Introduction
Visual field is considered the area perceived by one or both eyes while focusing a stationary point. There are two methods of evaluating the visual field: static perimetry and kinetic perimetry. In our research, static perimetry has been used, based on stationary light stimuli projected on the inside of the dome of various sizes and with variable light intensities. The program represents a predefined number of light stimuli (between 50 and 100) projected in different areas of the visual field (Field) that are projected in different variants (Strategy). The neuroanatomy and neurophysiology of the visual pathway is the key to the clinical understanding of visual field examination. The afferent visual pathway begins at each eyeball and undergoes the perception of visual stimuli to the cortex. Along the pathway, this stimulus will pass through the area of the optic chiasm, the optic tract, the lateral geniculate body and the optic radiation so that at the end the image is projected on the occipital cortical visual center in area 17/V1 (also known as the cerebral retina).
Suchoff I. B. mentions that visual field deficits are quite often observed after a traumatic brain injury (TBI). Usually, their presence signals a severe TBI, but they can be detected in the case of a moderate TBI with the involvement of optic chiasm damage or because of a posttraumatic neuropathy [1].
Ciuffreda K. J. et al. attests that visual field defects usually refer to certain sectors, which are missing or appear to be sensory suppressed following the effect of trauma on the primary visual pathways. These areas can range from hemianopsia to small regions of reduced sensitivity. In these cases, the symptoms can vary widely, starting with severe vision difficulties to minor visual effects. Visual field deficits were identified in 35% of patients with visual changes after TBI [2, 3]. Certain patients could benefit from using embedded prisms, such as Fresnel or Peli prisms [2, 4]. The training should include the stimulation with light targets of both the deficient sector and the entire visual field. Some programs are designed to enhance the visual field by stimulating cortical function. They achieve this by training patients to recognize visual field deficits as accurately as possible and even to adjust the orientation of their eyes towards these deficits [2, 5].
The visual pathway consists of a sensory chain made up of types of 4 neurons, three of which originate in various layers of the retina.
The first type of neurons corresponds to the basal layer of photoreceptors: 120 million rods, which predominate in the peripheral retina triggering a person's scotopic vision, and 6.5 million cone cells in the central area for photooptic vision. Most perimeters today use a brightness of 3-10 cd/m, adjusted to the photopic range, which exclusively tests the functional state of the photoreceptor cells.
The second type of neurons corresponds to the middle retinal layer represented by bipolar cells. At the periphery of the retina, a bipolar cell is considered to receive information from several photoreceptor cells, while the one located in the central part transmits information to a single receptor. This is why in neurological lesions, the evaluation of the visual field (VF) in the central 30 degrees is considered much more informative and objective.
The third type of neurons refers to the inner layer of ganglion cells that forms the optic nerve fascicle through its axons.
The fourth type of neurons begins with 4-5 million axons in the lateral geniculate body, joining it after passing through the optic radiation with the occipital cortical visual center [6-11].
The correspondence between the stimulated retinal area and its projection on the area of the visual field is always inverted: the temporal quadrants of the VF correspond to the nasal retina, and the nasal quadrants correspond to the temporal retina. This rule also applies to the lower and upper quadrants.
One of the screening strategies that can be used, according to literature data, is a rapid assessment method that allows for the detection of the presence, position, and size of absolute and relative defects exceeding 6dB depth [12, 13]. It divides all points into three categories:
Flawless
Defect (relative scotoma)
Absolute defect (scotoma).
According to recent studies, the credibility indices do not present a determined value in pediatric population. Thus, the alteration of the fixation capacity (CF) is determined to be: for the age range 5-10 years at 45.5%, ages 11-14 years at 20.18% and for 15-18 years at 31.3%. The evaluation of false positive points (FP) was determined to have the following distribution: for 5-10 years at 11.72%, for ages 11-14 years at 3.82% and for 15-18 years at 5.4%. The evaluation of false negative points (FN) was determined: for 5-10 years at 9.88%, for ages11-14 years at 5.88% and for 15-18 years at 6.44% [14]. On the other hand, some authors stipulate that these indicators could be referred to less strict values, resulting from the analysis of only high-quality results. Thus, we could use ranges of less than 20% for CF, less than 33% for FP and less than 33% for FN [14]. In our research, three reference intervals were evaluated with the following distribution: results up to 20%, results between 21-60% and respectively 61-100% in order to determine the most credible reference values in pediatric patients after TBI.
Materials and methods
Our research was carried out through the clinical evaluation of 96 patients aged between 7-18, hospitalized in the Department of Neurosurgery of the Mother and Child Institute, Natalia Gheorghiu National Scientific-Practical Center for Pediatric Surgery. Patients were evaluated 5-7 days after trauma occurrence, as their general state did not allow performance of the visual field examination. Most of the patients 39.6% revealed a mild traumatic brain injury resulted from a fall from height (54.2%) or a traffic accident (31.2%). Regarding the neurological status, it can be mentioned that 58.3% presented neuropathies, 20.8% coordination problems and 25% of the patients had tremor in the upper and lower limbs. In addition, children that have been included in the research underwent an ophthalmological evaluation that outlined that 83.3%-89.6% of patients revealed a visual acuity ranged between 0.09-0.5 units for the Snellen chart associated with a slight hyperopia of +3.00D in 93.7% - 95.8%. Upper gaze disturbances have been recorded in 58.3%, stereoscopic function alteration in 20.9% and a clear ophthalmoscopic picture in 45.9% patients.
The evaluation has been performed using the Rodenstock perimeter. The screening strategy was chosen because it is a summary method, providing light stimuli above the expected threshold level at all visual field test points. Patients have been asked to concentrate on the red flash point in the middle of the examination area in order to have a better fixation. All external sound and visual stress factors have been excluded, as the examination has been undergone in partial darkness conditions. The Standard Field Test, encompassing an evaluation of 12 points within a 30-degree field, stimulus color of green at 570 nm and a background of 10 abs with automatic level control. After a period of 4 months, the evaluation was repeated in order to outline changes in the researched parameters. Given that pediatric patients are often poorly cooperative, several breaks were scheduled, in order to avoid possible errors.
In order to achieve research objectives, a cohort study was conducted.
Research inclusion criteria.
L1 batch eligibility criteria:
School-aged children who present visual disorders after TBI.
No organic pathology of the visual analyzer.
Patients without other associated chronic pathology.
L0 batch eligibility criteria:
School-aged children who present visual disorders with no TBI.
No organic pathology of the visual analyzer.
Patients without other associated chronic pathology.
Results
Visual field examination was performed in both groups, revealing some visual field deficits in patients after TBI. The results of this examination indicated a lack of fixation among the patients in the research group. Specifically, for the right eye, in 89.6% (43 patients) the loss of fixation fluctuated between 61-100%, in 8.3% (4 patients) this value was up to 20%, and in 2.1% (1 patient) values ranged between 21%-60%. In the control group, the loss of the fixation of the right eye was observed in 68.7% (33 patients) - in the range of up to 20%, in 23% (11 patients) in the range of 61-100% and in 8.3% (4 patients) in the range of 21-60% (p < 0.001).
For the left eye, the results indicated a lack of fixation among patients in the research group: 91.6% (44 patients) experienced a loss of fixation in the range of 61%-100%, and 4.2% in the range of 21%-60% while 4.2% up to 20%, compared to the values for the left eye in the control group: 70.8% (34 patients) in the range of up to 20%, in 25% (12 patients) in the range of 21-60%, and 4.2% (2 patients) in the range of 61%-100% (p < 0.01) (tab. 1).
Evaluation of the ability to fixate on false positive points increased indices in both eyes among children in both the research group and in the control group, primarily values up to 20%, with a higher number in the control group. For the right eye 83.3% in the control group versus 45.8% in the research group, and for the left eye, 70.8% in the control group versus 43.8% in the research group (p < 0.05).
Table 1. Fixation loss ratio after brain injury in children aged between 7-18 years (96 patients). | |||||
Eye | Values | L1 | L0 | ||
Patients | % | Patients | % | ||
Right | Up to 20% | 4 | 8.3 | 33 | 68.7 |
21%-60% | 1 | 2.1 | 4 | 8.3 | |
61%-100% | 43 | 89.6 | 11 | 23 | |
p < 0.01 | |||||
Left | Up to 20% | 2 | 4,2 | 34 | 70,8 |
21%-60% | 2 | 4,2 | 12 | 25 | |
61%-100% | 44 | 91,6 | 2 | 4,2 | |
p < 0.001 | |||||
Note: L1 – research batch; L0 – control batch; Applied statistical test Fisher’s test. | |||||
Meanwhile, it should be noted that the ability to fixate false positive points in the patients of the research group for the interval 21-60% was observed in 22.9% versus 12.5% in the control group, and the interval of 61-100% - 31.3% patients in the research group versus 4.2% in the control group (tab. 2) (p < 0.001). For the left eye, the range 21-60% was noted with practically the same frequency among both the patients of the research group and the patients of the control group (22.9% versus 20.8%). Moreover, the rate of the ability to fixate false positive points in the range of 61-100% in the left eye noted a slight upward trend among the patients of the research group: 33.3%, compared to 8.3% in the control group (p < 0.05).
Table 2. False positive points fixation after brain injury in children aged between 7-18 years (96 patients). | |||||
Eye | Values | L1 | L0 | ||
Patients | % | Patients | % | ||
Right | Up to 20% | 22 | 45.8 | 40 | 83.3 |
21%-60% | 11 | 22.9 | 6 | 12.5 | |
61%-100% | 15 | 31.3 | 2 | 4.2 | |
p < 0.001 | |||||
Left | Up to 20% | 21 | 43.8 | 34 | 70.8 |
21%-60% | 11 | 22.9 | 10 | 20.8 | |
61%-100% | 16 | 33.3 | 4 | 8.3 | |
p < 0.05 | |||||
Note: L1 – research batch; L0 – control batch; Applied statistical test Fisher’s test. | |||||
The evaluation of the ability to fixate false negative points did not reveal significant statistical differences between the researched groups. Thus, in both the research and the control group, the majority of patients (> 91% of cases) for both eyes, presented values up to 20%, specifically for the right eye: 95.8% in the research group and91.7% in the control group (p < 0.05), and for the left eye: 93.7% in the research group and 97.9% in the control group (p < 0.05) (tab. 3).
Table 3. False negative points fixation after brain injury in children aged between 7-18 years (96 patients). | |||||
Eye | Values | L1 | L0 | ||
Patients | % | Patients | % | ||
Right | Up to 20% | 46 | 95.8 | 44 | 91.7 |
21%-60% | 1 | 2.1 | 3 | 6.2 | |
61%-100% | 1 | 2.1 | 1 | 2.1 | |
p < 0.05 | |||||
Left | Up to 20% | 45 | 93.7 | 47 | 97.9 |
21%-60% | 1 | 2.1 | 1 | 2.1 | |
61%-100% | 2 | 4.2 | 0 | 0 | |
p < 0.05 | |||||
Note: L1 – research batch; L0 – control batch; Applied statistical test Fisher’s test. | |||||
The structural defects index (SD) represents numerical values of the elevation levels present in the area of the visual field. This index can only take a positive value, and if it is numerically higher, it indicates the presence of changes in the topography of the visual field. The SD index indicated values between < 0dB, 3dB>, which would signify a smooth visual field without irregularities, in 62.5% (30 patients) -L1 and 91.6% (44 patients) - L0 for the right eye. Levels in the < 3dB, 9dB > range were recorded in 35.4% (17 patients) - L1 and 6.2% (3 patients) - L0 respectively. The maximum range of 9dB> reached equal values for both groups of 2.1% (1 patients) - L1 and 2.1% (1 patients) - L0 (p < 0.001). For the left eye, the following values were determined: the range of < 0dB, 3dB > in 70.8% (34 patients) - L1 and 95.8% (46 patients) - L0. The range < 3dB, 9dB > was attributed to 27.1% (13 patients) - L1 and 4.2% (2 patients) - L0 (p < 0.001). Maximum values of >9dB were determined only in the research group – 2.1% (1 patient) (tab. 4).
Table 4. Structural defect index after brain injury in children aged between 7-18 years (96 patients). | |||||
Eye | Values | L1 | L0 | ||
Patients | % | Patients | % | ||
Right | < 0 dB. 3dB> | 30 | 62.5 | 44 | 91.6 |
< 3 dB. 9 dB> | 17 | 35.4 | 3 | 6.2 | |
9 dB> | 1 | 2.1 | 1 | 2.1 | |
p < 0.001 | |||||
Left | < 0 dB. 3dB> | 34 | 70.8 | 46 | 95.8 |
< 3 dB. 9 dB> | 13 | 27.1 | 2 | 4.2 | |
9 dB> | 1 | 2.1 | 0 | 0 | |
p < 0.001 | |||||
Note: L1 – research batch; L0 – control batch; Applied statistical test Fisher’s test. | |||||
Another evaluated criterion would be the index of average defects, which represent the numerical differences from the standard values correlated to age. This index can be positive or negative, where a negative value indicates decreased sensitivity, and a positive value indicates increased sensitivity compared to reference numbers. The distribution of the average elevation demonstrated a more accentuated depressive tendency of the visual field in the research group. For the right eye the reference range was < -6dB, -3dB > 47.9% (23 patients), followed by the range of -6dB> for 39.5% (19 patients) and < -3dB, 3dB > for 12.5% (6 patients). Compared to the control group, these indices were mainly in the range < -3dB, 3dB > for 54.1% (26 patients), followed by the range < -6dB, -3dB > for 34.4% (17 patients) and respectively -6dB> for 10.4% (5 patients) (p < 0.001). For the left eye, the value distribution was very similar to the right eye, with the following values determined for the research group: range < -6dB, -3dB> for 56.2% (27 patients), followed by the range of -6dB> for 22.9% (11 patients) and < -3dB, 3dB > for 20.8% (10 patients) (p < 0.001). Compared to the control group: range < -3dB, 3dB > for 56.2% (27 patients), followed by range < -6dB, -3dB > for 37.5% (18 patients) and respectively -6dB> for 6. 2% (3 patients) (tab. 5).
Table 5. Index of average defect after brain injury in children aged between 7-18 years (96 patients). | |||||
Eye | Values | L1 | L0 | ||
Patients | % | Patients | % | ||
Right | < -3 dB. 3dB > | 6 | 12.5 | 26 | 54.1 |
< -6 dB. -3 dB > | 23 | 47.9 | 17 | 34.4 | |
-6 dB> | 19 | 39.5 | 5 | 10.4 | |
| |||||
Left | < -3 dB. 3dB > | 10 | 20.8 | 27 | 56.2 |
< -6 dB. -3 dB > | 27 | 56.2 | 18 | 37.5 | |
-6 dB > | 11 | 22.9 | 3 | 6.2 | |
Note: L1 – research batch; L0 – control batch; Applied statistical test Fisher’s test. | |||||
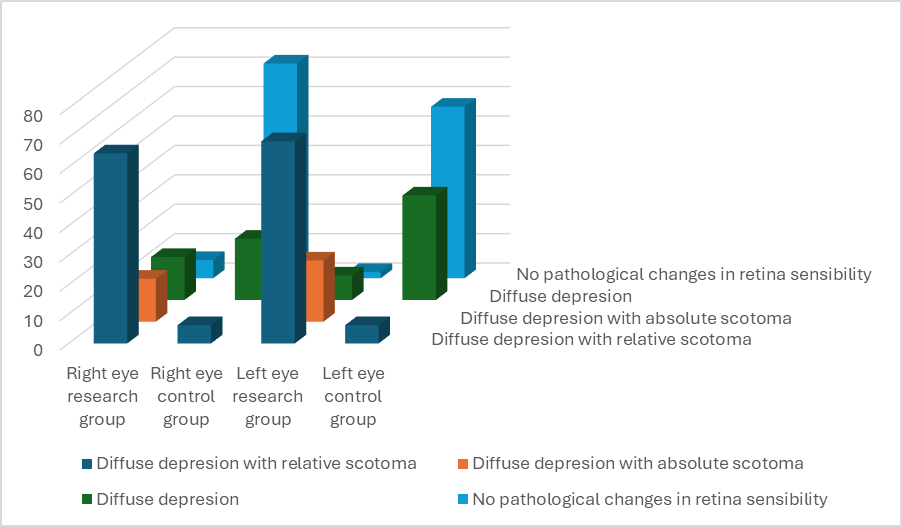
The Bebi curve graphically displays the summary image of the retinal sensitivity of the visual field. The graphic recording of the Bebi curve in the research group revealed the following changes for the right eye: diffuse depression with relative paracentral scotomas in 64.6% (31 patients), diffuse depression with absolute paracentral scotomas in 14.6% (7 patients), diffuse depression in 14.6% (7 patients) and unchanged sensitivity in 62.5% (3 patients). In contrast, data with reference to the control group showed unchanged sensitivity in 72.9% (35 patients), diffuse depression in 20.8% (10 patients), and diffuse depression with relative paracentral scotomas in 6.2% (3 patients). For the left eye, the distribution for the research group was as follows: diffuse depression with relative paracentral scotomas 68.7% (33 patients), diffuse depression with absolute paracentral scotomas in 20.8% (10 patients), and diffuse depression in 8.3% (4 patients) and unchanged sensitivity in 2.1% (1 patient). Data for the control group were indicated unchanged sensitivity in 58.3% (28 patients), diffuse depression in 35.4% (17 patients), and diffuse depression with relative paracentral scotomas in 6.2% (3 patients) (fig.1).
Fig. 1 Bebi curve data after brain injury in children aged between 7-18 years (96 patients). |
Visual field examinations were performed 4 months after the trauma in both groups. A lack of fixation was observed among the patients in the research group (tab. 6), with 73% (35 patients) showing values up to 20% for the right eye. In 25% (12 patients) this index was between 21-60%, and 2.1% of cases (1 patient), the index was between 61-100%. In the control group, values for the right eye were determined in 79.1% (38 patients) up to 20%, in 14.6% (7 patients) within the range of 21-60% and 6.3% (3 patients) in the range of 61-100% (p < 0.001).
For the left eye, the estimated results revealed a lack of fixation among patients in the research group: in 93.7% of cases (45 patients), the loss of fixation was in the range of up to 20%, and in 4.2% of cases – within the range of 21%-60%. This is compared to the distribution of the fixation values for the left eye in the control group: 97.9% cases (47 patients) - range up to 20%, in 2.1% cases (1 patient) – within the range of 21-60% (p < 0.001) (tab. 6).
Table 6. Fixation loss ratio after 4 months of brain injury in children aged between 7-18 years (96 patients). | |||||
Eye | Values | L1 | L0 | ||
Patients | % | Patients | % | ||
Right | Up to 20% | 35 | 73 | 38 | 79.1 |
21%-60% | 12 | 25 | 7 | 14.6 | |
61%-100% | 1 | 2.1 | 3 | 6.3 | |
p < 0.001 | |||||
Left | Up to 20% | 45 | 93.7 | 47 | 97.9 |
21%-60% | 2 | 4.2 | 1 | 2.1 | |
61%-100% | 1 | 2.1 | 0 | 0 | |
p < 0.001 | |||||
Note: L1 – research batch; L0 – control batch; Applied statistical test Fisher’s test. | |||||
The evaluation of the ability to fixate the false positive points revealed equal values in both eyes for the interval up to 20%, with 91.7% in the control group, and 91.7% in the research group (p < 0.001), and for the left eye 93.7% in the control group, versus 93.7% cases in the research group (p < 0.001). Meanwhile, it should be noted that the rate of the ability to fix false positive points in the range of 21-60% for the right eye was revealed in 6.2% patients in the researched group, versus 8.3% in the control group and the range 61-100% - 2.1% patients in the research group (tab.7). For the left eye, the values were as follows: the range of 21-60% - 4.2% patients in the research group, versus 6.3% in the control group and the range 61-100% - 2.1% patients in the research group.
Table 7. False positive points fixation after 4 months of brain injury in children aged between 7-18 years (96 patients). | |||||
Eye | Values | L1 | L0 | ||
Patients | % | Patients | % | ||
Right | Up to 20% | 44 | 91,7 | 44 | 91,7 |
21%-60% | 3 | 6,2 | 4 | 8,3 | |
61%-100% | 1 | 2,1 | 0 | 0 | |
p < 0.001 | |||||
Left | Up to 20% | 45 | 93,7 | 45 | 93,7 |
21%-60% | 2 | 4,2 | 3 | 6,3 | |
61%-100% | 1 | 2,1 | 0 | 0 | |
p < 0.001 | |||||
Note: L1 – research batch; L0 – control batch; Applied statistical test Fisher’s test. | |||||
The evaluation of the ability to on fixate false negative points did not reveal significant statistical differences between the groups. Thus, in both the research group and in the control group, most of patients presented values up to 20%, with 93.7% in the research group and 95.8% in the control group (p < 0.05), and for the left eye: research group – 89.6% and in the control group – 97.9% (p < 0.05) (tab. 8).
Table 8. False negative points fixation after 4 months of brain injury in children aged between 7-18 years (96 patients). | |||||
Eye | Values | L1 | L0 | ||
Patients | % | Patients | % | ||
Right | Up to 20% | 45 | 93,7 | 46 | 95,8 |
21%-60% | 2 | 4,2 | 0 | 0 | |
61%-100% | 1 | 2,1 | 2 | 4,2 | |
p < 0.05 | |||||
Left | Up to 20% | 43 | 89,6 | 47 | 97.9 |
21%-60% | 4 | 8,3 | 1 | 2.1 | |
61%-100% | 1 | 2,1 | 0 | 0 | |
p < 0.05 | |||||
Note: L1 – research batch; L0 – control batch; Applied statistical test Fisher’s test. | |||||
Evaluation of the localized defect indices indicated values between < 0dB, 3dB> in 93.7% (45 patients) - L1 and 97.9% (47 patients) - L0for the right eye. Levels in the < 3dB, 9dB > range were recorded in 4.2% (2 patients) - L1 and 2.1% (1 patient) - L0. The maximum range of >9dB was recorded for 2.1% (1 patient) of the research group. For the left eye, the following values were determined: the range of < 0dB, 3dB > characteristic for 91.6% (44 patients) - L1 and 100% (48 patients) - L0. The interval < 3dB, 9dB> attributed to 6.3% (3 patients) - L1 and maximum values of 9dB> to 2.1% (1 patient) were determined only in the research group. The distribution of the average elevation in the researched group was as follows for the right eye: the reference range was < -6dB, -3dB > in 12.5% (6 patients), the range of -6dB> in 12.5% (6 patients) and < -3dB, 3dB > in 75% (36 patients). Compared to the control group, these indices were primarily in the range < -3dB, 3dB > in 87.5% (42 patients), followed by the range < -6dB, -3dB > in 12.5% (6 patients). For the left eye, the value distribution was very similar to that of the right eye, with the following determined values for the research group: range < -6dB, -3dB> for 27.1% (13 patients), range of -6dB> for 10.4% (5 patients) and < -3dB, 3dB > for 62.5% (30 patients). Compared to the control group: < -3dB, 3dB > range for 91.7% (44 patients), followed by < -6dB, -3dB > range for 8.3% (4 patients)
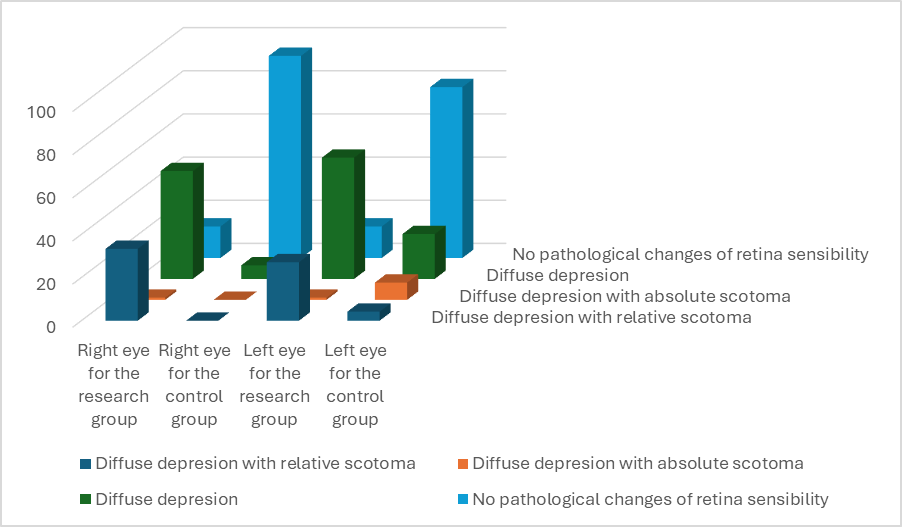
The graphic recording of the Bebi curve in the research group revealed the following changes for the right eye: diffuse depression with relative paracentral scotomas in 33.3% (16 patients), diffuse depression with absolute paracentral scotomas in 2.1% (1 patient), diffuse depression in 50% (24 patients) and unchanged sensitivity in 14.6% (7 patients). In contrast, data for the control group showed predominantly unchanged sensitivity in 93.7% (45 patients), diffuse depression in 6.3% (3 patients). For the left eye, the distribution for the research group was as follows: diffuse depression with relative paracentral scotomas in 27.1% (13 patients), diffuse depression with absolute paracentral scotomas in 2.1% (1 patient), diffuse depression in 56.2% (27 patients) and unchanged sensitivity in 14.6% (7 patients). The data for the control group indicated unchanged sensitivity in 79.2% (28 patients), diffuse depression in 20.8% (10 patients) (fig.2).
|
Fig. 2 Bebi curve data after 4 months of brain injury in children aged between 7-18 years (96 patients). |
Discussion
Reliability criteria of the visual field assessment were categorized according to previously determined percentage ranges. Patients in the research group exhibited a noticeable disturbance in fixation capacity of more than 20%, while in the control group the fixation capacity was maintained up to 20%. The rate of the ability to fixate on false positive points was up to 20% patients for both the research and control group. Similarly, the rate of the ability to fixate false negative points was within the range of up to 20% for both the research and control group. These values outline that visual field evaluation in the acute stage of brain injury can be performed, but its results should not be considered fully reliable, as the credibility criteria are not satisfactory met. Subsequent re-evaluation of these indices revealed significant changes. Later, disturbances in the fixation capacity were predominantly for the interval up to 20% for both the research and control group. The ability to fix false positive points was up to 20% in both groups. The ability to fixate on false negative points was within the range of up to 20% for both groups. Thus, perimetric examination could be a significant test in the initial phase of the post-TCB visual disturbances, but it requires repeated evaluation.
One of the aims of our research was to determine whether there are specific intervals for reliability criteria for TBI patients. The difference we found is that the false positive errors and false negative errors may be considered up to 20%, although some authors suggest that this range could extend up to 33% (Salman Dar, 2014). The parameters characterizing the diffuse loss of retinal sensitivity had a distribution with a suppressive tendency for posttraumatic patients. The index of localized defects was up to 3dB in both groups. The average elevation index was within the range of < -3dB, 3dB> in most of the control group. These numbers indicate an obvious alteration of retinal sensitivity after head trauma without a specific scotoma arrangement. The graphic interpretation of changes in the visual field revealed a prevalence of the incidence of diffuse retinal depression with relative paracentral scotomas in the research group, and for the control group unchanged sensitivity was determined. The index of localized defects was up to 3dB in both groups. The average elevation index was within the range of < -3dB, 3dB> in both groups. The graphic interpretation of changes in the visual field over time revealed a shift towards diffuse retinal depression with relative paracentral scotomas, as well as diffuse depression in the case of the research group, and for the control group an unchanged sensitivity was observed. It should be noted that the index of average elevation and localized defects correlates with reliability criteria (Heijl A,2022).
Visual field defects are identified in case of brain trauma in children. One of the goals of the research was to assess if the evaluation method would be sufficiently reliable, considering the fact that children are generally less cooperative. In cases of mild TBI, it is not appropriate to refer to the presence of well-defined visual field defects in the form of hemianopsia and/or quadranopsia. More commonly, relative scotomas are present, scattered in the field of vision, varying in size and intensity, and influenced by the extent of nerve tissue damage. However, we observe a decrease in retinal sensitivity, a fact clearly demonstrated by the Bebi curve, which shows the alteration of the visual stimulus perception by the retina in the immediate post-traumatic period. These changes, however, are compensated as the recovery period progresses, possibly due to the neurostimulatory treatment to which every post-TBI patient is subjected. Most of the research point that TBI may be associated with hemianopia or quadrantopia in the adult population (Saliman N., 2021). According to our research in pediatric population, retinal sensitivity is affected with relative scotomas dispersed without any particular location.
Conclusion
- Due to the fact that the reliability criteria of visual field assessment, such as fixation loss, false positive and false negative points fixation, do not meet the required credibility values in the acute period of brain injury in school-aged, the determined values should not be taken into consideration. However, they should be recorded and re-evaluated to determine possible organic changes.
- The reference values for reliability criteria in visual field examinations in school-aged children set the intervals for fixation loss, false positive points fixation and false negative points fixation at up to 20%.
- Most the school children undergoing TBI exhibit in the acute period, changes of the retinal sensitivity detected on visual field assessment, with values of structural defects ranged between < 3 dB, 9 dB> and index of average defects >-6 dB.
- Graphical representation of visual field evaluation in school-aged children after TBI does not present delimited visual field defects such as hemianopia and/or quadrantopia, but shows diffuse sensibility alteration in 50% and diffuse sensibility alteration with relative paracentral scotomas in 33.3%.
Competing interests
None declared.
Authors’ contribution
VV conceptualized the project and drafted the first manuscript. EB interpreted the data. EB critically revised the manuscript. All authors revised and approved the final version of the manuscript.
Patient consent
Obtained.
Ethical statement and patient consent
The Research Ethics Committee of Nicolae Testemiţanu State University of Medicine and Pharmacy approved the study, on 21.05.2018 minutes No.63.
Funding
The author have not declared a specific grant for the research from any funding agency in the public, commercial, or not-for-profit sectors.
Provenance and peer review
Not commissioned, externally peer review
Authors’ ORCID IDs
Victoria Verejan – https://orcid.org/0000-0002-0243-2582
Eugeniu Bendelic – https://orcid.org/0000-0001-7127-9457
References
Suchoff IB, Kapoor N, Ciuffreda KJ, Rutner D, Han E, Craig S. The frequency of occurrence, types, and characteristics of visual field defects in acquired brain injury: a retrospective analysis. Optometry. 2008;79(5):259-65. doi: 10.1016/j.optm.2007.10.012.
Verejan V., Bendelic E., Bernic J. Optimizing diagnose for visual disturbances after head trauma in school children. The Moldovan Medical Journal, 2019,62(3), 52-58.
Ciuffreda KJ, Ludlam DP, Yadav NK, Thiagarajan P. Traumatic brain injury: visual consequences, diagnosis, and treatment. Adv Ophthalmol Optom. 2016;1(1):307-333. doi: 10.1016/J.YAOO.2016.03.013
Chan RV, Trobe JD. Spasm of accommodation associated with closed head trauma. J Neuroophthalmol. 2002;22(1):15-7. doi: 10.1097/00041327-200203000-00005.
Ross NC, Bowers AR, Peli E. Peripheral prism glasses: effects of dominance, suppression, and background. Optom Vis Sci. 2012;89(9):1343-52. doi: 10.1097/OPX.0b013e3182678d99.
Plow EB, Obretenova SN, Fregni F, Pascual-Leone A, Merabet LB. Comparison of visual field training for hemianopia with active versus sham transcranial direct cortical stimulation. Neurorehabil Neural Repair. 2012;26(6):616-26. doi: 10.1177/1545968311431963.
Dougherty RF, Koch VM, Brewer AA, et al. Visual field representations and locations of visual areas V1/2/3 in human visual cortex. J Vis. 2003;3(10):586-598. doi: 10.1167/3.10.1.
Lyamzin D, Benucci A. The mouse posterior parietal cortex: anatomy and functions. Neurosci Res. 2019;140:14-22. doi: 10.1016/j.neures.2018.10.008.
Leh SE, Johansen-Berg H, Ptito A. Unconscious vision: new insights into the neuronal correlate of blindsight using diffusion tractography. Brain. 2006;129(Pt 7):1822-1832. doi: 10.1093/brain/awl111.
Whitney D, Levi DM. Visual crowding: a fundamental limit on conscious perception and object recognition. Trends Cogn Sci. 2011 Apr;15(4):160-168. doi: 10.1016/j.tics.2011.02.005.
Ellis CT, Yates TS, Skalaban LJ, et al. Retinotopic organization of visual cortex in human infants. Neuron. 2021;109(16):2616-2626. doi: 10.1016/j.neuron.2021.06.004.
Chiseliţă D. Oftalmologie generală [General ophthalmology]. Iaşi: Dosoftei; 1997. Romanian.
Șcerbatiuc C. Principii de bază ale perimetriei computerizate [Basic principles of computerized perimetry]. Chișinău: Medicina; 2022. 35 p. Romanian.
Salman Dar, Bitrian E., Tokarev J.,Grajewski A. Reliability of Visual Fields in Children. Investigative Ophthalmology & Visual Science April 2014, Vol.55
Heijl A. False Positive Responses in Auitomated Perimetry. Am.J.Ophthalmology. Jan:233:180-188,2022.
Saliman N. H., Belli A., Blanch R. J. Afferent visual manifestations of traumatic brain injury. Journal of neurotrauma 2021. Т. 38. №. 20. Pag. 2778-2789.