Introduction
The deep infiltrative endometriosis (DIE) is acknowledged as the most severe manifestation of pelvic endometriosis, comprising a quarter of its various phenotypes [1-3]. DIE is characterized by fibromuscular infiltration of organs and anatomical structures with subperitoneal invasion of endometrial tissues, regardless of the depth of infiltration, and it presents as a systemic, chronic inflammatory disease cyclically dependent on menstruation, with chronic pelvic pain being its common manifestation [1, 4-6].
The occurrence of DIE is on the rise. Despite ongoing research efforts worldwide, understanding its pathogenesis, clinical features, diagnostic methods, and treatment options remains a focus of intensive investigation. Impacting approximately 2% of females in their reproductive years, DIE contributes to pelvic pain syndrome, extragenital symptoms, fertility problems, and diminished reproductive prognosis for affected individuals [1, 5].
At the global consensus in 2021, the following classifications for clinical use in endometriosis were recommended: rASRM (revised American Society for Reproductive Medicine), the EFI scale (Endometriosis Fertility Index), and the #Enzian classification. These classifications not only allow for staging the pathological process but also for evaluating the reproductive prognosis of the patients [7, 8]. Of particular interest for our study are the #Enzian classification, which completely describes all possible forms of DIE, and the EFI, which provides a precise reproductive prognosis and allows for specific recommendations regarding fertility management for patients in the postoperative period [9-11].
As per the literature, clinical manifestations of DIE encompass the 4 "D" symptoms: dysmenorrhea, dyspareunia, dysuria, and dyschezia, frequently accompanied by infertility [12]. The primary cause of infertility associated with endometriosis (DIE) is the distortion of normal pelvic organ anatomy. Additionally, endometriosis impairs fertility through other mechanisms: inflammation and scarring of surrounding tissues lead to dysfunction of the ovaries and uterus, affecting the quality of oocytes and their ability to be fertilized. High levels of inflammatory cytokines and mediators negatively impact embryo implantation [13].
Scientific literature indicates that DIE, being the most aggressive and clinically prominent phenotype of endometriosis, notably diminishes the QoL for patients [14, 15]. This deterioration arises not only due to severe pain and extragenital symptoms but also because of the infertility. These factors collectively exacerbate the challenges faced by affected women, further diminishing their QoL [3].
After analyzing the scientific literature dedicated to the issue of DIE, it was decided to implement a study, the aim of which was to compare the impact of the DIE and others forms of endometriosis on EFI, patients' fertility and on reproductive prognosis to understand the management approach.
Material and methods
A cohort clinical study was carried out over a span of 2 years at the Gheorghe Paladi Municipal Clinical Hospital in Chisinau. Approval for the study was obtained from the Research Ethics Committee of Nicolae Testemiţanu State University of Medicine and Pharmacy (minutes No. 38, from 21.05.2021). The research involved women of reproductive age diagnosed with "Endometriosis," confirmed through intraoperative findings or indications from ultrasound/MRI scans according to the #Enzian classification from 2019, adhering to predefined inclusion and exclusion criteria. Exclusion criteria encompassed patients below the legal age, those who were virgins, retired individuals, cases of endometriosis with malignancy, severe extragenital pathologies (such as hypertension, cardiovascular, or liver disorders), precancerous or cancerous conditions (including cervical, endometrial, or ovarian), and patients who declined participation in the clinical investigation. Each participant provided informed consent prior to enrollment.
Consequently, the cohort comprised 190 women divided into two distinct groups according to the #Enzian classification: the study group comprised 85 patients diagnosed with DIE (compartments A, B, C, F), while the control group consisted of 105 women diagnosed with endometriosis of the ovaries, tubes, and superficial peritoneal endometriosis (corresponding to compartments O, T, P in the #Enzian classification 2019).
To quantify the impact of endometriosis on patient fertility, the EFI was employed. Pain severity was assessed using the Visual Analog Scale (VAS). Data analysis was conducted using an Excel spreadsheet, and statistical analyses were performed using the SPSS software. The Mann-Whitney U test was employed to compare quantitative variables between groups, while the Pearson's Chi-square test (χ²) was utilized for comparing qualitative variables among groups.
Results
The cohort of women was divided into two groups according to the #Enzian classification. So, in the main group of 85 patients, the lesions were distributed as follows in #Enzian compartments: A - 55.3%; B - 8.2%; C - 1.2%; FA - 17.6%; FB - 17.6%; FI - 9.4%; FO - 12.9%; P - 34.1%; O - 70.6%; T - 51.8%. In the control group of 105 patients, the localization of endometriosis was distributed as follows in compartments by the #Enzian: P - 15.2%; O - 90.5%; T - 50.5%.
Reproductive anamnesis data. An important objective of the study was to determine the frequency of infertility among groups of patients, as well as to calculate the score of the EFI index for patients' reproductive prognosis.
Thus, among patients with DIE, the frequency of infertility was 83.5% (71 patients out of 85). Detailed fertility calculations revealed that primary infertility in main study group is 48.2%±5.7%; 95% CI (36.5 – 59.3%), while 35.3%±5.4% of women were diagnosed with secondary infertility. Additionally, 14.1%±3.8% of women in this group did not suffer from infertility, and 2.4%±1.6% utilized contraceptive methods (withdrawal method, condoms, Figure 1).
Among the patients in the control group, the percentage of infertility was 71.4% (75 women out of 105). Fertility calculation in this group revealed that 37.1%±4.7% of women experienced primary infertility, while 34.3%±4.8% of women reported secondary infertility. However, within this study group, 21.0%±4.0% did not suffer from infertility, and 7.6%±2.7% utilized contraception (withdrawal method, condoms, Figure 1).
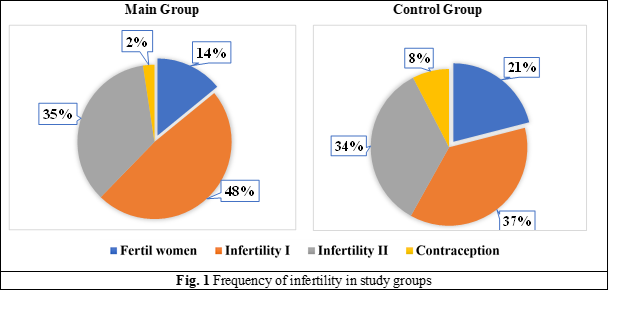
Statistical comparison of the infertility parameter did not reveal a statistically significant difference between the study groups (χ2 = 5.088a, df = 3, p = 0.165).
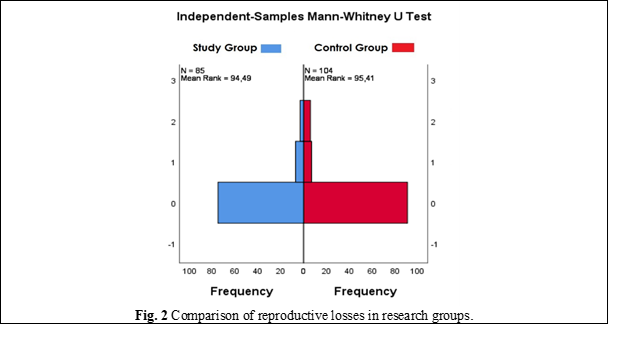
Reproductive losses. In addition, comparison between patients in the study groups did not reveal any differences in terms of reproductive losses (U = 4463.000, p = 0.839). In the main group, the frequency of reproductive losses was 13 cases out of 85 - 15.3%, while in the control group it was 11 out of 105 - 10.5% (Figure 2).
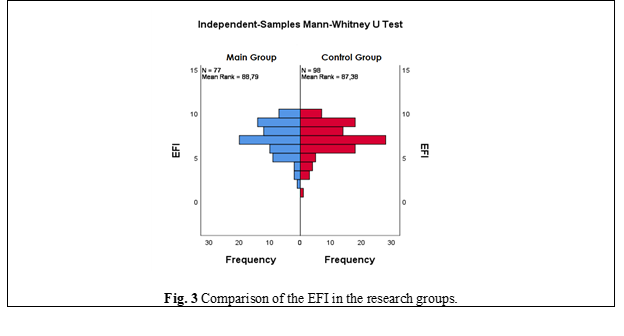
Calculations of EFI. For the final fertility prognosis calculation in the study groups, the EFI index was computed (Figure 3). The median EFI among women with DIE was 7.00 points (mean value - 7.18±0.25 points; 95% CI [6.68 – 7.68 points]). Simultaneously, the median EFI in the control group was also 7.00 points (mean value 7.13±0.29 points; 95% CI [6.55 – 7.71 points]).
Comparison of these data did not reveal a statistically significant difference in this parameter between the study groups (U = 3712.000, p = 0.852), despite the fact that the main group included patients with complete obliteration of the Douglas pouch, whose EFI tends towards 0 points.
Pain levels. The distribution of pain levels on the VAS among women of main group in comparison to the control group of patients is reflected in the Table 1. It is worth noting that patients with DIE are characterized by severe dyspareunia (7.85±0.33 points (95% CI; 7.18 – 8.53 points) vs 2.18±0.46 points (95% CI; 1.23 – 3.13 points) in control group, p < 0.01), which is the cause of sexual abstinence and, accordingly, infertility.
| Table 1. Comparison of pain levels according to the VAS | |||
Pain symptom | Main Group | Control Group | P |
| CPP | 7.90±0.21 | 2.41±0.45 | p < 0.01 |
| Dm | 9.02±0.17 | 5.31±0.52 | p < 0.01 |
| Dp | 7.85±0.33 | 2.18±0.47 | p < 0.01 |
| Du | 1.46±0.47 | 0 | p < 0.01 |
| Dh | 3.83±0.56 | 0 | p < 0.01 |
| Note: VAS - visual analog scale ; CPP - chronic pelvic pain, Dm - dysmenorrhea, Dp - dyspareunia, Dy - dysuria, Dx – dyschezia | |||
Discussion
The study found that although bilateral endometriomas ("kissing ovaries") were included in the DIE group, the total EFI score was greater than 7, similar to the control group. If "kissing ovaries", where EFI approaches 0 and pregnancy can only be achieved with ART, are excluded from DIE, other forms of DIE (88%), where the ovaries are not affected, show higher EFI values than the control group. However, infertility I and II frequencies are similar. This suggests that infertility in women with DIE may not be solely due to the organic changes reflected by EFI but also due to sexual disharmony associated with severe dyspareunia, sexual abstinence, or long-term use of pain-relieving medications, which may delay pregnancy but not always inhibit the progression of endometriosis.
Therefore, using EFI in the DIE group has limitations, potentially delaying ART use and wasting time in achieving spontaneous pregnancy. On the other hand, for women with DIE excluding "kissing ovaries", prolonged periods without pregnancy desire may benefit from multidisciplinary surgical treatment, reducing pain syndrome and dyspareunia, achieving spontaneous pregnancy in the future.
The benefits of surgical treatment for DIE were highlighted in a study by the Endometriosis School in Bordeaux (Horace Roman), showing increased rates of spontaneous pregnancies. Recent studies on the failure of progestin treatment due to the lack of progesterone receptors in DIE lesions, and our data, support surgical treatment in patients not opting for immediate pregnancy, especially in distant compartment DIE forms after #Enzian that do not directly involve the genitals.
Therefore, our study demonstrates the limitations of using EFI scores alone, excluding "kissing ovaries", to evaluate reproductive prognosis in DIE patients. Besides EFI, assessing sexual life quality is crucial to support spontaneous pregnancy in women with DIE. Relying solely on EFI for reproductive prognosis in DIE patients could result in wasted time and unfavorable reproductive outcomes, as it fails to consider dyspareunia and high EFI scores that may delay the timely use of IVF or other ART methods.
Conclusions
Our results suggest that infertility in women with DIE may be more often associated with sexual abstinence due to significant dyspareunia rather than organic impairments. Thus, EFI in patients with DIE does not reflect all aspects of infertility and has reservations, and consideration of both physical symptoms and sexual health is crucial in managing DIE to optimize fertility outcomes. These findings open the way to the feasibility of surgical treatment of DIE to improve sexual quality of life, which will reduce the need for IVF and increase the chances of spontaneous pregnancy in patients, but this conclusion requires further investigation in randomized clinical trials.
Competing interests
None declared.
Authors’ contributions
NC proposed the study's area, conceived the study design, controlled main points of its realization, reviewed the work critically, and approved the final version of the manuscript. EI participated in the study design, contacted and included subjects in research, analyzed and calculated information from questionnaires, performed the statistical analysis of collected data, drafted the manuscript, reviewed the work critically.
Acknowledgements and funding
We express our gratitude to academician Gheorghe Paladi, who advised us to pursue research in the gynecological field and supported the realization of this study. The study had no external funding.
Patient consent
Obtained.
Ethics approval
The study protocol was approved by the Research Ethics Committee of Nicolae Testemiţanu State University of Medicine and Pharmacy (minutes No. 38, from 21.05.2021).
Authors’ ORCID IDs
Nadejda Codreanu – https://orcid.org/0009-0008-8740-0379
Elena Ivanova – https://orcid.org/0000-0001-8460-9849
References
1. Saridogan E, Becker CM, Feki A, Grimbizis GF, Hummelshoj L, Keckstein J, et al. Recommendations for the surgical treatment of endometriosis - part 1: ovarian endometrioma. Gynecol Surg. 2017;14(1):27. doi: 10.1186/s10397-017-1029-x.
2. Imperiale L, Nisolle M, Noël JC, Fastrez M. Three types of endometriosis: pathogenesis, diagnosis and treatment. State of the art. J Clin Med. 2023;12(3):994. doi: 10.3390/jcm12030994.
3. Wild M, Miskry T, Al-Kufaishi A, Rose G, Crofton M. Medical management of deeply infiltrating endometriosis - 7 year experience in a tertiary endometriosis centre in London. Gynecol Surg. 2019;16(1):1-7. https://doi.org/10.1186/s10397-019-1065-9.
4. Bazot M, Daraï E. Diagnosis of deep endometriosis: clinical examination, ultrasonography, magnetic resonance imaging, and other techniques. Fertil Steril. 2017;108(6):886-94. doi: 10.1016/j.fertnstert.2017.10.026.
5. Bazot M, Bharwani N, Huchon C, Kinkel K, Cunha TM, Guerra A, et al. European Society of Urogenital Radiology (ESUR) guidelines: MR imaging of pelvic endometriosis. Eur Radiol. 2017;27(7):2775. doi: 10.1007/s00330-016-4673-z.
6. Becker CM, Bokor A, Heikinheimo O, Horne A, Jansen F, Kiesel L, et al. ESHRE guideline: endometriosis. Hum Reprod Open. 2022;(2):hoac009. doi: 10.1093/hropen/hoac009.
7. Johnson NP, Hummelshoj L, Adamson GD, Keckstein J, Taylor HS, Abrao MS, et al. World Endometriosis Society consensus on the classification of endometriosis. Hum Reprod. 2017;32(2):315-24. doi: 10.1093/humrep/dew293.
8. Vermeulen N, Abrao MS, Einarsson JI, Horne AW, Johnson NP, Lee TTM, et al. Endometriosis classification, staging and reporting systems: a review on the road to a universally accepted endometriosis classification,. Hum Reprod Open. 2021;2021(4):hoab025. doi: 10.1093/hropen/hoab025.
9. Vermeulen N, Abrao MS, Einarsson JI, Horne AW, Johnson NP, Lee TTM, et al. Endometriosis classification, staging and reporting systems: a review on the road to a universally accepted endometriosis classification. J Minim Invasive Gynecol. 2021;28(11):1822-48. doi: 10.1016/j.jmig.2021.07.023.
10. Fruscalzo A, Dayer A, Londero A Pietro, Guani B, Khomsi F, Ayoubi JM, et al. Endometriosis and infertility: prognostic value of #Enzian Classification compared to rASRM and EFI score. J Pers Med. 2022;12(10):1623. doi: 10.3390/jpm12101623.
11. Vitonis AF, Vincent K, Rahmioglu N, Fassbender A, Buck Louis GM, Hummelshoj L, et al. World Endometriosis Research Foundation Endometriosis Phenome and Biobanking Harmonization Project: II. Clinical and covariate phenotype data collection in endometriosis research. Fertil Steril. 2014;102(5):1223-32. doi: 10.1016/j.fertnstert.2014.07.1244.
12. Hernández Cardona MI, Ajewole C, Lewis H, Carrillo JF, Castellanos ME, Barish S, et al. Time to move beyond surgical classification systems for endometriosis. Int J Gynecol Obstet. 2023;163(1):58-62. doi: 10.1002/ijgo.14786.
13. Casals G, Carrera M, Domínguez JA, Abrão MS, Carmona F. Impact of surgery for deep infiltrative endometriosis before in vitro fertilization: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2021;28(7):1303-1312.e5. doi: 10.1016/j.jmig.2021.02.007.
14. Bień A, Rzońca E, Zarajczyk M, Wilkosz K, Wdowiak A, Iwanowicz-Palus G. Quality of life in women with endometriosis: a cross-sectional survey. Qual Life Res. 2020 Oct 1;29(10):2669-77. doi: 10.1007/s11136-020-02515-4.
15. Warzecha D, Szymusik I, Wielgos M, Pietrzak B. The impact of endometriosis on the quality of life and the incidence of depression - a cohort study. Int J Environ Res Public Health. 2020 May 2;17(10):3641. doi: 10.3390/ijerph17103641.