Introduction
With the increase in life expectancy and the improvement of social conditions, natural dentition has to be preserved for a long time to ensure quality of life. However, the prevalence of some dental and jaw diseases remains significant, with dental caries and periodontal disease being the most common. The destruction of periodontal ligaments and the alveolar process that occurs in periodontitis gradually reduces the stability of the tooth in the alveolar socket and increases its mobility [1, 2]. Once tooth mobility appears, the rate of bone tissue destruction accelerates very quickly, leading to even greater tooth mobility and resulting in one of the complications of periodontitis - loss of one or more teeth [3]. The unrestored edentulous space and alveolar ridges may lead to impairment of biomechanics in the dental-facial system, continued deterioration of periodontal tissues, and negative effects on general health. In advanced periodontal disease, teeth loss is often accompanied by severe bone loss, leading to tooth migration, which seriously affects aesthetics and the patient’s social behavior. However, it is known that functionally and aesthetically adequate dentition is important for psychological well-being and quality of life, and prosthodontic rehabilitation is often necessary to restore lost aesthetics and function in periodontally compromised dentition. It is proven that remission of the pathological process in periodontal tissues cannot be achieved without stabilizing mobile, periodontally compromised teeth [4]. The clinical management of mobile teeth is a complex issue that improves the prognosis of teeth and provides stability in periodontal treatment. There are several methods for stabilizing and preserving mobile teeth in periodontitis using various designs of permanent and temporary splinting systems, represented by fixed and movable constructions, each with its own goals, indications, contraindications, advantages, and disadvantages [5-7]. The goal of both removable and non-removable splint-prostheses is to control oral disease while restoring aesthetics and function with durable, biocompatible designs. When choosing the design of a splint-prosthesis, it is important to remember that the preparation of the margin, contour, and profile of protrusion of the prosthesis elements can affect the gum tissue’s response [8-10]. An improperly made denture can damage even healthy oral tissues or aggravate existing periodontal disease [11-13]. Temporary splinting of mobile, periodontally compromised teeth is an important stage in the complex treatment of periodontitis, used to improve mastication, aesthetics, and the prognosis for teeth with pathological mobility. Depending on the purpose of splinting, temporary splints can be used for several days to several months. However, with the development of modern adhesive fixation methods, the duration of temporary splinting can be extended. After the removal of dental deposits, curettage of periodontal pockets, gingivectomy and other therapeutic measures, pathological tooth mobility may increase. Temporary splints help prevent this phenomenon and consolidate the success of conservative and surgical treatments, which also has a positive effect on the patient's psycho-emotional state.
To develop treatment plans with a predictable prognosis for temporary splinting, as well as permanent splinting, it is necessary to consider the proportions of the teeth, the ratio of the weight and length of the elements that make up the splint, the zenith of the gums, and the aesthetics of the periodontium. Bio-functionality and harmony between the temporary splint and periodontal tissues are important for restoring the biomechanics of chewing, aesthetics, and the durability of the remaining teeth and their periodontium. In this regard, its design, occlusion, and biomaterials are of great importance and must be considered in planning.
Visible lengthening of the teeth (which increases the degree of trauma to periodontal tissues) creates some difficulties in choosing the type of temporary splinting system, especially in planning the design of the system and choosing materials to reduce functional overloading of support teeth, which can increase when using fixed splinting system composed of artificial crowns or fixed partial dentures due to their weight. In prosthetic dentistry, temporary splints made from acrylic resin, directly in the patient's mouth, have often been used. However, these splints are unaesthetic, have limited geometric mechanical strength, and poor adhesion to hard tissues of the teeth, which can lead to demineralization of the enamel. That is why temporary splinting using adhesive fibrous splints, for which flexible reinforcing elements and light-curing composite materials are used, has been recognized as one of the most promising methods. This approach allows the creation of aesthetic and fracture-resistant temporary splinting structures. Currently, many manufacturers produce special materials for reinforced splinting of teeth based on an inorganic matrix (ceramics, fiberglass) and materials based on an organic matrix (polyethylene, aramid fibers). The fittings of the elements are made of a variety of the finest fibers with a diameter of 3-5 microns, woven together. Reinforcement fibers gain special strength through their impregnation with resin and flowable composites.
But at the same time, it is necessary to mention that the restorative materials used in such types of splinting can influence biofilm formation because their rough and uneven surfaces create a favorable environment for bacterial colonization. Gingival phenotype, the depth of the gingival sulcus, as well as the location of the alveolar ridge vary from one patient to another and should also be considered in treatment planning. However, contraindications to the procedure are minimal, with increased tooth sensitivity and an allergy to the materials used being among them.
That is why the analysis of the properties of adhesive splints indicates the need for further detailed study of the properties of composite materials used for splinting mobile teeth and the selection of design or structural peculiarities of future constructions. These studies are necessary to develop tactics and criteria for choosing splinting structures for mobile teeth based on the specifics of clinical situations.
The aim of the study is to assess the change in periodontal parameters in patients with periodontal disease before and after the application of temporary splinting with different materials, aimed at restoring periodontal function and occlusal stability.
Material and methods
12 patients (6 female and 6 male), aged 26–60 years, with pathological teeth mobility due to chronic generalized periodontitis were included in the study (Table 1).
Table 1. Features of the lots of patients | |||
Features | Study lot I | Study lot II | Study lot III |
Men | 2 | 2 | 2 |
Women | 2 | 2 | 2 |
Average age | 46 | 48 | 51 |
Number of examined teeth | 22 | 26 | 28 |
All patients were clinically (subjective, objective) and para-clinically examined (OPG, diagnostic models, microbiological examination, parodonto-screen).
Inclusion criteria:
age of the participants 26–60 years old
both males and females
gingival bleeding
gingival recessions
periodontal pockets of varying depth
tooth mobility
partial edentulism of one tooth
no burdened history of general health (according to the patient’s own account, without any complaints)
obtained ethical clearance to include the patient in the study.
The examination of the patient with chronic marginal periodontitis was carried out according to the classic scheme: 1 – anamnesis gathering; 2 - objective clinical examination; 3 - complementary or additional examination. Anamnesis is a valuable component in supporting the data from the objective examination and forming an accurate understanding of the location and nature of the pathological process. The anamnesis included two basic components: the anamnesis of the disease (determining the patient's complaints such as gingival bleeding, changes in color, size, and volume, gum swelling, gingival pain, gingival retraction, tooth mobility, tooth sensitivity, the presence of dental deposits, purulent discharges, and foul odor) and the life anamnesis (providing extensive information about the condition and particularities of the body, living and working conditions, harmful habits, etc.), guiding us toward a correct and comprehensive diagnosis and treatment plan. The objective clinical examination of the patients was recorded in the periodontograms, including clinical-instrumental examination data in graphic form. This allows us to systematize the data from the basic methods used in the examination of the marginal periodontium.
The objective clinical examination was carried out through inspection, palpation, percussion, and auscultation, allowing the confirmation or refutation of the anamnestic data and their objective completion for establishing a preliminary diagnosis. The exo-buccal examination provided information about the facial structure, the condition of the skin, and the presence of changes characteristic of various general ailments or jaw anomalies, occlusion, the condition of the labio-chin and nasolabial areas, chin, lips, facial profile type, latero-mandibular deviations, and the condition of the nervous, lymphatic, salivary, and TMJ systems, among others. The detailed intraoral examination was carried out according to a consistent scheme, determining the condition and depth of the oral vestibule, lip frenulum, the degree of mouth opening, the transition zone of the mucosa, the condition of the teeth and periodontal tissues, interdental contacts, dental migrations, dental arches, and the type of occlusion. During the clinical examination of the gums, attention was focused on their position, color, texture, shape (retractions or inflammations), contour, gingival insertion at the tooth level, the degree of bacterial plaque accumulation, dental tartar, root exposure, the depth of periodontal pockets, etc.
The objective clinical examination of the patients was recorded in the periodontal charts, including clinical-instrumental examination data in graphic form.
The determination of tooth mobility was performed in the usual way, using dental forceps with slight pressure in the vestibulo-oral and axial directions. It was assessed according to the three degrees of mobility based on Miller's classification, modified by P. Fleszar (1980), and recognized in scientific-practical dentistry as:
- grade 1 - tooth movement in the transverse plane does not exceed 1 mm;
- grade 2- in the same plane, tooth movement exceeds 1 mm;
- grade 3- very pronounced mobility, in both transverse and axial directions.
All patients received etiotropic treatment (scaling, root planning, professional brushing). Before completing other treatments (endodontic, surgical, and prosthetic), depending on clinical conditions, temporal splinting using a minimally invasive method with different adhesive fibers for stabilizing mobile teeth was performed. The 12 patients included in our study were divided into three groups: in the I-st group (4 patients), temporary splinting was performed using fiberglass threads braided with polyester microfibers; in the II-nd group (4 patients), temporary splinting was performed using polyethylene fibers; and in the III-rd group (4 patients), temporary splinting was performed using aramid fibers. In all clinical cases, splint fibers were covered with photo-composite material designed for teeth splinting. Restoration of the dental arch integrity (one tooth missing gap) was achieved with an artificial acrylic tooth fixed onto the splint system using the same photo-composite material. Clinical assessment parameters, including the depth of periodontal pockets, the degree of attachment loss, the bleeding index, and the plaque accumulation index, were determined at the beginning of treatment, as well as 1, 3, and 6 months after etiotropic treatment and the installation of splinting devices.
Results and discussions
Periodontitis is one of the most common and serious diseases in dentistry. Timely treatment of periodontitis is necessary to prevent irreversible changes in periodontal tissues, dentition, and overall health. The most effective approach to treating periodontal diseases is considered to be an integrated one, including diagnostics, professional oral hygiene, and a combination of therapeutic, surgical, orthopedic, and orthodontic methods. Splinting mobile teeth occupies a special place in tooth-preserving methods of periodontal treatment and can be used either as a primary therapeutic measure or as an adjunct to stabilize the teeth. A periodontal splint is a device used to maintain and stabilize (immobilize) mobile teeth in their functional and physiological position. Among the various types of splinting, temporary splinting (stabilizing) holds a special and very important role, offering characteristic advantages and indications based on the patient’s overall and dental status.
Assessing the change in periodontal parameters in patients with periodontal disease before and after applying temporary splinting with different materials is possible after a detailed clinical and paraclinical patient examination. The clinical symptoms and their frequency observed in our study groups are described in Table 2.
Table 2. Clinical features of periodontal symptoms in patients groups | |
Periodontal disease symptoms | % out of the number of patients |
| 56% |
| 5% |
| 60% |
| 42% |
| 72% |
| 50% |
| 92% |
| 100% |
| 62% |
| 38% |
Radiological examination results confirmed the presence of signs of periodontitis: atrophy of the alveolar bone to varying degrees, signs of functional overload of the teeth indicated by widening of the periodontal space, and evidence of resorption of alveolar bone tissue, as well as varying degrees of inclination of the remaining teeth. Diagnostic models allowed for the determination of the degree of tooth migration, the presence, location, and extent of furcation invasions, the number and topography of absent teeth, occlusal and interdental relationships, and signs of parafunctional habits.
Temporary splinting of periodontal teeth was performed during conservative treatment, as well as before periodontal surgery and full oral rehabilitation.
For splinting periodontally compromised teeth in the Ist group of patients, fiberglass Cord Armosplint was used. This cord is made of special high-modulus weaving, with fiberglass threads braided with polyester microfibers, having a diameter of 1.5 mm. The cord is silanized (treated) to improve bonding with the composite. It is a moisture-resistant material, well impregnated with a special wetting liquid, which ensures a strong connection between the fiberglass and composite. It can be used with any flowable composite and has similar transparency qualities, which avoids color imitation issues during restoration, especially important for splinting anterior teeth. For convenience, the set with fiberglass “Armosplint” includes a liquid for wetting the fiberglass, a flowable composite, and an adhesive system that provides a strong bond and a reliable marginal fit based on chemical adhesion to tooth tissues. Working with this material, we observed that its flexibility allows good adaptation to uneven tooth surfaces, it can be cut with ordinary sharp scissors and does not unravel. Intra-dental application of the material was done after preparing square-shaped grooves with a depth of 1,5 mm and a width of 1,8-2,0 mm. However, we can mention that the cord thickness plus the covering composite material layer often requires endodontic preparation of the teeth. For fixing an artificial acrylic tooth to restore dental arch integrity, it will be prepared with the same grooves as in the splinted natural teeth.
For splinting periodontally compromised teeth in the IInd group of patients, Construct Kerr was used. This reinforcing tape is made of heavy-duty polyethylene fibers treated with cold gas discharge plasma and impregnated with unfilled resin Construct Resin. After application, the tape does not interfere with brushing and oral hygiene and provides sufficient aesthetics and durability. It can be used in combination with various composite materials. Intra-dental application of the material was performed after preparing square-shaped grooves with a depth of 1,5-2,0 mm and a width of 1,8-2,0 mm, or square-shaped grooves with a depth of 1,5 mm and a width of 1,8-2,0 mm with additional platforms of different shapes (square or dovetail) with the same depth. For fixing an artificial tooth in the reconstruction of dental arch integrity, the same grooves as those in splinted teeth will be prepared
For splinting periodontally compromised teeth in the IIIrd group of patients, aramid fiber Splintkord was used. This material is characterized by its strength, safety, resistance to saliva and food influence, and long service life. When using this material and technique, the teeth are first separated with a thin diamond disk, or the proximal surfaces are cleaned with strips. Wheel-shaped diamond burs are used to create a circular groove of 0.5-0.8 mm depth on the vestibular and oral sides of the tooth, and a deepening with a thin fissure bur to 1.2 mm on the vestibular surface. For fixing artificial acrylic teeth in the restoration of dental arch integrity, the same circular grooves as those in splinted natural teeth will be prepared.
Table 3. Types of applied splinting devices | |
Type of device | Number of dental arches |
Splinting type – palatal | 4 |
Splinting type – lingual | 4 |
Splinting type – circular | 4 |
The temporal splint may be unilateral or bilateral, depending on the number of mobile teeth involved, and requires at least 6 months for monitoring abutment teeth. Temporal splinting in all our three groups of patients necessarily concluded with the control and thorough correction of static and functional occlusal contacts to prevent occlusal trauma. In the cases of frontal edentulism with the absence of one tooth on the lower jaw (6 clinical cases) and on the upper jaw (2 clinical cases), as well as lateral edentulism with the absence of one tooth (first premolar) on the lower jaw (2 clinical cases) and on the upper jaw (2 clinical cases with first premolar absence), the integrity of the dentition was restored using a factory-made artificial acrylic tooth attached to the splint system with fibers used for splinting teeth and closed with the photopolymer composite material Flowrest set. Light-cure composite restorative material Flowrest set with a flowable consistency (low modulus) is used in therapeutic and of orthopedic dentistry for filling cavities of classes III, IV, and V; filling undercuts and making lower layers of classes I and II during restoration; sealing fissures; restoring small defects in indirect porcelain and composite veneers; and splinting movable teeth. It has high thixotropy and medium flowability, allowing it to fill well-prepared grooves in the teeth. We observed that the use of temporary splinting systems in patients included in the study positively affected the condition of periodontal tissue.
One of the essential diagnostic criteria for determining the degree of periodontitis is the depth of periodontal pockets This was assessed in our study across different groups before and after temporal splinting, demonstrating the effectiveness of the treatment method, as shown in Table 4.
Table 4. Average depth of periodontal pockets before and after etiotropic therapy and the application of splinting devices in all three patient groups | |||
| Group I | Group II | Group III |
Pre-treatment (x̄) | 4,7 | 3,9 | 4,2 |
Post-treatment (x̄) | 3.1 | 2,2 | 2,7 |
difference | 1,6 | 1,7 | 1,5 |
Note: Periodontal pockets were measured using a periodontal probe - a blunt-tipped instrument with millimeter markings. The depth of periodontal pockets was measured in millimeters. It was noted that the response to treatment was better in the second group of patients. | |||
The plaque index according to Silness-Löe was significantly reduced in each group compared to the initial values, though the reduction was less significant in the third group (Table 5).
Table 5. Difference in average plaque index before and after etiotropic therapy and the application of splinting devices | |||
| Lot I | Lot II | Lot III |
Pre-treatment (x̄) | 1,56 | 1,9 | 2,2 |
Post-treatment (x̄) | 0.65 | 1,2 | 1,7 |
difference | 0,91 | 0,7 | 0,5 |
Note: The measurement of oral hygiene status using the Silness-Löe plaque index is based on recording both soft debris and mineralized deposits on the teeth. Group I – average difference consisted of 0,91; in group II – 0,7; and in group III – 0,5. | |||
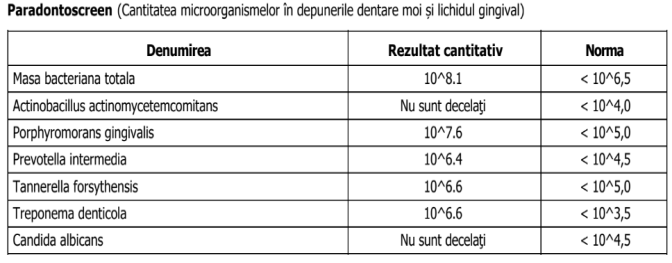
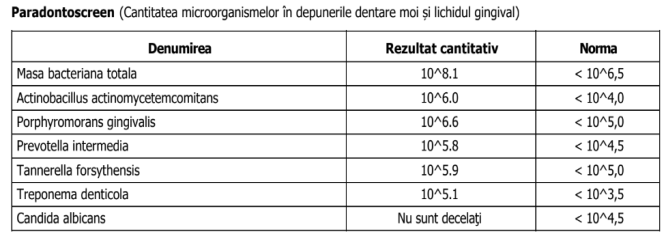
Violations of the qualitative and quantitative balance between normal forms of microflora and opportunistic microorganisms (micro biocenosis of the oral cavity), characteristic of dysbiosis, involve an increase in the number of potentially pathogenic microorganisms and/or an increase in the pathogenic strength of some microorganisms. In our study, such changes were determined through laboratory diagnostic methods in the diagnostic of periodontitis. The microbiocenosis of the oral cavity includes various types of microorganisms (bacteria, viruses, fungi, and protozoa). Qualitative and quantitative balance disruptions between normal microflora forms and opportunistic microorganisms are specific to dysbiosis. In this state, there is an increase in the number of potentially pathogenic microorganisms and/or an enhancement in the pathogenic power of some microorganisms. An effective solution for diagnosing dysbiotic disorders in the oral cavity is ParodontoScreen, a technology for quantitative real-time PCR analysis. Some examples of clinical cases, presented as photos from the investigation results, (that is why they are in Romanian), are shown in Fig.1.
|
|
Fig. 1 Results of Parodontoscreen for some study clinical cases before treatment. | |
ParodontoScreen, for detecting opportunistic microorganisms living in the human oral cavity, enabled us to objectively assess the qualitative and quantitative composition of anaerobic microorganisms in different biotopes of the oral cavity. This optimization of diagnosis and determination of treatment effectiveness is demonstrated in Table 6.
Table 6. Average data of Microbiological and Parodontoscreen results before and after conservative treatment and temporal splinting | ||||||
| Actinobacillus actinomycetemcomitans | Porphyromonas gingivalis | Prevotella intermedia | Tannerella forsythensis | Treponema denticola | Candida albicans |
Pre-treatment | 10^4.1 | 10^7.6 | 10^6.6 | 10^6.8 | 10^6.6 | 10^5.1 |
Post-treatment | - | 10^5.7 | 10^4.7 | 10^5.1 | 10^4.1 | 10^3.1 |
Normal quantity | < 10^4,0 | < 10^5,0 | < 10^4,5 | < 10^5,0 | < 10^3,5 | < 10^4,5 |
Note: Normal data on the quantity of opportunistic microorganisms in the human oral cavity, according to Parodontoscreen exam, were taken from the data of the MedExpert laboratory. | ||||||
In the treatment of patients with periodontal disease, dynamic monitoring is necessary throughout the entire period of temporary splinting. The interval between visits is determined based on the type of splinting, the degree of risk for complications, and factors such as the severity of periodontitis, systemic and local conditions, the level of individual oral hygiene, and the patient's motivation. In cases of gingivitis, mild chronic generalized periodontitis, or mild to moderate periodontal disease, an interval of 6 months between visits is recommended. In cases of moderate to severe chronic generalized periodontitis, or severe periodontitis, the interval is 4 months, while for aggressive forms of periodontitis, it is 2 months.
Conclusions
1. Temporary splinting helps to decrease tooth mobility, allowing for the restoration of periodontal balance, decreased inflammation, and improved tissue healing and attachment gain, contributing to the effectiveness of pathogenetic and symptomatic therapy.
2. An analysis of the properties of adhesive splints indicates the need for further detailed study of composite materials used for tooth splinting. These studies are necessary for developing strategies and criteria for choosing splinting structures based on the specific details of clinical situations.
Competing interests
None declared.
Authors’ contributions
All authors participated in the study design and contributed to drafting the manuscript. The authors critically reviewed the work and approved the final version of the manuscript.
Acknowledgment
We would like to express our special gratitude to University Professor Valeriu Fala, who assisted us in conducting this research.
Patient consent
Obtained.
Ethics approval
No approval was required for this study.
Author’s ORCID IDs:
Mariana Ceban – https://orcid.org/0000-0001-7203-358X
Victor Ceban – https://orcid.org/0009-0000-4039-0478
Vitalie Pântea – https://orcid.org/0000-0002-3489-030X
References
Könönen E, Gursoy M, Gursoy UK. Periodontitis: a multifaceted disease of tooth-supporting tissues. J Clin Med. 2019;8(8):1135. doi: 10.3390/jcm8081135.
Genco RJ, Borgnakke WS. Risk factors for periodontal disease. Periodontol 2000. 2013;62(1):59-94. doi: 10.1111/j.1600-0757.2012.00457.x.
Newman MG, Takei HH, Klokkevold P, Carranza FA, editors. Carranza's clinical periodontology. 12th ed. St. Louis: Elsevier/Saunders; 2015. 875 p.
Durrani F, Galohda A, Rai SK, Singh NK, Verma R, Yadav DS, Karthickraj SM. Evaluation and comparison of stress distribution around periodontally compromised mobile teeth splinted with different materials: three-dimensional finite element analysis. Indian J Dent Res. 2019 Jan-Feb;30 (1):97-101. doi: 10.4103/ijdr.IJDR_250_17.
Al-Sinaidi A, Preethanath RS. The effect of fixed partial dentures on periodontal status of abutment teeth. Saudi J Dent Res. 2014;5(2):104-108. doi: 10.1016/j.ksujds.2013.11.001.
Avetisyan A, Markaryan M, Rokaya D, Tovani-Palone MR, Zafar MS, Khurshid Z, Vardanyan A, Heboyan A. Characteristics of periodontal tissues in prosthetic treatment with fixed dental prostheses. Molecules. 2021;26(5):1331. doi: 10.3390/molecules26051331.
Bluma E, Vidzis A, Zigurs G. The influence of fixed prostheses on periodontal health. Stomatologija. 2016;18(4):112-121.
Hao Y, Huang X, Zhou X, Li M, Ren B, Peng X, Cheng L. Influence of dental prosthesis and restorative materials interface on oral biofilms. Int J Mol Sci. 2018;19(10):3157. doi: 10.3390/ijms19103157.
Heboyan A. Marginal and internal fit of fixed prosthodontic constructions: a literature review. Int J Dent Res Rev. 2019;2(19):21-28. doi: 10.28933/ijdrr-2019-06-1105.
Mangoush E, Säilynoja E, Prinssi R, Lassila L, Vallittu PK, Garoushi S. Comparative evaluation between glass and polyethylene fiber reinforced composites: a review of the current literature. J Clin Exp Dent. 2017 Dec;9(12):e1408. doi: 10.4317/jced.54205.
Nagaraj KR, Savadi RC, Savadi AR, Prashanth Reddy GT, Srilakshmi J, Dayalan M, John J. Gingival biotype – Prosthodontic perspective. J Indian Prosthodont Soc. 2010;10(1):27-30. doi: 10.1007/s13191-010-0011-3.
Knoernschild KL, Campbell SD. Periodontal tissue responses after insertion of artificial crowns and fixed partial dentures. J Prosthet Dent. 2000;84(5):492-498. doi: 10.1067/mpr.2000.110262.
Srimaneepong V, Heboyan A, Zafar MS, Khurshid Z, Marya A, Fernandes GVO, Rokaya D. Fixed prosthetic restorations and periodontal health: a narrative review. J Funct Biomater. 2022 Feb 1;13(1):15. doi: 10.3390/jfb13010015.