel) | 0 (0.00) | 1 (1.79) | p > 0.05 |
Clinical picture: | |||
Back pain, n (%) | 60 (96.67) | 55 (98.21) | p > 0.05 |
| 21 (33.87) | 27 (48.21) | p > 0.05 |
| 38 (61.29) | 26 (46.43) | p > 0.05 |
| 3 (4.84) | 3 (5.36) | p > 0.05 |
Degree of hydronephrosis: | |||
II, n (%) | 29 (46.77) | 25 (44.64) | p > 0.05 |
III, n (%) | 33 (53.23) | 31 (55.36) | p > 0.05 |
Note: statistical test applied: Pearson χ2; p – statistical significance; DJ – Double-J; ED – External Drainage; UPJO – ureteropelvic junction obstruction; UPJ – ureteropelvic junction. | |||
All subjects had advanced urinary tract dilatations (as determined by renal ultrasound), with degree II in 45.76% (54) of cases and degree III in 54.24% (64) of cases. Distribution by groups identified that in the DJ group, 29 (46.77%) patients had grade II hydronephrosis and 33 (53.23%) patients had grade III. In the ED group, grade II hydronephrosis was diagnosed in 25 (44.64%) patients and grade III in 31 (55.36%). The results are shown in Table 2.
In 63.56% (75) of the cases, we performed only a pyeloplasty; in another 36.44% (43) of the cases, due to the association of other urological conditions, we also performed some other surgical procedures like stone extraction, nephropexy, and resection of renal cysts or aberrant vessels. In the DJ group, only pyeloplasties were performed in 56.45% (35) of the cases, compared to 71.43% (40) cases in the ED group, and the ratio of more complex interventions was 43.55% (27) to 28.57% (16) cases, with no statistically significant differences between the studied groups, which once again demonstrates their homogeneity.
The mean operative time for all operations was 95.77±20.48 minutes, with 93.52±18.10 minutes in the DJ group and 98.21±22.69 minutes in the ED group. (F = 5.361, p = 0.002; Kruskal-Wallis H = 16.078, gl = 3, p = 0.001). The results are presented in Table 3.
Table 3. Particularities of surgical interventions. | |||
Parameters | DJ group (n = 62) | ED group (n = 56) | p |
Pyeloplasty, n (%) | 35 (56.45) | 40 (71.43) | p > 0.05 |
Pyeloplasty + other operations, n (%) | 27 (43.55) | 16 (28.57) | p > 0.05 |
Mean operative time (min.): | |||
mean | 93.52±18.10 | 98.21±22.69 | p = 0.001 |
median | 90 | 100 |
|
IIQ | 85-105 | 85-120 |
|
Min-Max | 60-140 | 60-150 |
|
Note: statistical test applied: Pearson χ2; p – statistical significance; DJ – Double-J; ED – External Drainage. | |||
The mean postoperative hospital stay for all patients was 11.37±4.26 days, the median being 11 days, with ranges between 4 and 30 days. In the DJ group, it was 8.45±2.02 days on average, with a median of 8 days and values between 4 and 18 days; in the ED group, it was 14.71±3.45 days, the median being 14 days with ranges between 9 and 30 days, this difference being statistically significantly higher (F = 147.851, p = 0.000; Kruskal-Wallis H = 79.388, gl = 1, p = 0.000). The results are presented in Table 4.
Table 4. Duration of postoperative hospitalization (in days). | |||
Parameters | DJ group (n = 62) | ED group (n = 56) | p |
Mean | 8.45±2.02 | 14.71±3.45 | p = 0.000 |
Median | 8 | 14 |
|
IIQ | 7-9 | 13-16 |
|
Note: statistical test applied: Pearson χ2; p – statistical significance; DJ – Double-J; ED – External Drainage. | |||
The analysis of the consumption of non-opioid analgesic medication identified that in the DJ group, the need for drugs was lower than in the ED group (7.77±3.48 vs. 9.86±4.64 administrations) (F = 7.911, p = 0.006). The evaluation of the number of opioid drugs did not identify statistically significant differences between the investigated groups, constituting 2.50±1.24 administrations in the DJ group, and 2.76±1.63 administrations in the ED group. The data are presented in Table 5.
Table 5. Postoperative pain medications (number) | |||
Parameters | DJ group (n = 62) | ED group (n = 56) | p |
Opioid analgesics | |||
mean | 2.50±1.24 | 2.76±1.63 | 2.62±4.18 |
median | 2 | 3 | 2 |
IIQ | 2-3 | 2-3 | 2-3 |
Min-Max | 0-6 | 0-10 | 0-10 |
Non-opioid analgesics | |||
mean | 7.77±3.48 | 9.86±4.64 | 8.77±4.18 |
median | 7 | 9 | 8 |
IIQ | 5-10 | 7-12 | 6-10 |
Min-Max | 2-20 | 3-29 | 2-29 |
Note: statistical test applied: Pearson χ2; p – statistical significance; DJ – Double-J; ED – External Drainage. | |||
The only intraoperative complication (0.85%, n = 1) was significant bleeding that required hemostatic transfusion; it occurred during the extraction of the stone from the renal pelvis, and the patient was from the DJ group.
From the day of surgery until discharge, complications were recorded in 22 (18.64%) patients, of whom 6 (9.68%) were in the DJ group and 16 (28.57%) in the ED group (x2 = 6.925, gl = 1, p = 0.009). From the time of discharge until the end of the follow-up period (12 months), complications were recorded in 3 (2.54%) patients, all of them from the ED group (5.36%, n = 3). Overall, from the day of surgery until the end of the follow-up period, different types of complications were recorded in 20.34% (24) of the cases, of which 9.68% (6) were in the DJ group and 32.14% (18) were in the ED group (x2 = 6.165, gl = 1, p = 0.002). Thus, for patients in the DJ group, the chance of developing postoperative complications was 4.4 times lower compared to those in the ED group (OR = 4.42; CI: 1.61–12.16). The results are presented in Table 6.
Table 6. Complications of the reconstructive interventions. | |||
Parameters | DJ group (n = 62) | ED group (n = 56) | p |
Intraoperative complications, n (%) | 1 (0.85) | 0 (0.00) | p > 0.05 |
Overall postoperative complications, n (%) | 6 (9.68) | 18 (32.14) | p = 0.002 |
Early postoperative complications, n (%) | 6 (9.68) | 16 (28.57) | p = 0.009 |
Late postoperative complications, n (%) | 0 (0.00) | 3 (5.36) | p = 0.065 |
Reinterventions, n (%) | 1 (1.61) | 5 (8.93) | p > 0.05 |
Note: statistical test applied: Pearson χ2; p – statistical significance; DJ – Double-J; ED – External Drainage. | |||
Due to several obstructive complications occurring in the postoperative period, in 5.08% (6) of cases, it was necessary to perform different endoscopic interventions (stent replacement, stent insertion, and ureteral catheter insertion), of which 8.93% (5) occurred in the ED group and 1.61% (1) in the DJ group.
The most frequent postoperative complication was acute pyelonephritis of the operated kidney (12.71%, n = 15); this was recorded in 4.84% (3 cases) in the DJ group and in 21.43% (12 cases) in the ED group (x2 = 7.298, gl = 1, p = 0.007). Postoperative bleeding that required transfusion of blood components was recorded in 3 (2.54%) patients, all of them from group II (MDE) (5.36%, n = 3). Prolonged urinary leakage occurred in 2 (1.69%) patients, all from the ED group (3.57%, n = 2). Renal colic occurred in 2 (1.69%) patients, one in each group (1.61% in DJ and 1.79% in ED). In the DJ group, we also had one case of postoperative wound infection (0.85%), one case of 4-day polyuria (0.85%), and one case of thrombophlebitis (0.85%).
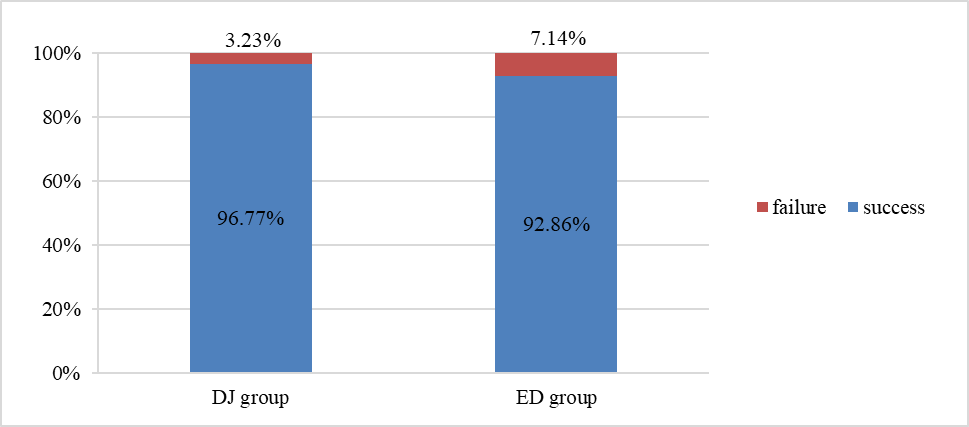
In our study, the overall success rate was 94.92% (112 cases). In 5.08% (6) cases, patients presented flank pain and ultrasound progression of hydronephrosis, so they were considered treatment failures. The DJ group had a success rate of 96.77% (60 cases), while the ED group had a success rate of 92.86% (52). Treatment failure was recorded in 3.23% of the (2) DJ cases and in 7.14% of the (4) ED cases. The results are shown in Figure 1.
Discussions
In this study, we compared the impact of two different methods of urinary drainage on the outcomes of surgical treatment of ureteropelvic junction obstruction in adults. There is consensus that dismembered pyeloplasty is the treatment of choice and standard of care for patients with UPJO. On the other hand, the same cannot be said regarding the method of urinary drainage [7]. The number and quality of studies comparing different methods of urinary drainage in adults are low. Our study seeks to identify the benefits and drawbacks of internal and external urinary drainage methods, as well as their impact on treatment outcomes.
|
Fig. 1 Success rate. Note: DJ – Double-J; ED – External Drainage; success – absence of flank pain and hydronephrosis progression on renal ultrasound examination at 12 months from intervention; failure – presence of flank pain and/or ultrasound progression of hydronephrosis at 12 months from intervention. |
Braga et al. [7] consider that the potential benefits of using a ureteral stent are decreased postoperative urine leakage, alignment of the anastomosis to avoid ureteral kinking, and early discharge from the hospital. On the other hand, the advantages of external methods are the absence of bladder spasms and their easy removal. According to Joshi et al. [13], external methods offer an advantage when it is necessary to evaluate the urinary tract, but they are associated with increased risks of renal parenchyma damage, bleeding, urinary tract infections, back pain, and decreased quality of life. In a network meta-analysis performed by Liu et al. [4], it was found that according to the ranking results, the DJ stenting procedure had the highest operative success rate, renal function improvement, and the shortest hospital stay, while the external stenting method had the lowest rate of overall complications and redo pyeloplasty.
According to our findings, ED is associated with a longer operation time than DJ. It was also demonstrated that ED is associated with a higher requirement for postoperative pain medications; this could be explained by the fact that external drainage is more traumatic, requiring perforation of the renal parenchyma and flank muscles.
The length of hospital stay is an important indicator of morbidity and the economic evaluation of different treatment methods. In our trial, the postoperative length of stay was significantly longer in the ED group than in the DJ group.
Our results have shown that intraoperative complications are not influenced by the urinary drainage method, but a strong association was found between urinary drainage and the number and type of postoperative complications. Early complications were observed more frequently in the ED group than in the DJ group. Late complications were present only in the ED group. The overall complication rate during the past 12 months has shown that the chance of developing postoperative complications in the case of DJ is 4.4 times lower compared to ED.
The most frequent postoperative complication was acute pyelonephritis; it was associated with ED, which could be explained by the renal trauma caused by the trans-parenchymal exteriorization of the drainage tubes and the possibility of their infection.
The overall operative success rate in our study was slightly higher in the DJ group, but without a statistically significant difference, so we can say that both methods are associated with high outcomes and are equal in operative success.
Conclusions
Both urinary drainage methods appear equivalent concerning overall success rates, but double-J ureteral stents are associated with a shorter operating time, fewer postoperative pain medications, a shorter postoperative hospital stay, and a lower number of postoperative complications compared with external urinary drainage methods.
Competing interests
None declared
Authors’s ORCID ID
Alexandru Piterschi, https://orcid.org/0000-0002-7865-0623
References
Jackson L., Woodward M., Coward R. J. The molecular biology of pelvi-ureteric junction obstruction. Pediatr. Nephrol., 2018, Apr; 33 (4): 553-571. doi: 10.1007/s00467-017-3629-0.
Khan F., Ahmed K., Lee N. et al. Management of ureteropelvic junction obstruction in adults. Nat. Rev. Urol. 2014; 11: 629-638. doi: 10.1038/nrurol.2014.240
Tanase A. Urologie şi Nefrologie Chiruricală, 2005; p 51.
Liu X., Huang C., Guo Y. et al. Comparison of DJ stented, external stented, and stent-less procedures for pediatric pyeloplasty: A network meta-analysis. International Journal of Surgery, 68 (2019); 126-133. doi: 10.1016/j.ijsu.2019.07.001
Elafifi M., Eltatawy H., Haroon H., Gaber M. Evaluation of Non-Stented Dismembered Pyeloplasty in Children Suffering from Pelvi-Ureteric Junction Obstruction. Annals of Pediatric Surgery, 2009; 5 (1): 52-57.
Austin P., Cain M., Rink R. Nephrostomy tube drainage with pyeloplasty: Is it necessarily a bad choice? J. Urol., 2000; 163: 1528-30. doi: 10.1016/s0022-5347(05)67671-9
Braga L. H., Lorenzo A. J., Farhat W.A. et al. Outcome analysis and cost comparison between externalized pyeloureteral and standard stents in 470 consecutive open pyeloplasties. J. Urol., 2008 (Suppl); 180: 1693-9. doi: 10.1016/j.juro.2008.05.084
Lee L., Kanaroglou N., Gleason J. et al. Impact of drainage technique on pediatric pyeloplasty: comparative analysis of externalized uretero-pyelostomy versus double-J internal stents. Can. Urol. Assoc. J., 2015; 9 (7–8): E453–E457. Doi: 10.5489/cuaj.2697
Piterschi A. Drenarea căilor urinare superioare în tratamentul chirurgical al stricturilor joncțiunii pielo-ureterale. Anale științifice ale IP USMF „N. Testemițanu”. Zilele Universității, 2015.
Galescu A. Rolul sondelor autostatice „double-J” în tratamentul litiazei reno-ureterale. Analele Științifice ale USMF „N. Testemițanu”, 2011, nr. 4 (12): pp. 195-199. ISSN 1857-1719.
Ghicavîi V., Galescu A., Ceban E. et al. Necesitatea aplicării stentului ureteral după ureteroscopii cu litotriție şi litextracție in litiaza ureterală. Arta Medica, 2011; nr.2S (45): pp. 94-96. ISSN 1810-1852.
Nguyen H., Benson C., Bromley B. et al. Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J. Pediatr. Urol., (2014); 10: 982–99. doi: 10.1016/j.jpurol.2014.10.002.
Joshi H. B., Stainthorpe A., MacDonagh R. P. et al. Indwelling ureteral stents: evaluation of symptoms, quality of life and utility. J. Urol., 2003; 169 (3): 1065-1069; discussion 1069. doi: 10.1097/01.ju.0000048980.33855.90.
Chu D. I., Shrivastava D., Van Batavia J. P. et al. Outcomes of externalized pyeloureteral versus internal ureteral stent in pediatric robotic-assisted laparoscopic pyeloplasty, J. Pediatr. Urol., 2018; 14 (5): 450.e1–450.e6. doi: 10.1016/j.jpurol.2018.04.012.
Nasser F. M., Shouman A. M., ElSheemy M. S. et al. Dismembered pyeloplasty in infants 6 Months old or younger with and without external trans-anastomotic nephrostent: a prospective randomized study. Urology, 2017; 101: 38-44. doi: 10.1016/j.urology.2016.09.024.