Introduction
Diabetes mellitus (DM) is a complex and heterogeneous syndrome, induced by the genetic or acquired disorder of insulin secretion and/or the resistance of peripheral cells to insulin action, which induces profound changes in protein, carbohydrate, lipid, and hydro-saline metabolism. The mentioned disorders are the basis for the appearance of a wide spectrum of chronic complications, which can affect all tissues and organs [1]. Type 2 DM accounts for over 95% of all diabetes cases worldwide [2] and represents an important and independent cardio-metabolic risk factor.
Prediabetes is the change in carbohydrate metabolism that includes alterations in fasting glucose and/or glucose tolerance [2]. People with prediabetes have a high risk of developing type 2 DM in the future. Additionally, they have an increased risk of developing diabetes complications and cardiovascular disease.
Diabetes currently has no known single cause, but certain factors such as advanced age, obesity, dyslipidemia, a sedentary lifestyle, and genetic factors are implicated in the development of type 2 DM in most populations [3]. Chronic hyperglycemia is associated with long-term microvascular (neuropathy, retinopathy, and nephropathy) and macrovascular (ischemic heart disease, stroke, peripheral vascular disease) complications. In the absence of early diagnosis and effective treatment, DM complications can advance to severe stages [4]. DM comorbidities lead to a substantial decrease in the quality of life, as well as significant socio-economic consequences [5]. According to the 2019 Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) estimates, diabetes was the 8th leading cause of death and disability in the world in 2019 [6]. In 2019, 6.7 million DM-related deaths were reported, which corresponds to one death every 5 seconds. DM is also a major risk factor for ischemic heart disease and stroke, which were estimated by the GBD in 2019 to be the first and second leading causes of global disease burden, respectively [6, 7]. DM represents a substantial burden on health care systems [8, 9], with estimates from the International Diabetes Federation indicating that 537 million people worldwide had diabetes in 2021, resulting in healthcare costs of 966 billion USD [2]. Globally, it is predicted to reach over 1054 billion USD by 2045 [10, 2]. It is considered that 1 in 2 persons with diabetes is undiagnosed [2].
In 2023, the health system in the Republic of Moldova (RM) had records of 131,550 people with DM. It is estimated that 21% of cases are undiagnosed [11]. Data on the prevalence and incidence of DM and prediabetes are limited due to the lack of studies in this direction.
Material and methods
This is the first cross-sectional epidemiological study (Epidemiological study of widespread endocrine pathologies (diabetes, obesity) in the Republic of Moldova and management strategy) that analyzes the prevalence of DM, prediabetes, and dyslipidemia in the population of RM. The data were collected between June 2020 and June 2023 and included 748 people from north, south, and center regions of RM, randomly chosen from the registers of general practitioners (GP). Individuals over 18 years of age who voluntarily expressed their willingness to participate in the study and signed the consent form represented the inclusion criteria. Exclusion criteria were refusal to participate in the study, age up to 18 years, pregnancy, and lactation.
Prior to data collection, written informed consent was obtained from each study participant. Ethical approval was obtained from the Research Ethics Committee of Nicolae Testemițanu State University of Medicine and Pharmacy (Minute 3 from December 28 2020).
The aim of the study was to assess the prevalence of diabetes and obesity in the adult population of RM. The objectives consisted of assessing the spectrum of carbohydrate and lipid metabolism disorders and their association with well-known risk factors for diabetes and obesity, as well as evaluating the nutritional status in the general population of RM.
Social and demographic data (age, sex, marital status, educational level, ethnicity) and behavioral characteristics (smoking, physical activity, nutritional habits), personal or familial history of DM, and comorbidities were collected through face-to-face interviews applying a pre-tested and semi-structured questionnaire.
Anthropometric parameters were measured in each participant using standardized techniques and calibrated equipment. Body mass index (BMI) was calculated by dividing weight in kilograms by the square of height in meters. Obesity, overweight and normal weight were defined as BMI ≥ 30 kg/m2, 25 – 29.9 kg/m2 and 18.5 – 24.9 kg/m2 respectively. Abdominal circumference (AC) was assessed with a centimeter tape at the level of the navel. AC values > 94 cm for men and > 80 cm for women were considered increased, according to WHO [12]. Systolic blood pressure and diastolic blood pressure were measured in a sitting position on the right arm using a calibrated tonometer. Hypertension was defined as systolic blood pressure (SBP) ≥ 140 mmHg and/or diastolic blood pressure (DBP) ≥ 90 mmHg.
Participants were instructed to fast for at least 8 hours prior to laboratory testing. Biological samples of 3–5 ml of venous blood were collected using a simple vacutainer tube. The blood sample was allowed to clot at room temperature and centrifuged at 3000 rpm for 10 minutes and tested in an accredited laboratory. The fasting blood glucose level was determined using the spectrophotometric method, and the hemoglobin A1c (HbA1c) level was determined using the immunoturbidimetric method.
The diagnosis of DM was established based on the diagnostic criteria of the American Diabetes Association: HbA1c ≥ 6.5%, fasting glucose (FG) ≥ 7 mmol/l, blood glucose 2h after the oral glucose tolerance test (OGTT) ≥ 11.1 mmol/l, or the presence of diabetes history reported by the patient. The diagnostic criteria for prediabetes were: HbA1c value between 5.7 and 6.4%, FG – 5.6 – 6.9 mmol/l, blood glucose 2 hours after OGTT 7.8 – 11 mmol/l.
Data quality was ensured by using a pre-tested semi-structured questionnaire, providing training for the data collector, and active involvement of senior research scientists in the data collection process. The questionnaires were checked for consistency, clarity, and accuracy. Physical measurements were taken twice, and in some cases three times, to minimize observer bias in data measurement and recording.
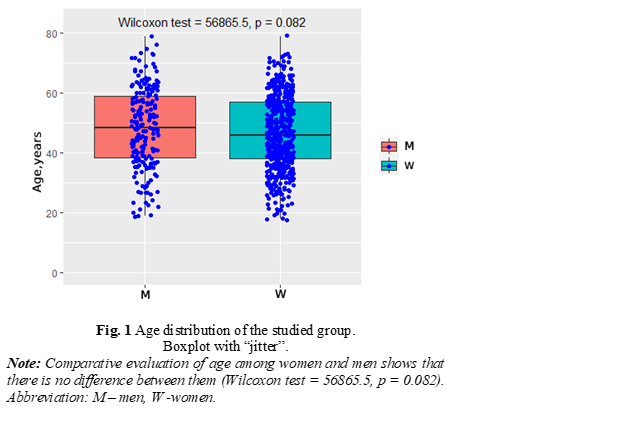
Statistical analysis was performed using RStudio (R-4.3.2 for Windows. The R-project for statistical computing), an integrated development environment for the R programming language. Descriptive statistics for numerical data included mean and standard deviation, categorical data being presented as absolute and relative frequencies, completed by 95% confidence intervals. Comparative evaluation among the groups for continuous features was performed by Wilcoxon non-parametric test for two independent groups. Spearman's rank correlation test was used as a measure for estimated associations. For all mentioned statistical tests, the type I error rate was considered as 0.05.
Results
So far, 748 people have participated in the study, and 728 people from 7 municipalities and districts of the Republic of Moldova, randomly chosen from the registers of GPs, were included in the data analysis. 20 people (2.7%) were excluded from the study due to incomplete data. Of the 728 people, 198 were men and 530 were women, with an average age of 47.14±12.65 years (Fig. 1).
Only 23.2% of men and 30.4% of women had a BMI within the normal range, 41.4% of men and 33.8% of women had a BMI within the range of 25 – 29.9 kg/ m2, which corresponds to overweight. In the group of people with BMI corresponding to class I obesity (30 – 34.9 kg/m2), there were 24.7% men and 20.6% women. Class II obesity (BMI 35 – 39.9 kg/m2) was present in 8.6% men and 8.9% women, and BMI > 40 kg/m2, corresponding to class III obesity, was determined in 0.5% men and 2.6% women (Tab. 1).
Table 1. Body mass index in the investigated persons, absolute number (%). | ||||
|---|---|---|---|---|
Variable | M, n = 198 | 95% CI | W, n = 530 | 95% CI |
BMI, kg/m2 |
|
|
|
|
<18.5 | 3 (1.5%) | 0.39% - 4.7% | 20 (3.8%) | 2.4% - 5.9% |
18.5-24.99 | 46 (23.2%) | 18% - 30% | 161 (30.4%) | 27% - 35% |
25-29.99 | 82 (41.4%) | 35% - 49% | 179 (33.8%) | 30% - 38% |
30-34.99 | 49 (24.7%) | 19% - 31% | 109 (20.6%) | 17% - 24% |
35-39.99 | 17 (8.6%) | 5.2% - 14% | 47 (8.9%) | 6.7% - 12% |
>40 | 1 (0.5%) | 0.03% - 3.2% | 14 (2.6%) | 1.5% - 4.5% |
Note: BMI – Body mass index, M – Men, W – Women, CI – Confidence Interval. | ||||
AC greater than 94 cm (men) and 80 cm (women) was present in 73.7% of men and 76% of women. AC values greater than 102 cm and 88 cm in men and women, respectively, which correspond to abdominal obesity, were determined in 39.4% of men and 53.8% of women (Tab. 2).
Variable | M, n = 198 | 95% CI | W, n = 530 | 95% CI |
|---|---|---|---|---|
Table 2. Abdominal circumference in the investigated persons, absolute number (%). | ||||
Abdominal circumference, cm |
|
|
|
|
< 80 cm (W) and < 94 cm (M) | 52 (26.3%) | 20% - 33% | 127 (24.0%) | 20% - 28% |
80-88 cm (W), 94-102 cm (M) | 68 (34.3%) | 28% - 41% | 118 (22.3%) | 19% - 26% |
> 88 cm (W), > 102 cm (M) | 78 (39.4%) | 33% - 47% | 285 (53.8%) | 49% - 58% |
Note: M – Men, W – Women, CI – Confidence Interval | ||||
A positive correlation was determined between BMI and age (Spearman's rank correlation rho=0.2/0.3, in men/women, p < 0.01), as well as between AC and age (Spearman's rank correlation rho=0.44/0.31 in men/women, p < 0.001).
The number of DM cases diagnosed for the first time during the study was 2.5% (18 people), with an equal gender distribution, while 21.4% of the participants had prediabetes, with a gender distribution as follows: 28.3% (56) men and 18.9% (100) women. A positive correlation was determined between the increased value of blood glucose and age (Spearman's rank correlation rho=0.33/0.35, men/women, p < 0.01) in both sexes.
The risk of developing DM, assessed using the FINDRISC questionnaire, was found to be reduced (<7) in 64 (32.3%) men and 180 (34.0%) women. Slightly increased risk (7-11) was present in 77 (38.9%) men and 172 (32.5%) women. Moderately increased risk (12-14) was present in 30 (15.2%) men and 74 (14.0%) women, and high risk in 20 (10.1%) men and 90 (17.0%) women. 7 (3.5%) men and 14 (2.6%) women fell into the very high risk category (FINDRISC >20).
Discussion
This is the first epidemiological study that analyzes the prevalence of DM, prediabetes, and dyslipidemia in the population of RM. At this stage of the study, 2.5% of new cases of DM were detected. The prevalence of prediabetes was 21.4%, positively correlated with age, being higher in men, similar to the data reported in other studies [13, 14].
The PREDATORR study, led by M. Moța et al., reported similar data regarding the number of new cases of diabetes – 2.4%, and the prevalence of DM – 11.6% [15]. The prevalence of prediabetes was 16.5% in the Romanian population, which is lower compared to the results reported in our study (21.4%). In 2021, the IDF reported a 10 % global prevalence of DM and 6% on average for the European Union (EU). According to the same source, the prevalence of DM in RM is 5.6% [2].
Obesity is a disease with a major negative impact on health. Obesity predisposes to a wide range of diseases that are often interconnected, leading to an increased risk of simple (two comorbid diseases) and complex (four or more comorbid diseases) multimorbidity in these individuals, compared to healthy-weight individuals [16]. Abdominal obesity is one of the main components of metabolic syndrome [17] and is an independent risk factor for various non-communicable diseases, such as cardiovascular disease, type 2 DM, hypertension, and cancer [18, 19]. AC is associated with cardiovascular and all-cause mortality [20]. At the same time, AC is a simple anthropometric measurement that can be easily performed in resource-limited settings and could help screen for cardiometabolic risk [21]. In our study, the prevalence of abdominal obesity was higher among women (76% versus 73.7%) and increased with age, similar to reports from other countries [20, 22].
This study has strengths and limitations. The strengths are the large sample size and the fact that all biochemical analyses were performed in the same certified laboratory. Selection bias is the limitation of the study.
Diabetes mellitus and obesity are a burden on the health system due to the complications of these diseases and associated pathologies, such as major cardiovascular events, debilitating complications, and high costs of hospitalization and treatment. Campaigns aimed at preventing diabetes and obesity must be enforced at the national level alongside general strategies for non-communicable diseases that share similar risk factors. These programs should address key risk factors: promoting healthy eating and physical activity, reducing excess weight, cessation of smoking, and reducing alcohol consumption.
Conclusion
Our study showed an increased prevalence of carbohydrate metabolism disorders, including prediabetes, as well as a high prevalence of abdominal obesity. DM is significantly associated with universally recognized risk factors: overweight, obesity, and dyslipidemia. Persons with unknown diabetes mellitus have been identified. Therefore, targeting strategies to control and prevent modifiable risk factors associated with DM and prediabetes through health promotion measures can contribute to reducing the prevalence and complications of DM. Further studies are needed to appreciate the real extent of the diabetes epidemics.
Competing interests
None declared
Patient consent
Obtained.
Ethics approval
This study was approved by the Research Ethics Committee of Nicolae Testemițanu State University of Medicine
and Pharmacy (Minutes 3 from December 28th, 2020).
Authors’ contribution
SV, ID, AS, LV conceived and participated in the work design. SV, ID, VF, SBG, TA, CP drafted the article. OA performed the statistical analysis. SV, AS, OA, LV critically reviewed the article for important intellectual content. All the authors contributed to the acquisition of data, reviewed the work critically, and approved the final version of the manuscript.
Funding
The study was supported by a Governmental project, code number 20.80009.8007.29.
Authors’ ORCID IDs
Stela Vudu - https://orcid.org/0000-0002-0377-9131
Ina Dușa - https://orcid.org/0009-0004-4629-3184
Oleg Arnaut - https://orcid.org/0000-0002-5483-8672
Aristia Șeremet - https://orcid.org/0000-0003-2377-5928
Vlada Furdui - https://orcid.org/0000-0002-2232-3236
Stela Bacinschi-Gheorghiță - https://orcid.org/0009-0004-7306-6593
Tatiana Ambros - https://orcid.org/0009-0005-8435-1135
Diana Munteanu - https://orcid.org/0009-0001-3797-797X
Carolina Piterschi - https://orcid.org/0009-0002-5459-1013
Lorina Vudu - https://orcid.org/0000-0002-7481-3843
References
- Anestiadi Z, Vudu L, Alexa Z, et al.; [Ministry of Health of the Republic of Moldova]. Diabetul zaharat necomplicat: protocol clinic naţional, PCN-33 [Uncomplicated diabetes mellitus: national clinical protocol, PCN-33]. Chisinau: The Ministry; 2019. Available from: https://msmps.gov.md/wp-content/uploads/2021/02/PCN-33-DZ.pdf. Romanian.
- Magliano D, Boyko E; International Diabetes Federation. Diabetes Atlas [Internet]. 10th ed. Brussels: IDF; 2021 [cited 2023 May 12]. Available from: https://diabetesatlas.org/atlas/tenth-edition/
- Goldenberg R, Punthakee Z. Definition, classification and diagnosis of diabetes, prediabetes and metabolic syndrome. Can J Diabetes. 2013;37 Suppl 1:S8-S11. doi: 10.1016/j.jcjd.2013.01.011.
- Olokoba AB, Obateru OA, Olokoba LB. Type 2 diabetes mellitus: a review of current trends. Oman Med J. 2012;27(4):269-273. doi: 10.5001/omj.2012.68.
- Boyle JP, Honeycutt AA, Narayan KM, Hoerger TJ, Geiss LS, Chen H, Thompson TJ. Projection of diabetes burden through 2050: impact of changing demography and disease prevalence in the U.S. Diabetes Care. 2001;24(11):1936-1940. doi: 10.2337/diacare.24.11.1936.
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-1222. doi: 10.1016/S0140-6736(20)30925-9.
- Emerging Risk Factors Collaboration; Sarwar N, Gao P, Seshasai SR, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215-2222. doi: 10.1016/S0140-6736(10)60484-9.
- Squires E, Duber H, Campbell M, Cao J, Chapin A, Horst C, Li Z, Matyasz T. Health care spending on diabetes in the U.S., 1996–2013. Diabetes Care. 2018;41(7):1423-1431. doi: 10.2337/dc17-1376.
- Afroz A, Alramadan MJ, Hossain MN, et al. Cost-of-illness of type 2 diabetes mellitus in low and lower-middle income countries: a systematic review. BMC Health Serv Res. 2018;18(1):972. doi: 10.1186/s12913-018-3772-8.
- Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022 Jan;183:109119. doi: 10.1016/j.diabres.2021.109119.
Biroul Național de Statistică al Republicii Moldova [National Bureau of Statistics of the Republic of Moldova] [Internet]. Chisinau; 2023. Available from: https://statbank.statistica.md/PxWeb/pxweb/ro/30%20Statistica%20sociala….
- World Health Organization. Waist circumference and waist-hip ratio: report of a WHO expert consultation [Internet]. Geneva: WHO; 2008 [cited 2023 March 14]. Available from: https://www.who.int/publications/i/item/9789241501491.
- Sociedade Portuguesa de Diabetologia [Portuguese Society of Diabetology]. Diabetes: factos e números, Portugal 2014: Relatório Anual do Observatório Nacional da Diabetes [Diabetes: facts and numbers, Portugal 2014: Annual Report of the National Diabetes Observatory]. Lisbon; 2014. Available from: https://spd.pt/images/od_2014.pdf. Portuguese.
- Soriguer F, Goday A, Bosch-Comas A, Bordiú E, Calle-Pascual A, Carmena R, Casamitjana R. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the [email protected] Study. Diabetologia. 2012 Jan;55(1):88-93. doi: 10.1007/s00125-011-2336-9.
- Mota M, Popa SG, Mota E, Mitrea A, Catrinoiu D, Cheta DM, Guja C. Prevalence of diabetes mellitus and prediabetes in the adult Romanian population: PREDATORR study. J Diabetes. 2016 May;8(3):336-44. doi: 10.1111/1753-0407.12297.
- Kivimäki M, Strandberg T, Pentti J, Nyberg ST, Frank P, Jokela M, Ervasti J. Body-mass index and risk of obesity-related complex multimorbidity: an observational multicohort study. Lancet Diabetes Endocrinol. 2022;10:253-63. doi: 10.1016/S2213-8587(22)00033-X.
Alberti KGM, Zimmet P, Shaw J. Metabolic syndrome: a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469-480. doi: 10.1111/j.1464-5491.2006.01858.x.
Choi D, Choi S, Son JS, Oh SW, Park SM. Impact of discrepancies in general and abdominal obesity on major adverse cardiac events. J Am Heart Assoc. 2019 Sep 17;8(18):e013471. doi: 10.1161/JAHA.119.013471.
Sahakyan KR, Somers VK, Rodriguez-Escudero JP, Hodge DO, Carter RE, Sochor O, Coutinho T, Jensen MD, Roger VL, Singh P, Lopez-Jimenez F. Normal-weight central obesity: implications for total and cardiovascular mortality. Ann Intern Med. 2015 Dec 1;163(11):827-35. doi: 10.7326/M14-2525.
Sun Y, Liu B, Snetselaar LG, Wallace RB, Caan BJ, Rohan TE, Neuhouser ML, Shadyab AH. Association of normal-weight central obesity with all-cause and cause-specific mortality among postmenopausal women. JAMA Netw Open. 2019 Jul 3;2(7):e197337. doi: 10.1001/jamanetworkopen.2019.7337.
Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, Santos RD, Arsenault B. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020 Mar;16(3):177-189. doi: 10.1038/s41574-019-0310-7.
Wong MCS, Huang J, Wang J, Chan PSF, Lok V, Chen X, Leung C, Wang HHX, Lao XQ, Zheng ZJ. Global, regional and time-trend prevalence of central obesity: a systematic review and meta-analysis of 13.2 million subjects. Eur J Epidemiol. 2020 Jul;35(7):673-683. doi: 10.1007/s10654-020-00650-3.