Introduction
Dento-maxillary anomalies are characterized by growth and development disorders, primary or acquired, of the dental system or maxillary bone bases major imbalances in the dento-alveolar and occlusal arches [1].
The form-function correlation throughout the individual's life can play a significant role in the etiological process of occlusal anomalies. If function can influence the growth of the jaws, then a change in function can cause the dento-maxillary anomaly. The growth of the upper and lower jaw in the transverse plane is achieved at a variable rate, with periods of intense activity and relative rest [2]. According to several authors, the activity of the medio-sagittal suture continues up to the age of 9 years, being achieved through the mechanism of apposition and resorption. Boboc G. finds an increase of 0.5 mm/year without a difference between the sexes in the anterior area, though for boys, it is higher in the posterior area [3]. The acceleration of the transverse development process occurs around the age of 4-6 years, manifested by the appearance of spacing in the upper and lower front teeth. After the age of 10, changes in the transverse plane are minimal, and for the maxilla, growth continues up to 16 years for boys and 12-13 years for girls. According to Moyers R., there is an increase of 4 mm in the maxilla. He also states that during tooth eruption, the jaws develop in the transverse plane due to the vertical growth of the alveolar processes [4].
The Pont index assesses the transverse development of the dental arches by relating the arch’s dimensions to the size of the teeth, or when normal facial development maintains a certain proportion between the dimension of the arches and the dimension of the face. Currently, the most widely used method for assessing the development of the arches, especially the upper one, is the analysis of the total space (according to Tweed) [5, 6].
The frequency of division 1 of class II is high, ranging between 55 - 70%, depending on the age of the patients, which is significantly higher than division 2, representing only 9% of the total number of malocclusions [7, 8]. The narrowing of the upper jaw is one of the common pathologies, both as an independent malocclusion and as a component element of a basic dentomaxillary anomaly. Snaghina N. G. (1966) reports an incidence of 63.2% in her orthodontic practice. Along with the upper jaw, the upper dental arch usually narrows [9]. In all clinical cases of compression of the upper jaw, it is necessary to perform a biometrical analysis model to assess the degree of compression, both at the premolars and upper molars levels. This facilitates the assessment of an individual treatment plan [10].
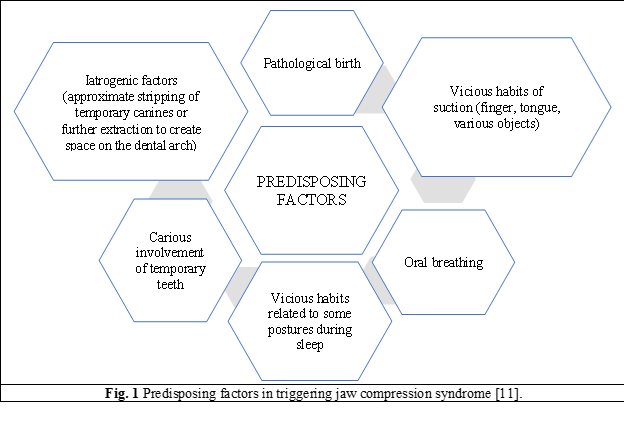
In addition, the phenomenon of delayed eruption in hypothyroidism can cause developmental disorders with the narrowing of the arches, and the insufficiently developed muscle tissue can have a harmful impact on the development of the jawbones. It is unanimously accepted that the genesis of the deformity is included in the diagnosis and provides important data for it. Jaw narrowing cannot be reduced to a single cause and effect, according to the Cause – Time – Tissue – Results equation (the Dockrell orthodontic equation) [12, 13]. The longitudinal growth study by Bolton and Harris determined the heritable component in skeletal traits. Up to 4 years, certain palatal features show a strong genetic determination, it decreases with age, whereas the heritability of craniofacial features increases, with vertical ones being more influenced by the genotype than the horizontal ones [14-16].
Table 1. Longitudinal growth analysis according to Bolton analysis [17] | ||
Age | Craniofacial parameters | Arch and occlusion parameters |
4 | 0.6 | 0.5 |
14 | 0.9 | 0.2 |
20 | 0.9 | 0.1 |
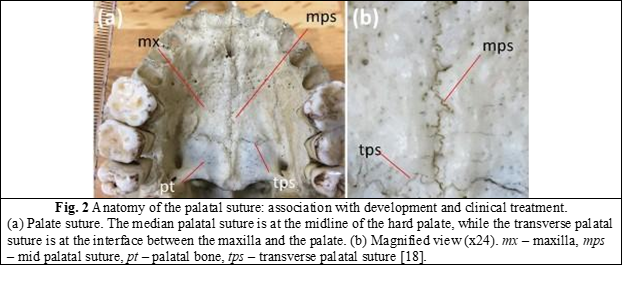
The median palatine suture serves as the growth center for the maxilla. Either inadequate growth in this segment, such as excess or deficiency, causes malocclusions and/or tooth crowding. However, the pattern formation mechanism of palatal sutures, such as the sagittal or median suture, is poorly understood. The palatine suture is the suture between the left and right maxilla and the palatine bone. It is composed of a median palatal suture, present in the middle maxillary region, and a transverse palatal suture that forms the border between the palatine bone and the maxillary bone pictured in figure 2. Most of the surface of the hard palate is made up of the maxilla, so the transverse palatal suture is in the posterior third of the hard palate [18, 19]. The morphology and development of the palatine suture were initially described by direct observation of bone specimens and later by radiographic observations. In forensics, the palatal suture is an age indicator, similar to the calvarial suture [18].
The stages of midpalatal suture fusion were initially described by Angelieri based on standardized cross-sectional cone beam computed tomography (CBCT) images. The radiographic appearance of the midpalatal suture early in life has been noted as a line or area of high density just prior to interdigitation and sutural fusion. The following descriptive stages of the maturation of the middle palatal suture are proposed in figure 3 [19].
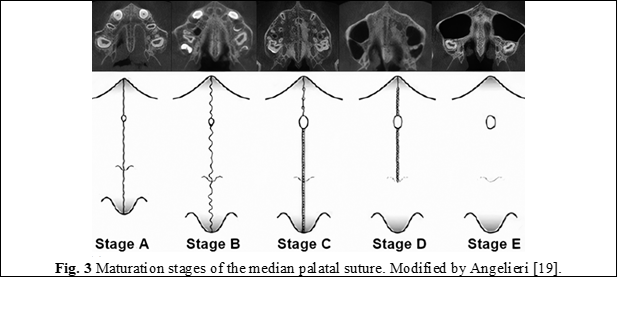
In stage A, the palatal suture is almost a straight suture line of high density, with little or no interdigitation. In stage B, the median palatal suture becomes irregular in shape and appears as a scalloped high-density line. Stage B patients may also have some small areas where 2 parallel, scalloped, high-density lines are seen close together and separated by low-density spaces. In stage C, the midpalatal suture appears as 2 parallel, scalloped, high-density lines that are close to each other, separated by small low-density spaces in the maxillary and palatine bones (between the incisive foramen and the maxillary-palatine suture and posterior to the suture palatomaxillary). The suture can be arranged either straight or irregularly. In stage D, fusion of the midpalatal suture has occurred with the palatine bone, with maturation progressing from posterior to anterior. In the palatine bone, the median palatal suture cannot be visualized at this stage and the bone density is increased. In the maxillary portion of the suture, fusion has not yet occurred, and the suture can still be seen as 2 high density lines separated by small low-density spaces. In stage E, fusion of the midpalatal suture in the maxilla has occurred. The actual suture is not visible in at least one portion of the jaw. The bone density is the same as in other regions of the palate [20-22].
Material and methods
The study, conducted at the department of orthodontics and at “Calfa Dentˮ dental clinic was based on data from clinical and paraclinical examinations, along with diagnostic methods. The study included 165 patients with compression syndrome of the upper jaw aged between 7-18 years, from both rural and urban areas of the country.
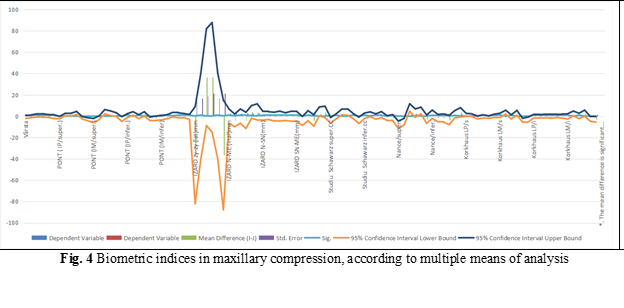
Patients were examined paraclinically by CBCT. This diagnostic method is an important complementary test in the diagnosis and planning of orthodontic treatment. In daily practice, the analysis of the dental and alveolar arches is used, but not the analysis of the dentofacial skeletal parameters, as shown in figure 4. The determination of the skeletal parameters of the upper jaw is the basic factor for the selection of the treatment method of patients with endoalveolia of the upper jaw, both for the dento-alveolar form and the skeletal form.
The most common modification in the reduction of the transverse dimension is the narrowing of the jaw. The genetic damage to the arches is correlated with the damage to the entire process of growth in width and manifests itself in both arches, sometimes with quite pronounced narrowing. The upper arch is more influenced by external factors; environmental factors have the potential to alter growth and affect normal overall development.
The inclusion criteria for CBCT were constituted by asymmetric deformities of the jaws (maxillary retromicrognathia, retrognathia, inferior promacrognathia), crossed occlusion, developmental deviations of the maxilla from the mandible no more than 5 mm transversely, mesialized occlusion, distalized occlusion, jaw narrowings. Exclusion criteria for CBCT: concomitant pathologies, bone tissue pathologies, unsatisfactory hygiene. The Profile Teleradiography (TRG) analysis determined the degree of narrowing of the upper jaw, the inclination of the group of lateral teeth, the level of formation of the median suture. Based on establishing the differential diagnosis, two clinical forms were highlighted, with protrusion and with crowding. The following variants have been proposed for the form with protrusion: Chase's biproalveolodontia, protrusion characteristic of periodontal disease, endocrine disorders (namely hypothyroidism). For the crowding form: absolute/relative macrodontia and generalized mesioposition.
Results
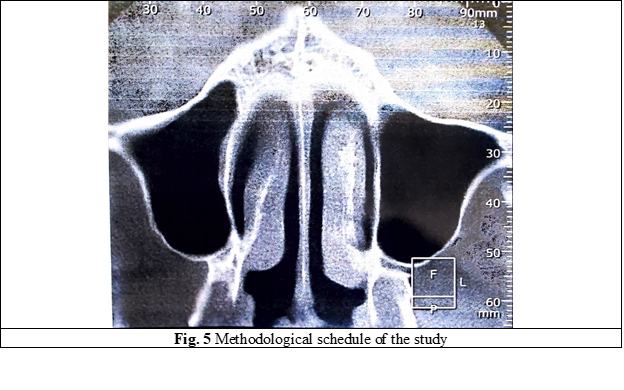
Radiological analysis of the median suture before and after treatment revealed expansion of the palatal suture, as shown in figure 5. Transverse dento-alveolar arch widening was achieved with a hypercorrection for the subsequent arrangement of the position of the lower lateral teeth and the achievement of multiple fissure-cuspid contacts, creating space for the eruption of upper permanent teeth and removing crowding of upper front teeth. In this work group, the activation speed of the expansion device was insignificant because the median suture was in the initial phase of mineralization and its realization occurred both at the dental and skeletal levels. Some commonly used orthodontic treatment techniques for the upper arch include slow jaw expansion, rapid jaw expansion, and surgically assisted rapid jaw expansion. Slow jaw expansion requires light and steady force, while fast jaw expansion requires high and steady pressure to activate. Surgically assisted rapid maxillary expansion has gradually become popular to correct transverse maxillary hypoplasia. Maxillary expansion has various consequences on the nasomaxillary complex.
Discussion
There are multiple effects of maxillary expansion on the nasomaxillary complex, particularly having a direct effect on the median palatine suture along with the palate, maxilla, mandible, temporomandibular joint, soft tissue, and maxillary anterior and posterior teeth [23]. The optimal treatment plan is established based on the complementary paraclinical examination (CBCT), namely: the analysis of the palatal suture, the calculation of the transverse offer of the maxilla and the adjacent anatomical reports [24]. At the same time, based on the CBCT, the capacity in millimeters of the movement that can be performed following the disjunction of the upper jaw can be established, regardless of the type of expansion. This is because the teeth subjected to compression have an increased root angulation, a fact that indicates the need to apply a movement preferably of tilting, not of translation as was usual before [25].
Conclusions
Maxillary compression syndrome is a clinical manifestation often encountered in orthodontic practice, whether as stand-alone malocclusion according to German classification or as clinical component of the class II malocclusion by Angle. Only based on a complex paraclinical examination and correct interpretation we can establish the definitive diagnosis of this clinical entity and indicate a correct treatment plan that will minimize recurrence. Therefore, CBCT is the best investigative method in the assessment of upper jaw compression, because it provides complex information across all 3 reference planes and also helps in the correct interpretation of the palatal suture, which is key to therapeutic success in treating this type of malocclusion.
Competing interests
None declared.
Contribution of authors
SC, VT, IS, AMS drafted the manuscript and realized the literature search, VT, SC designed the study and revised the manuscript critically, SC and IS drafted the manuscript and AMS revised the manuscript critically. All authors have read and approved the final version of the article.
Ethical statement and patient consent
No approval was required for this study.
Funding
The study had no external funding.
Authors’ ORCID IDs
Sabina Calfa – https://orcid.org/0000-0001-5332-738X
Valentina Trifan – https://orcid.org/0000-0003-2398-7410
Iulian Storojov – https://orcid.org/0009-0009-8377-6237
Ana-Maria Șeptelici – https://orcid.org/0009-0001-9418-8934
References
Trifan V, Lupan I, Trifan D, Calfa S. Morbiditatea prin anomaliile dento-maxilare în Republica Moldova [Morbidity by dental-maxillary anomalies in the Republic of Moldova]. Medicina Stomatologica. 2015;(1/34):47-52. Romanian.
Gowri Sankar S, Viswapurna P, Venkata RV. Textbook of orthodontics. New Delhi: Paras Medical Publisher; 2016. 788 p.
Boboc G. Anomaliile dento-maxilare [Dento-maxillary anomalies]. Bucharest: Editura Medicala; 1981. p. 207-212. Romanian.
Moyers RE, Riolo ML, Guire KE, Wainright RL, Bookstein FL. Differential diagnosis of class II malocclusions. Am J Orthod. 1980;78(5):477-94. doi: 10.1016/0002-9416(80)90299-7.
Mitchell L. Introduction to orthodontics. 4th ed. Oxford: Oxford University Press; 2013. 306 p.
Zegan G. Ortodonție și ortopedie dento-facială: tehnici contemporane [Orthodontics and dento-facial orthopedics: contemporary techniques]. Iași: PIM; 2012. 383 p. Romanian.
Shayani A, Sandoval Vidal P, Garay Carrasco I, et al. Midpalatal suture maturation method for the assessment of maturation before maxillary expansion: a systematic review. Diagnostics (Basel). 2022;12(11):2774 [cited 2022 Nov 13]. Available from: https://www.mdpi.com/2075-4418/12/11/2774
Liu S, Xu T, Zou W. Effects of rapid maxillary expansion on the midpalatal suture: a systematic review. Eur J Orthod. 2015 Dec;37(6):651-5. doi: 10.1093/ejo/cju100.
Снагина Н.Г. Определение степени тесного положения зубов в раннем периоде сменного прикуса с использованием биометрического метода исследования. Стоматология. [Determination of the degree of narrow tooth position in the early period of overbite with the use of a biometric method of research. Dentistry]. 1983;5:41-43.
Cantarella D, Dominguez-Mompell R, Mallya SM, et al. Changes in the midpalatal and pterygopalatine sutures induced by micro-implant-supported skeletal expander, analyzed with a novel 3D method based on CBCT imaging. Prog Orthod. 2017 Nov 1;18(1):34. doi: 10.1186/s40510-017-0188-7.
Hussain U, Ayub A, Farhan M. Etiology and treatment of midline diastema: a review of literature. Pakistan Orthod J. 2013;5(1):27-33 [cited 2023 Jun 11]. Available from: https://www.researchgate.net/publication/351132522_Etiology_and_treatment_of_midline_diastema_a_review_of_literature
Bazargani F, Feldmann I, Bondemark L. Three-dimensional analysis of effects of rapid maxillary expansion on facial sutures and bones. Angle Orthod. 2013 Nov;83(6):1074-82. doi: 10.2319/020413-103.1.
Gkantidis N, Kolokitha OE, Topouzelis N. Management of maxillary midline diastema with emphasis on etiology. J Clin Pediatr Dent. 2008 Summer;32(4):265-72. doi: 10.17796/jcpd.32.4.j087t33221771387.
Leonardi R, Cutrera A, Barbato E. Rapid maxillary expansion affects the spheno-occipital synchondrosis in youngsters. A study with low-dose computed tomography. Angle Orthod. 2010 Jan;80(1):106-10. doi: 10.2319/012709-56.1.
Higurashi N, Kikuchi M, Miyazaki S, Itasaka Y. Comparison of Ricketts analysis and Downs-Northswestern analysis for the evaluation of obstructive sleep apnea cephalograms. Psychiatry Clin Neurosci. 2001 Jun;55(3):259-60. doi: 10.1046/j.1440-1819.2001.00850.x.
Isfeld D, Lagravere M, Leon-Salazar V, Flores Mir C. Novel methodologies and technologies to assess mid-palatal suture maturation: a systematic review. Head Face Med. 2017 Jun 14;13(1):13. doi: 10.1186/s13005-017-0144-2.
Enache AM. Anomalia clasa II/1 Angle cu îngustarea arcadei superioare. Etipatogenie și clinică [Class II/1 Angle malocclusion with upper jaw compression. Etiopathogeny and clinics]. Bucharest. 2005 ARS Docendi; Bucharest, Romania. Romanian.
Shibusawa N, Endo Yoshie, Morimoto N, Takahashi I. Mathematical modeling of palatal suture pattern formation: morphological differences between sagittal and palatal sutures. Sci Rep 2021; 11: 8995. Published online 2021 Apr 26. doi:10.1038/s41598-021-88255-y
Angelieri Fernanda, Cevidanes L, Franchi L, Goncalves J, Benavides E. Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2013 Nov; 144(5): 759-769. doi: 10.1016/j.ajodo.2013.04.022
Grunheid T, Larson C, Larson B. Midpalatal suture density ratio: a novel predictor of skeletal response to rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2017 Feb;151(2):267-276. doi: 10.1016/j.ajodo.2016.06.043.
Buzatu R, Nagib R, Dincă M, Vâlceanu A, Szuhanek A. Midpalatal suture morphology and bone density evaluation after orthodontic expansion: a cone-bean computed tomography study in correlation with aesthetic parameters. Rom J Morphol Embryol. 2018;59(3):803-809.
Gonzálvez Moreno AM, Garcovich D, Zhou Wu A, Alvarado Lorenzo A, Bernes Martinez L, Aiuto R, et al. Cone Beam Computed Tomography evaluation of midpalatal suture maturation according to age and sex: a systematic review. Eur J Paediatr Dent. 2022 Mar;23(1):44-50. doi: 10.23804/ejpd.2022.23.01.08.
Reis L, Ribeiro R, Farinazzo R, Reis H, Devito K. Classification of the midpalatal suture maturation in individuals older than 15 years: a cone beam computed tomographic study. Surg Radiol Anat. 2020 Sep;42(9):1043-1049. doi: 10.1007/s00276-020-02518-3.
Caprioglo A, Fastuca R, Zecca P, Beretta M, Mangano C. Cellular midpalatal suture changes after rapid maxillary expansion in growing subjects: a case report. Int J Mol Sci. 2017 Mar 11;18(3):615. doi: 10.3390/ijms18030615.
Christovam I, Lisboa C, Vilani Lemes G, Bodart Brandao R, Mattos C, et al. Tomographic analysis of midpalatal suture prior to rapid maxillary expansion. Dental Press J Orthod. 2021 Jun 30;26(3):e2119300. doi: 10.1590/2177-6709.26.3.e2119300.oar.