Introduction
The discovery of antimicrobial drugs undoubtedly marked a turning point for humanity, changing the course of medicine and offering a new hope for life [1, 2]. Scientists believe this important event in medical history added a decade to human life expectancy [1]. It is known that the human body has its own defense mechanisms against infection, and even if some symptoms occur, a strong immune system can respond effectively and quickly to bacterial infections. However, in certain circumstances, the human body needs assistance to combat infection. In the case of bacterial infections, antibiotics provide that help [2, 3].
Over time, antimicrobial therapy has become increasingly used in the treatment of both confirmed and suspected bacterial infections, as well as for infection prophylaxis in surgical wards, intensive care units, and even pediatric wards [3, 4]. Due to the widespread use of antibiotics, appropriate prescribing has become a key topic among international researchers [2]. International studies on antibiotic prescription practices in hospitalized children indicate that antibiotics are being misused [3]. As a result of antibiotic overuse, many microorganisms have developed resistance through various defense mechanisms, particularly Gram-negative bacteria, which pose a major challenge worldwide [2, 5].
Antimicrobial resistance is associated with ineffective therapies, increased mortality, prolonged hospitalization, and additional costs for both patients and countries [2]. Given the current uncontrolled spread of resistant bacteria, it is imperative to identify the causes of this phenomenon. Numerous international studies have found that a major determinant in the development of resistance is the irrational and uncontrolled consumption of antibiotics within the population [3, 6]. Irrational antibiotic use includes prescribing antibiotics in incorrect doses, self-medication, and the treatment of viral or non-bacterial diseases [3]. It has been estimated that many factors such as politics, economics, doctors' knowledge and experience, diagnostic uncertainty, and pharmaceutical marketing contribute to the irrational use of antibiotics [7].
International research has estimated that patients' high expectations of the therapeutic effects of antibiotics influence their behavior and attitudes towards the use of antimicrobial preparations. Thus, measures to combat the spread of resistant micro-organisms should focus on increasing public awareness of how antibiotics are used, prescribed, and dispensed [4].
The aim of the present study is to assess the general public's knowledge, attitudes, and behavior regarding antibiotic use and to identify the factors associated with irrational antibiotic use.
Material and methods
A cross-sectional study was conducted to assess the general public’s knowledge, attitudes, and behavior regarding the use of antimicrobial preparations in the treatment of infectious diseases. As of January 1, 2021, the population of the Republic of Moldova aged 18 to 74 was 2,619,950. With a sample size of 572 persons, the margin of error at a 95% confidence interval was no more than 4.3%. The sample size was calculated using the following formula:
(1) ![]()
where: z is the z-score, equal to 1.96 for a 95% confidence interval
ε is the margin of error
N is the population size
p is the population proportion (around 60%).
Inclusion criteria for the study population. Adults aged 18 to 74 years were included in the study. Individuals under 18 and over 74 years of age were excluded, as these groups rarely make independent decisions regarding their own health. Informed consent was obtained from each respondent at the beginning of the interview. Participants were selected using a random sampling approach.
Training for research team (interviewers). The research team underwent training in an online session conducted via the Zoom platform by three researchers from the University of Copenhagen. This training covered key aspects of qualitative research methodology, an introduction to qualitative research, and practical sessions. The team consisted of 7 interviewers who were assigned to the selected sites to conduct interviews and collect data between November 8 and November 17, 2022. The team was formed by order number 250-d, issued on November 8, 2022, by the National Agency for Public Health of the Republic of Moldova.
The study utilized a questionnaire developed and validated by the World Health Organization as its primary instrument. This opinion questionnaire featured closed-ended questions, which were administered by interviewers during face-to-face interviews. The survey included dichotomous (Yes/No), multiple choice, and hierarchical questions to comprehensively analyze the knowledge, attitudes, and behaviors of the interviewed population. Data collection was conducted using Android-based tablets, with the questionnaire implemented through KoBoToolbox, a free and open-source suite of tools for mobile data collection.
To conduct this survey, 10 locations in the Chisinau municipality, typically characterized by a higher flow of people, were randomly selected. These locations included bus and trolleybus stops, shopping centers, universities, and medical facilities (Table 1).
Table 1. Locations selected for the survey | |||
Trolleybus and bus stops | Shopping centers | Medical facilities | Universities |
"Construction College" | Gemenii Shopping Center, 136 Stefan cel Mare și Sfânt Boulevard | "Toma Ciorba" Clinical Hospital of Infectious Diseases, 163 Stefan cel Mare si Sfant Boulevard | Nicolae Testemițanu State University of Medicine and Pharmacy, 165 Stefan cel Mare Boulevard |
"Grand National Assembly Square" | Grand Hall Shopping Center, 2/4 Constantin Negruzzi Boulevard | Oncological Institute, 30 Nicolae Testemițanu Street |
|
"House of Press" | UNIC Shopping Center, 8 Stefan cel Mare și Sfant Boulevard | Institute of Cardiology, 29/1 Nicolae Testemițanu Street |
|
The collected data was analyzed using Microsoft Excel (Microsoft, Redmond, Washington) tools. Relative statistical parameters were calculated, specifically the ratio, using the formula:
(2) ) ![]()
Using this formula and raw data, the demographic parameters of the respondents were determined, including: (1) distribution by gender; (2) distribution by age groups; (3) distribution by socio-professional groups. The same principle was applied to analyze the responses to the questionnaire.
The study was confirmed as exempt from review by the WHO Ethics Review Committee (Protocol Number ERC.0003790).
Results
According to the interview location, 25.0% of respondents were interviewed while waiting at bus or trolleybus stops, 39.0% near selected shopping centers, 12.0% in the vicinity of universities, and 24.0% near the mentioned medical institutions.
Females accounted for 60.0% of the respondents, while males comprised 40.0%.
The individuals included in the study were almost evenly distributed across age groups: 21.0% of respondents were aged 18-24 years, 34.0% were in the 25-39 years age group, 25.0% were in the 40-54 years group, and 20.0% were aged 55 years or older.
Respondents were categorized into socio-professional groups based on their primary activity. The largest group consisted of employees performing physical labor (23.0%), followed by students (22.0%), office workers (17.0%), and retired persons (15.0%).
Of all the individuals included in the study, 49.0% reported having taken antibiotics in tablet, powder or syrup form within the past 12 months. In 60.0% of cases, these antibiotics were obtained with a prescription, 21.0% were administered by a healthcare professional, 10.0% were taken from leftover medication from previous treatments, and 7.0% were taken without prescription.
The reasons for using these antimicrobial preparations varied (Fig. 1).
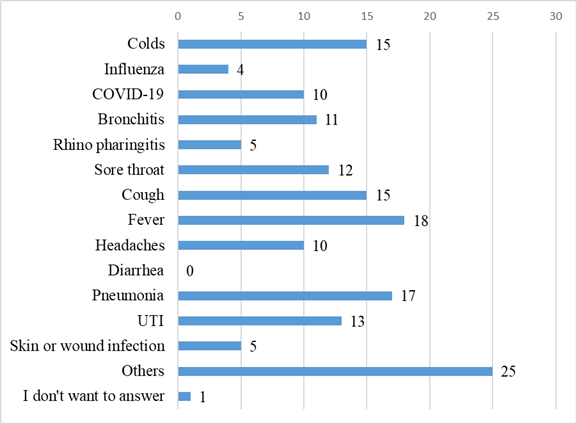 |
Fig. 1. Reason provided by respondents for frequent antibiotic use, % Note: UTI – urinary tract infection |
Most people used antibiotics to manage a fever (18.0%), while 17.0% took antibiotics to treat pneumonia. Additionally, 15.0% used antibiotics for colds and coughs, 13.0% for urinary tract infections, 12.0% for sore throat, 11.0% for bronchitis, and 10.0% for headaches.
In response to the question "Did you have any tests–such as blood tests, urine analysis, or pharyngeal exudate–to determine the cause of the illness before or at the same time as starting antibiotics?", 63.0% answered "Yes,” and 33.0% answered “No”.
To assess the level of knowledge regarding the use of antimicrobials, respondents were asked several general questions about antimicrobial preparations. The statement "Antibiotics kill viruses and are effective against colds" was considered true by 43.0% of respondents and false by 44.0%. Meanwhile, 66.0% agreed with the statement "Using antibiotics when not needed makes them ineffective", and 56.0% identified diarrhea as one of the common side effects of antibiotics.
An interesting pattern emerged when responses to the statement "Antibiotics kill viruses" were disaggregated by age group (Fig. 2).
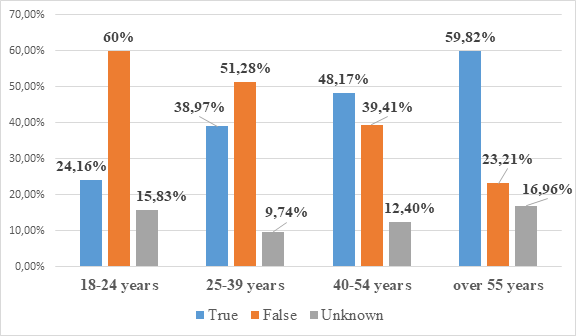 |
Fig. 2. Disaggregation of responses to the statement "Antibiotics kill viruses" by age group, %. Note: The figure illustrates the distribution of “True,” “False,” and “Don't know” answers (blue, orange, and grey columns) among respondents, categorized into age groups: 18-24 years, 25-39 years, 40-54 years, and over 55 years. |
The rate of correct response was higher in age groups under 40 years, which is an important milestone in assessing population knowledge and identifying target groups for public health interventions. Representing more than half of the respondents, an average of 55.64% chose the correct answer to the "trap" question in the survey.
The majority of individuals included in the study (77.0%) believed that antibiotics should be taken until the treatment was completed, while 16.0% were of the opinion that the antimicrobial treatment should last only until the person felt well.
Of the individuals who were advised not to take antibiotics unnecessarily in the past 12 months, 51.0% received this advice from a doctor, 47.0% from the news or other TV programs, 29.0% from online sources, and 19.0% from family members or friends. For 64.0% of respondents, this information was sufficient to change their perspective on antimicrobials. Specifically, they reported: consulting a doctor when they believe they need antibiotic treatment (95.0%); stopping self-medication with antibiotics (49.0%); and not keeping leftover antibiotics for future infections (21.0%).
When asked which sub-topics they would like more information about, most respondents indicated an interest in learning how to prescribe antibiotics (35.2%), followed by antimicrobial resistance (20.5%) and the administration or use of antibiotics (20.0%). In 84.0% of cases, respondents preferred to receive this information from a healthcare worker, while 22.0% favored an official health website, 9.0% mentioned TV, and 8.0% cited relatives and friends.
Among those who had COVID-19, 33.0% had not taken antibiotics to treat the infection, 16.0% had taken antibiotics prescribed by a doctor, and 3.0% had taken antibiotics without a prescription. Slightly more than a third of respondents (32%) reported not having had COVID-19.
To address antimicrobial resistance, 14.0% believe that preventive and control measures should be taken at the individual level, 12.0% at the national level, 15.0% at the global level, and 39.0% think actions should be implemented at all levels.
Discussion
Population knowledge on how to use antimicrobial preparations varies by country/territory, culture, socioeconomic status, education, age, and personality [8].
The main objective of this study was to identify the main factors associated with antimicrobial misuse in order to recommend the development of targeted measures to prevent and control antibiotic resistance [8].
Due to the growing levels of resistance, in 2017, the World Health Organization implemented the first antibiotic release restrictions. Since then, most European countries have developed and approved several regulations in this area [9, 10]. However, the results of the current study, recent studies conducted in Russia, and numerous similar studies in other countries show that dispensing antibiotics in pharmacies without a prescription remains a common practice, for known reasons–primarily the commercial interests of pharmacists or their compassion for the patient's condition [9, 11, 12].
In this context, it is very important to note that such reasons cannot justify a 'fair' policy of marketing antibacterial preparations in contravention of the regulations set by government authorities. International researchers have also reported the results of quantitative studies, which demonstrate the common practice of over-the-counter dispensing of antibiotics in pharmacies [9, 13, 14].
The results of the study showed a moderate level of awareness (63.8%) of antibiotic use, higher than the levels reported by El Zowalaty and Al-Shawi et al. (48.0% and 48.4% respectively) [15, 16].
In this study, 81.0% of the respondents indicated that they had taken antibiotics on prescription, while 18.0% had not been prescribed by a doctor. Among the participants in the study conducted by El Zowalaty, 62.0% took antibiotics for treatment according to a doctor's prescription, and 48.0% took them without a prescription [16].
As in the study by Alnasser et al., the majority of respondents believed that antimicrobial preparations or prescriptions should not be kept for later use and should not be passed on to another person for treatment [17].
The majority of study participants indicated that antibiotics should be discontinued after completing the full course of treatment prescribed by the doctor (77.0%), while 16.0% believed treatment should be stopped when feeling better. This contrasts with 56.8% of participants in the study by Alkhalifah et al., who frequently stopped antibiotics when symptoms improved [18]. Results from other local studies conducted in Riyadh, Saudi Arabia, show that between 48.0% and 67.0% of respondents stopped antibiotics after feeling better [16].
Importantly, a significant proportion of people in the survey have misconceptions about the need for antibiotics. Thus, 43.0% of respondents believe that antibiotics kill viruses, and 48.0% agree that they are effective against colds. These results align with those obtained in the study by Dopelt et al. in 2023, conducted with a group of students at Ashkelon Academic College in Israel, the majority of whom believed that antibiotics could be used to cure a cold, fever, sore throat, and viral infections [19]. Similar results have also been obtained in other research highlighting the problem of a lack of knowledge about antibiotic use [20, 21].
Moreover, these people believe that they should receive antibiotics with their doctor’s prescription whenever they fall ill or use those left over from previous treatment. Such misconceptions are also reflected in the findings of studies by Sambakunsi and Marzan et al. in Malawi and Bangladesh, where many respondents practiced self-medication, including with antibiotics [22, 23].
A significant proportion of participants in a study conducted in Russia believe that antibiotics are generally easy to obtain at any time and can be self-prescribed based on symptoms previously experienced by the person themselves, family members, or friends. In these situations, self-treatment with antibiotics recommended by close individuals is practiced without any medical education background [9]. Similar self-medication practices have been demonstrated in other studies in north-west Russia [12].
In these cases, associated with the irrational use of antibiotics, individuals were unaware of the potential adverse reactions to antimicrobial preparations or the risk of developing bacterial resistance to them.
Another important finding based on the study results was the positive correlation between employment status and appropriate antibiotic use. Thus, the socio-professional status of the interviewee serves as a determinant of antibiotic use. Such observations were also made by Napolitano et al. in a study from Italy, in which unemployed respondents were less informed about antibiotics [24]. Several international studies have shown the relationship between awareness of antibiotic use and antibiotic resistance with the level of education and the presence of children [25], and in a study in Saudi Arabia, appropriate antibiotic use practices were associated with marital status and the presence of children (80% of married participants), explained by more information about antibiotics received during pediatric patients’ treatment [18].
To combat antimicrobial resistance, 14.0% believe that measures to prevent and control this phenomenon should be taken at the individual level, 12.0% at the national level, 15.0% at the global level, and 39.0% believe that actions should be taken at all levels.
It is gratifying that most of the respondents are aware of the impact of AMR on the health of the population and believe that prevention and control measures to combat this phenomenon should be taken at the individual, national, and global levels. Insignificant differences in this respect were found in the study conducted by Rachina et al. in Russia, where less than 10.0% of respondents regarded AMR as a global problem that affects the individual not only at the moment but also as a problem for the future [9]. These results are also consistent with other studies in Germany [26] and Australia [27].
Among the limitations of this study, we mention the cross-sectional study design, which does not allow us to determine causality but only to highlight associations between variables. Also, the survey conducted in urban settings cannot speak to the behavior of rural people or the behavioral patterns of healthcare personnel and policymakers who interact with the general public through awareness-raising activities. Given that it was conducted in one step and in a very short period, our survey was not able to capture internal migration or seasonal changes that affect the epidemiologic environment.
Conclusions
Despite all the regulations regarding the use of antibiotics, common practices of self-diagnosis and self-treatment with antibiotics persist, along with attempts to purchase antimicrobial preparations in pharmacies without a prescription. Moreover, treatment advice often comes from friends or family members who lack any medical education.
The general population has insufficient knowledge about antibiotics and misconceptions about the impact of their irrational use and the role of individual users in the development of bacterial resistance. A lack of clarity about the nature of infections continues to contribute to the inappropriate use of antibiotics – treating different viral or bacterial diseases without prior investigation – and, consequently, to the development of resistance in microorganisms.
Addressing these misconceptions through educational interventions and promoting the responsible use of antibiotics remains a priority in combating antibiotic resistance and ensuring optimal treatment outcomes.
Insufficient knowledge among study participants about the effects and appropriate practices of antibiotic use highlights the need to strengthen awareness-raising measures, as well as to promote effective collaboration between family doctors and pharmacists to ensure the rational use of antibiotics.
The findings of the study emphasize the need for interventions at both the individual and community level through healthcare policies and public education programs. These findings provide insight into the population’s understanding of the phenomenon of resistance, serving as a benchmark for designing interventions aimed at increasing knowledge and awareness of the problem.
Competing interests
None declared.
Authors’ contributions
Conception and design of the work - MA, IOS, MP, VC, EB, OB. Drafting the article - MA, IOS. Reviewing the article for important intellectual content - MA, IOS, OB. All authors critically reviewed the work and approved the final version of the manuscript.
Acknowledgment
No external funding.
Patient consent
Obtained.
Ethics approval
Favorable opinion of the Research Ethics Committee of the Nicolae Testemițanu State University of Medicine and Pharmacy, No. 1, dated September 27, 2022.
Author’s ORCID IDs
Anton Maria – https://orcid.org/0000-0002-4804-7137
Oana-Simina Iaconi – https://orcid.org/0009-0003-3139-7004
Maria Perjeru – https://orcid.org/0009-0007-0849-3902
Valeria Ceban – https://orcid.org/0009-0004-6177-4445
Ecaterina Beleacov – https://orcid.org/0009-0001-1174-4510
Olga Burduniuc – https://orcid.org/0000-0002-6944-0800
References
- Mancuso G, Midiri A, Gerace E, Biondo C. Bacterial antibiotic resistance: the most critical pathogens. Pathogens. 2021;10(10):1310. doi: 10.3390/pathogens10101310.
- World Health Organization. 10 threats to global health in 2018 [Internet]. Medium.com; c2018 [cited 2024 Jun 16]. Available from: https://medium.com/@who/10-threats-to-global-health-in-2018-232daf0bbef…;
- Al-Taani GM, Karasneh RA, Al-Azzam S, et al. Knowledge, attitude, and behavior about antimicrobial use and resistance among medical, nursing and pharmacy students in Jordan: a cross sectional study. Antibiotics (Basel). 2022;11(11):1559. doi: 10.3390/antibiotics11111559.
- Shahpawee NS, Chaw LL, Muharram SH, et al. University students’ antibiotic use and knowledge of antimicrobial resistance: what are the common myths? Antibiotics. 2020;9(6):349. https://doi.org/10.3390/antibiotics9060349.
- Van Hecke O, Butler CC, Wang K, Tonkin-Crine S. Parents' perceptions of antibiotic use and antibiotic resistance (PAUSE): a qualitative interview study. J Antimicrob Chemother. 2019;74(6):1741-1747. doi: 10.1093/jac/dkz091.
- Duan L, Liu C, Wang D, et al. The vicious cycle of the public's irrational use of antibiotics for upper respiratory tract infections: a mixed methods systematic review. Front Public Health. 2022;10:985188. doi: 10.3389/fpubh.2022.985188.
- Bassetti M, Giacobbe DR. A look at the clinical, economic, and societal impact of antimicrobial resistance in 2020. Expert Opin Pharmacother. 2020;21(17):2067-2071. doi: 10.1080/14656566.2020.1802427.
- Baddal B, Lajunen TJ, Sullman MJM. Knowledge, attitudes and behaviours regarding antibiotics use among Cypriot university students: a multi-disciplinary survey. BMC Med Educ. 2022;22(1):847. doi: 10.1186/s12909-022-03853-2.
- Rachina S, Zakharenkova P, Kozlov R, et al. The antibiotic knowledge, attitudes and behaviours of patients purchasing antibiotics with prescription in Russia: a qualitative, comparative analysis. JAC Antimicrob Resist. 2024;6(2):41. doi: 10.1093/jacamr/dlae041.
- Ndaki PM, Mushi MF, Mwanga JR, et al. Dispensing antibiotics without prescription at community pharmacies and accredited drug dispensing outlets in Tanzania: a cross-sectional study. Antibiotics (Basel). 2021;10(8):1025. doi: 10.3390/antibiotics10081025.
- Rachina S, Kozlov R, Kurkova A, et al. Antimicrobial dispensing practice in community pharmacies in Russia during the COVID-19 pandemic. Antibiotics. 2022;11(5):586. https://doi.org/10.3390/antibiotics11050586.
- Cantarero-Arevalo L, Nørgaard LS, Sporrong SK, et al. A qualitative analysis of the culture of antibiotic use for upper respiratory tract infections among patients in Northwest Russia. Front Pharmacol. 2022;13:800695. doi: 10.3389/fphar.2022.800695.
- Zaidi SF, Alotaibi R, Nagro A, et al. Knowledge and attitude towards antibiotic usage: a questionnaire-based survey among pre-professional students at King Saud bin Abdulaziz University for Health Sciences on Jeddah Campus, Saudi Arabia. Pharmacy (Basel). 2020;8(1):5. doi: 10.3390/pharmacy8010005.
- Gunasekera YD, Kinnison T, Kottawatta SA, Silva-Fletcher A, Kalupahana RS. Misconceptions of antibiotics as a potential explanation for their misuse. A survey of the general public in a rural and urban community in Sri Lanka. Antibiotics (Basel). 2022;11(4):454. doi: 10.3390/antibiotics11040454.
- Miyano S, Htoon TT, Nozaki I, Pe EH, Tin HH. Public knowledge, practices, and awareness of antibiotics and antibiotic resistance in Myanmar: the first national mobile phone panel survey. PLoS One. 2022;17(8):e0273380. doi:10.1371/journal.pone.0273380.
- El Zowalaty ME, Belkina T, Bahashwan SA, et al. Knowledge, awareness, and attitudes toward antibiotic use and antimicrobial resistance among Saudi population. Int J Clin Pharm. 2016;38(5):1261-1268. doi: 10.1007/s11096-016-0362-x.
- Alnasser AHA, Al-Tawfiq JA, Ahmed HAA, et al. Public knowledge, attitude and practice towards antibiotics use and antimicrobial resistance in Saudi Arabia: a web-based cross-sectional survey. J Public Health Res. 2021;10(4):2276. doi:10.4081/jphr.2021.2276.
- Alkhalifah HM, Alkhalifah KM, Alharthi AF, Elzahrany YR, Aljuhani MA. Knowledge, attitude and practices towards antibiotic use among patients attending Al Wazarat health center. J Family Med Prim Care. 2022;11(4):1299-1307. doi: 10.4103/jfmpc.jfmpc_1431_21.
- Dopelt K, Amar A, Yonatan N, Davidovitch N. Knowledge, attitudes, and practices regarding antibiotic use and resistance: a cross-sectional study among students in Israel. Antibiotics. 2023;12(6):1028. https://doi.org/10.3390/antibiotics12061028.
- Sakeena MHF, Bennett AA, Jamshed S, et al. Investigating knowledge regarding antibiotics and antimicrobial resistance among pharmacy students in Sri Lankan universities. BMC Infect Dis. 2018;18(1):209. doi: 10.1186/s12879-018-3107-8.
- Sakr S, Ghaddar A, Hamam B, Sheet I. Antibiotic use and resistance: an unprecedented assessment of university students’ knowledge, attitude and practices (KAP) in Lebanon. BMC Public Health. 2020;20(1):535. https://doi.org/10.1186/s12889-020-08676-8.
- Sambakunsi CS, Småbrekke L, Varga CA, Solomon V, Mponda JS. Knowledge, attitudes and practices related to self-medication with antimicrobials in Lilongwe, Malawi. Malawi Med J. 2019;31(4):225-232. doi: 10.4314/mmj.v31i4.2.
- Marzan M, Islam DZ, Lugova H, Krishnapillai A, Haque M, Islam S. Knowledge, attitudes, and practices of antimicrobial uses and resistance among public university students in Bangladesh. Infect Drug Resist. 2021;14:519-533. doi: 10.2147/IDR.S289964.
- Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One. 2013;8(12):e84177. doi: 10.1371/journal.pone.0084177.
- Guo H, Hildon ZJ, Chow A. ”Antibiotics are for everyone, our past and our future generations, right? If antibiotics are dead, we will be in big trouble”: building on community values for public engagement on appropriate use of antibiotics in Singapore. Front Public Health. 2022;10:1001282. doi: 10.3389/fpubh.2022.1001282.
- Schneider S, Salm F, Schröder C, Ludwig N, Hanke R, Gastmeier P. Antibiotikaeinnahme und Resistenzentwicklung–Wissen, Erfahrungen und Einnahmeverhalten innerhalb der deutschen Allgemeinbevölkerung [Antibiotic intake and resistance development - Knowledge, experience and behavior among the German general population]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2016;59(9):1162-1170. https://doi.org/10.1007/s00103-016-2417-5. German.
- McClelland JW, Norris JM, Dominey-Howes D, Govendir M. Knowledge and perceptions of Australian postgraduate veterinary students prior to formal education of antimicrobial use and antimicrobial resistance. One Health. 2021;14:100366. doi: 10.1016/j.onehlt.2021.100366.

