Introduction
Lumbar neurocompressive syndrome is a condition characterized by radicular pain, motor, sensory and reflex disorders, paresthesia or numbness in the lower limb, which can be caused by positions and/or movements of the spine [1]. In lumbar radiculopathy, the association of the mechanical and inflammatory factors play an important role. Often large hernias are asymptomatic, indicating that the size of the hernia is not responsible for neurological symptoms and signs [2].
Sensory and motor changes are produced by pure compression of an uninflamed nerve, but without pain. The pain is caused by excitation of an inflamed nerve [3]. It has been established that neurophysiological dysfunctions, degenerative changes, and reduced blood flow in nerve roots are induced by spinal nerve root compression [4]. The forms of pain are different and depend on the degree of compression of the nerve roots and its duration [5]. Pain occurs in the case of cellular damage by producing cellular degeneration, while in moderate ischemia with cellular demyelination pain does not occur [6]. The changes produced by the contact of the nucleus pulposus with the epidural elements have been established in observational studies with the appreciation of convincing evidence of tissue-level changes. After such contact, alterations in nerve electrical activity and intraneural blood flow are observed [7]. During an inflammatory process, nociceptive neurons become sensitized and begin to respond to stimuli that were previously unable to elicit a response. This phenomenon, called hyperalgesia, is common to all inflammatory processes and is characterized by a decrease in the nociceptive threshold and increased activity in response to thermal and mechanical stimulation [8].
Standard radiography in a supine position constitutes the initial stage of the patient's assessment [9]. Lumbar spine radiography cannot determine disc herniation, but indirect signs can be visualized that suggest their presence. These are the so-called classic Barr triad which includes: scoliosis, flattening of the physiological lordosis, and narrowing of the intervertebral space [10, 11]. Spondylosis and subchondral sclerosis of the upper and lower endplates are known as degenerative-dystrophic signs [12]. Lumbar spine radiography in frontal, lateral and oblique incidences is often necessary to exclude other more serious pathologies and to detect degenerative changes in the lumbar spine, for example: osteochondrosis, osteoporosis and changes in the facet joints. Plain radiographic examination is not recommended for patients with low back pain who do not present important or "alarm" signs [13, 14].
Studies by different authors show that the role of MRI in the diagnosis of radiculopathy is limited to visualizing of disc herniation and spinal canal stenosis. In addition, the studies have not provided conclusive information about the accuracy of MRI diagnosis [15]. This is largely explained by the absence of a "gold" standard for the identification of serious vertebral pathology in radiculopathy [16]. MR imaging reflects disc degeneration in the area of low T2 signal intensity, but it is uncertain whether this is a reliable indicator of degenerative structural changes [17]. Disc degeneration and an area of high signal intensity on MRI were not helpful in identifying a symptomatic disc, and when the endplates became abnormal, all discs caused pain consistent with the imaging picture [18].
Imaging signs of degenerative-dystrophic process in the lumbar region of the spine include a decrease in the height of the intervertebral disc, the presence of fissure, edema, vacuum, or calcifications at the level of the intervertebral disc. Changes in the signal at the level of the ligament apparatus and the spinal cord, as well as the presence of marginal osteophytes, disc herniation, listhesis and stenosis, and Modic-type changes in the vertebral bodies can be also determined [19].
Material and methods
The study included 102 patients with signs of lumbar neurocompressive syndrome, of which 51 patients (group I) were examined by MRI and another 51 patients (group II) were examined using standard radiography of the lumbosacral region of the spine. All patients clinically and - neurological examination in the Department of Neurosurgery of the Timofei Moșneaga Republican Clinical Hospital between November 2015 and April 2017. The research protocol obtained a favorable opinion from the Research Ethics Committee (minute no. 74 of 17.06.2016), Nicolae Testemițanu State University of Medicine and Pharmacy, Chișinău, Republic of Moldova.
The reason for the patients to see the doctor was lumbar and leg pain.
Criteria for inclusion in the study:
Adult patients (> 18 years), who signed the informed consent for participation in the study.
Patients with radiculopathy.
People who have no absolute contraindications for standard radiography and/or MRI.
Exclusion criteria:
Patients with acute abdominal syndrome.
Patients with tumors, arterio-venous malformations and spinal infections.
Patients with spinal trauma.
Patients with all forms of intervertebral disc instability.
Patients with systemic diseases, with or without intestinal manifestations (clinically and laboratory confirmed).
People who have absolute contraindications to exploration by radiological methods and MRI.
The following formula was used to determine the required number of patients for the research:
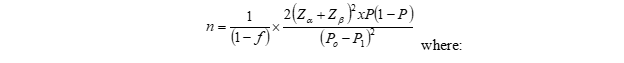
where:
Po = According to the bibliographic data, the success rate of detecting the diagnosis by applying the traditional (radiological) method is on average 40.0% (P0=0.40).
P1 = In the research group, patients will be investigated by the modified method (MRI) with the success rate of detecting 80.0% of cases (P1 = 0.80)
P = (P0 + P1)/2 = 0.60
Zα – tabular value. When the statistical significance is 95.0%, then the coefficient Zα =1.96
Zβ – tabular value. When the statistical power of the comparison is 99.0%, then the coefficient Zβ = 1.96
f = Proportion of subjects expected to drop out of the study for reasons other than the investigated effect q = 1/(1-f), f = 10.0% (0.1).
Entering the data into the formula, we obtained:
Thus, the patients were divided into two groups.
• Group I – patients with lumbar neurocompressive syndrome patients in whom the diagnosis was established by applying the MRI examination of the lumbar region of the spine (n = 51).
• Group II – patients with lumbar neurocompressive syndrome patients in whom the diagnosis was established by applying standard radiographic examination to the lumbar region of the spine (n = 51).
Both MRI and radiological examination of the lumbar spine were performed at the Euromed Diagnostic Medical Center. The clinical examination included: medical history, including evaluating the followings parameters: pain, using visual analogue scale of pain; psychological changes, using assessment scale of psychological changes (HADS scale); social and professional adjustment disorders (ODI scale); patient satisfaction; quality of life (EQ-5D – Euro Quality of Life 5 Dimension). Specific tests and neurological examinations were also performed. Spine radiography was performed in the frontal and lateral views on a Siemens Axiom Luminos dRF machine. Functional radiological investigations were performed at the same facilities. Magnetic resonance imaging was performed on a closed-type Siemens Magnetom Skyra machine with a magnetic field strength of 3 Tesla. The examination was performed with the patient lying on his back. Patient positioning was achieved using a laser to ensure a more homogeneous magnetic field. A localizer-type protocol was used to obtain a 3-plane image positioning and preview. The 3 planes were taken with a step of 4 mm using the sequences T1 and T2 weighted, T2 FS (fat saturation), PD FS. The obtained results were recorded in Excel tables. To compare the sensitivity, specificity, as well as the positive and negative predictive values of the imaging data of the pathologies recorded in the study groups, the 95% confidence interval (95CI) was calculated. Fisher's exact test was used to estimate significant differences in imaging signs between the means of the two groups. The significance threshold was considered p<0.10.
Results
The imaging data obtained in the 2 groups of patients are presented in table 1.
Table 1. Imaging data about the pathologies recorded in the study groups. | |||
| Group I | Group II | p¹ |
Disc herniations | 51 (100%) | 0 (0%) | 0.0000 |
disc extrusions | 43 (84.3%) | 0 (0%) | 0.0000 |
disc protrusions | 39 (76.5%) | 0 (0%) | 0.0000 |
polysegmental damage | 43 (84.3%) | 0 (0%) | 0.0000 |
Marginal osteophytes without signs of root conflict | 51 (100%) | 48 (94.1%) | 0.0813 |
Narrowing of the intervertebral space | 49 (96.1%) | 48 (94.1%) | 0.6409 |
Schmorl's hernias | 48 (94.1%) | 31 (60.8%) | 0.0001 |
Static disorders | 38 (74.5%) | 46 (90.2%) | 0.0401 |
Modic-type edematous changes | 16 (31.4%) | 0 (0%) | 0.0000 |
Vertebral hemangiomas | 14 (27.5%) | 0 (0%) | 0.0001 |
Stenosis of the lumbarspinal canal | 12 (23.5%) | 0 (0%) | 0.0004 |
Disc sequestration | 8 (15.7%) | 0 (0%) | 0.0040 |
Marginal osteophytes with root conflict | 5 (9.8%) | 0 (0%) | 0.0240 |
Disruption of the flowof cerebrospinal fluid | 4 (7.8%) | 0 (0%) | 0.0445 |
Spondylodiscitis | 3 (5.9%) | 0 (0%) | 0.0813 |
Sacroiliitis | 2 (3.9%) | 21 (41.2%) | 0.0000 |
Coxofemoral osteoarthritis | 1 (2.0%) | 14 (27.5%) | 0.0004 |
Subchondral sclerosis | 0 (0%) | 48 (94.1%) | 0.0000 |
Intervertebral discscalcification | 0 (0%) | 3 (5.9%) | 0.0813 |
Note: p¹ applied statistical test – Fisher’s exact | |||
The analysis data of the magnetic resonance imaging investigation of the lumbo-sacral region obtained in the 2 groups of patients are presented in table 2 and 3.
Table 2. Multivariate analysis of magnetic resonance imaging data obtained in patients with sensory disorders (loss of sensation in the lower limb) | ||
The dependent variable | F statistic | p¹ |
Disc sequestration | 12.321 | 0.001 |
Disc extrusions | 6.085 | 0.017 |
Lumbar spinal canal stenosis | 2.895 | 0.095 |
Static disorders of the spine | 1.485 | 0.229 |
Narrowingof the intervertebral space | 1.217 | 0.275 |
Sacroiliitis | 1.217 | 0.275 |
Schmorl'shernias | 1.160 | 0.287 |
Polysegmental disc herniation | 0.642 | 0.427 |
Coxofemoral osteoarthritis | 0.589 | 0.447 |
Modic-typeedematous changes | 0.408 | 0.526 |
Disruptionof the flowof cerebrospinal fluid | 0.269 | 0.606 |
Disc protrusions | 0.126 | 0.724 |
Spondylodiscitis | 0.020 | 0.888 |
Vertebralhemangiomas | 0.019 | 0.891 |
Marginalosteophytes with rootconflict | 0.017 | 0.896 |
Note: p¹ applied statistical test – Fisher’s exact | ||
Table 3. Multivariate analysis of magnetic resonance imaging data obtained in patients with lower limb motor disorders (gait disorders) | ||
The dependent variable | F statistic | p¹ |
Disc extrusions | 8.839 | 0.005 |
Disc sequestration | 7.654 | 0.008 |
Static disorders of the spine | 6.808 | 0.012 |
Disc protrusions | 3.007 | 0.089 |
Narrowingof the intervertebral space | 1.700 | 0.198 |
Coxofemoral osteoarthritis | 0.818 | 0.370 |
Spondylodiscitis | 0.582 | 0.449 |
Schmorl'shernias | 0.172 | 0.680 |
Lumbar spinal canal stenosis | 0.147 | 0.703 |
Polysegmental disc herniation | 0.089 | 0.767 |
Marginalosteophytes with rootconflict | 0.056 | 0.814 |
Disruptionof the flowof cerebrospinal fluid | 0.041 | 0.841 |
Vertebralhemangiomas | 0.038 | 0.847 |
Sacroiliitis | 0.019 | 0.890 |
Modic-typeedematous changes | 0.016 | 0.898 |
Note: p¹ applied statistical test – Fisher’s exact | ||
By analyzing the data of the magnetic resonance imaging investigation of the lumbar spine, a threshold of statistical significance (of 10%, p < 0.10) was determined in patients with sensory disturbances in the lower limb in the case of stenosis of the lumbar spinal canal, and in patients with motor disorders in the lower limb in the case of disc protrusions. In addition, by analyzing the magnetic resonance imaging data, a significance threshold (of 5%, p < 0.05) was determined in patients with sensory disorders (in the case of disc sequestrations and in the case of disc extrusions), and with motor disorders in the case of disc extrusions, disc sequestrations and static disorders of the spine.
The analysis of the results of conventional radiographic investigation of the lumbosacral region obtained in the 2 groups of patients is presented in tables 4 and 5.
Table 4. Multivariate analysis of radiographic data obtained in patients with sensory disturbances (loss of sensation in the lower limb) | ||
The dependent variable | F statistic | p¹ |
Coxofemoral osteoarthritis | 25.039 | 0.000 |
Schmorl'shernias | 4.689 | 0.035 |
Static disorders of the spine | 1.334 | 0.254 |
Marginalosteophytes without rootconflict | 0.759 | 0.388 |
Narrowingof the intervertebral space | 0.759 | 0.388 |
Subchondral sclerosis | 0.759 | 0.388 |
Sacroiliitis | 0.624 | 0.433 |
Intervertebral discs calcification | 0.369 | 0.546 |
Note: p¹ applied statistical test – Fisher’s exact | ||
Table 5. Multivariate analysis of radiographic data obtained in patients with motor disorders in the lower limb (gait disorders) | ||
The dependent variable | F statistic | p¹ |
Intervertebral discs calcification | 20.176 | 0.000 |
Coxofemoral osteoarthritis | 18.356 | 0.000 |
Sacroiliitis | 1.609 | 0.211 |
Schmorl'shernias | 1.306 | 0.259 |
Static disorders of the spine | 1.169 | 0.285 |
Narrowingof the intervertebral space | 0.665 | 0.419 |
Subchondral sclerosis | 0.665 | 0.419 |
Marginalosteophytes without root conflict | 0.524 | 0.473 |
Note: p¹ applied statistical test – Fisher’s exact | ||
The analysis of standard radiography of the lumbar spine allowed the determination of the threshold of statistical significance (of 5%, p < 0.05) in patients with sensory disorders in the lower limb in the case of coxofemoral osteoarthritis and Schmorl’s hernias. In patients with motor disorders at the level of the lower limb, standard radiography of the lumbar spine was informative in case of calcification of the intervertebral discs and in coxofemoral osteoarthritis.
Discussions
IImaging investigations have important clinical significance for the diagnosis and treatment of disc herniation. They can provide not only basic information for diagnosis but also help in making a choice between conservative treatments or surgery and in selecting surgical tactics as well to improve the quality of treatment [20]. Currently, commonly used imaging examinations include MRI, CT, myelography, and radiography. MRI has the advantage of using non-ionizing radiation and offers good visualization capabilities, especially for soft tissues [21]. MRI can also comprehensively observe whether each lumbar intervertebral disc has lesions, identify the degree and location of nucleus pulposus herniation in the sagittal plane, and distinguish whether there are other lesions involving the space in the spinal canal. Lumbar intervertebral disc extrusion is a frequent cause of low back pain that not only manifests as local pain but also is frequently accompanied by radicular pain, sensory deficits, and/or muscle weakness due to nerve root involvement [22, 23]. The results of some studies showed that the sensitivity, specificity, positive likelihood ratio, negative likelihood ratio was 0.89 (95% CI: 0.87-0.91), 0.83 (95% CI: 0.78-0.87), 4.57 (95% CI: 2.95-7.08), 0.14 (95% CI: 0.09-0.22) respectively, for magnetic resonance imaging. Sensitivity, specificity, positive likelihood ratio, negative likelihood ratio was 0.82 (95% CI: 0.79–0.85), 0.78 (95% CI: 0.73–0.82), 3.54 (CI 95%: 2.86–4.39), 0.19 (CI 95%: 0.12–0.30) respectively calculated for tomography. Sensitivity, specificity, positive likelihood ratio, negative likelihood ratio was 0.79 (95% CI: 0.75–0.82), 0.75 (95% CI: 0.70–0.80), 2.94 (CI 95%: 2.43–3.56), 0.29 (CI 95%: 0.21–0.42), respectively for myelography [24]. In our study, significant correlations were observed in MRI images in patients with signs of radiculopathy (manifested by lumbar pain, motor and sensory deficit) or found in the presence of extrusion, sequestration of the intervertebral disc as well as in spinal canal stenosis (significance threshold from 5% to 10%). This corresponds to the literature data. The sensitivity, specificity, positive predictive value, negative predictive value of the method in the case of disc extrusion were 60.78% (CI 95%: 7.02%–33.12%), 100% (CI 95%: 93.02%– 100%), 100% (CI 95%: 93.02%–100%), 55.43% (CI 95%: 52.07%–58.75%), respectively. In case of intervertebral disc sequestration: 9.80% (CI 95%: 3.26%–21.41%), 100% (95% CI: 93.02%–100%), 100% (95% CI: 93.02%–100%), 52.58% (95% CI: 50.32%–54.83%) and in spinal canal stenosis: 5.88% (95% CI: 1.23%–16.24%), 100% (95% CI: 93, 02%–100%), 100% (95% CI: 93.02%–100%), 51.52% (95% CI: 49.80%–53.23%), respectively. In determining the cause of lumbar pain accompanied by motor and sensory deficit due to disc extrusion, MRI sensitivity, specificity, as well as positive and negative predictive values are high. In case of intervertebral disc sequestration as well as the narrowing of the vertebral canal the sensitivity of the method will have low values, but the specificity, the positive and negative predictive values will have high values.
Conventional radiography cannot directly identify the existence of intervertebral disc herniation. Scoliosis, marginal vertebral hyperplasia, and narrowing of the intervertebral space detected radiographically all suggest degenerative changes. If the lumbosacral structure is altered (for example, the presence of transitional vertebrae, spondylolisthesis and spondylolysis), it indicates that the adjacent intervertebral discs present degenerative changes with an increased risk of intervertebral disc prolapse due to increased overloads. With the development of technology today, a radiographic examination is rarely used [25]. In our study, significant correlations following radiological analyses of patients with lumbar radiculopathy are found in case of coxofemoral osteoarthritis, intervertebral disc calcifications and Schmorl’s hernias (significance threshold of 5%). The sensitivity, specificity, positive predictive value and negative predictive value of the method in the presence of coxofemoral osteoarthritis is 3.92% (CI 95%: 0.48%–13.46%), 74.51% (CI 95%: 60.37 %–85.67%), 13.33% (CI 95%: 3.53%–39.30%), 43.68% (CI 95%: 39.55%–47.89%), respectively. In the case of intervertebral disc calcification, they are 0.00% (95% CI: 0.00%–6.98%), 94.12% (95% CI: 83.76%–98.77%), 0% (95% CI: 0 %), 48.48% (95% CI: 46.77%–50.20%) and for Schmorl’s hernias 70.59% (95% CI: 56.17%–82.51%), 39.22% (95% CI: 25.84%–53.89%), 53.73% (95% CI: 46.67%–60.64%), 57.14% (95% CI: 43 .59%–69.70%), respectively. For conventional radiography of the lumbosacral region of the spine, sensitivity, specificity, as well as high positive and negative predictive values are found in the case of Schmorl’s hernias; in the case of intervertebral disc calcifications, the method's sensitivity and positive predictive value are practically zero, with high specificity and negative predictive value. In the case of coxofemoral osteoarthritis, the sensitivity of the method and the positive predictive value of the indices are lower compared to the indices for the specificity of the method and the negative predictive value.
Conclusion
MRI can be considered the imaging technique of first choice in the diagnosis of pathologies of the lumbar spine characterized by sensory and motor changes in the lower limbs.
Competing interests
None declared.
Authors’ contributions
Study design (VS, OM), clinical material acquisition (VS), data interpretation and statistical analysis (VS, OM), manuscript preparation (VS, OM). The final version of the manuscript was read and approved by both authors.
Acknowledgements and funding
The study had no external funding.
Patient consent
Obtained.
Ethics approval
The study protocol was approved by the Research Ethics Committee of Nicolae Testemițanu State University of Medicine and Pharmacy (minutes No. 74, from 17.06.2016).
Authors’ ORCID IDs
Victoria Seu – https://orcid.org/0009-0007-0394-9368
Oxana Malîga – https://orcid.org/0000-0001-9848-5525
References
Ropper AH, Zafonte RD. Sciatica. N Engl J Med. 2015;372(13):1240-1248. doi: 10.1056/NEJMra1410151.
Goupille P, Mulleman D, Valat JP. Radiculopathy associated with disc herniation. Ann Rheum Dis. 2006;65(2):141- 143. doi: 10.1136/ard.2005.039669.
Lurie JD. What diagnostic tests are useful for low back pain? Best Pract Res Clin Rheumatol. 2005;19(4):557-575. doi: 10.1016/j.berh.2005.03.004.
Verhaar JAN, van Mourik JBA. Orthopedie [Orthopedics]. 2nd ed. Houten: Bohn Stafleu van Loghum; 2008. 455 p. Dutch.
van Rijn RM, Wassenaar M, Verhagen AP, et al. Computed tomography for the diagnosis of lumbar spinal pathology in adult patients with low back pain or sciatica: a diagnostic systematic review. Eur Spine J. 2012 Feb;21(2):228-239. doi: 10.1007/s00586-011-2012-2.
Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20(17):1899-1908. doi: 10.1097/00007632-199509000-00011.
International Association for the Study of Pain; Boyd D, Butler M, Carr D, Cohen M, Devor M, Dworkin R, Greenspan J, et al. IASP Pain Terminology. Washington: IASP; 2011 [cited 2023 Oct 12]. Available from: https://www.iasp-pain.org/resources/terminology/#pain.
Hestbaek L, Korsholm L, Leboeuf-Yde C, Kyvik KO. Does socioeconomic status in adolescence predict low back pain in adulthood? A repeated cross-sectional study of 4,771 Danish adolescents. Eur Spine J. 2008;17(12):1727-1734. doi: 10.1007/s00586-008-0796-5.
Powell HC, Myers RR. Pathology of experimental nerve compression. Lab Invest. 1986;55(1):91-100.
Imhof H, Breitenseher M, Kainberger F, Rand T, Trattnig S. Spine disease. European Radiol. 2000;10(Suppl 2):313-319.
Milette PC. Classification, diagnostic imaging, and imaging characterization of a lumbar herniated disc. Radiol Clin North Am 2000; 38: 1267-1292.
Bodiu A. Fiziopatologia durerii radiculare în hernia discală lombară [Pathophysiology of nerve root pain in lumbar disc herniation]. Curierul Medical (Chișinău). 2008;(3):149-152. Romanian.
Adams MA, Roughley PJ. What is intervertebral disc degeneration, and what causes it? Spine. 2006;31(18):2151-2161.
Șavga N. Principii de alegere a tacticii curative a proceselor displazice din segmentul lombosacral [The principes of choice of optimal medical tactics of displastical processes in lumbar-sacral vertebral part]. Arta Medica (Chișinău). 2009;(6):38-41.
Pedachenko IuE, Krasienko EP, Bodiu AP. [Assessment of the results of surgical treatment of lumbar spinal stenosis in different age groups]. Curierul Medical (Chișinău). 2013;56(3):20-28. Russian.
Moraru I, Sangheli M. Spondilodiscita infecțioasă: diagnostic și tratament [Infectious spondylodiscitis: diagnosis and management]. Bull Acad Sci Mold. Med Sci. 2011;1(29):113-117. Romanian.
Sampiev MT, Zagorodnii NV, Dotsenko VV. [Minimally invasive retroperitoneal approach in surgery of degenerative lumbar stenosis]. RUDN J Med (Moscow). 2003;(2):113-116. Russian.
Kushniruk PI, Drevali ON. [Morphological rationale for medial facetectomy during microsurgical removal of herniated lumbar intervertebral discs]. Burdenko J Neurosurg. 2006;(1):13-18. Russian.
Carragee EJ, Tanner CM, Khurana S, et al. The rates of false-positive lumbar discography in select patients without low back symptoms. Spine. 2000;25(11):1373-80. doi: 10.1097/00007632-200006010-00009.
Tsai MD, Jou SB, Hsieh MS. A new method for lumbar herniated inter-vertebral disc diagnosis based on image analysis of transverse sections. Comput Med Imaging Graph. 2002;26(6):369-80. doi: 10.1016/s0895-6111(02)00033-2.
Wassenaar M, van Rijn RM, van Tulder MW, Verhagen AP, van der Windt DA, Koes BW, et al. Magnetic resonance imaging for the diagnosis of lumbar spine pathology in adult patients with low back pain or sciatica: a systematic review of the diagnosis. Eur Spine J. 2012;21(2):220-7. doi: 10.1007/s00586-011-2019-8.
22. Amin RM, Andrade NS, Neuman BJ. Lumbar disc herniation. Curr Rev Musculoskelet Med. 2017;10(4):507-516. doi: 10.1007/s12178-017-9441-4.
Vialle LR, Vialle EN, Suárez Henao JE, Giraldo G. Lumbar disc herniation. Rev Bras Ortop. 2015;45(1):17-22. doi: 10.1016/S2255-4971(15)30211-1.
Huang Z, Zhao P, Zhang C, Wu J, Liu R. Value of imaging examinations in diagnosing lumbar disc herniation: a systematic review and meta-analysis. Front Surg. 2023;9:1020766. doi: 10.3389/fsurg.2022.1020766.
25. Yu X, Niu G, Yang J, Ni L, Zhang W, Guo Y. Quantitative evaluation for the diagnostic efficacy of computed tomography and magnetic resonance imaging in patients with lumbar disc herniation. Natl Med J China. 2011;91(1):23-7. doi: 10.3760/cma.j.issn.0376-2491.2011.01.007.