Introduction
Acoustic neuroma (AN) which is also known as vestibular schwannoma is a benign tumor that originates from the Glial Schwann sheath junction of the VIII pair of cranial nerves and arises more frequently from the inferior vestibular nerve [1]. Although AN is a rare disorder and has an incidence of only 1.09 per 100,000 population, it represents 5-6% of all intracranial tumors and 80% of tumors found in cerebellopontine angle (CPA) [2, 3]. AN is a well-known pathology, with over 10,000 articles published in the Pubmed database and more than 2,000 articles in the last 5 years. The high interest is due to the not very elucidated evolution of AN. According to various articles, AN may remain stable, shrink in size or grow rapidly resulting in a poor outcome [4, 5]. The diagnosis of AN is made by the help of various tests: audiometry, vestibulometry, auditory evoked potentials, vestibular evoked myogenic potentials, but the gold standard in the diagnosis of this tumor is the magnetic resonance imaging (MRI) with gadolinium [6-8]. Nowadays, considering the evolution aspects of AN and the tumor size diagnosed by MRI examination, there are various treatment possibilities such as “Wait and Scan” monitoring, radiological and surgical treatment. The latter remains the gold standard in the treatment of acoustic neuroma and is done through 3 main approaches: retrosigmoid approach (RS), translabyrinthine approach (TL) and middle fosa approach. The surgical treatment of AN started with the first successful removal of this tumor by Thomas Annandale on May 3, 1895. The RS approach was further developed and extensively practiced by Harvey William Cushing who was a pioneer of neurosurgery and is considered the “father of the modern neurosurgery”. He performed his first AN surgery on 12th of January 1906. The TL surgery of AN was developed by William Fouts House, who started to operate this type of tumor through TL approach on 2nd of June 1962. He is also considered to be the “father of neurootology” [9, 10]. In our country, AN surgery was done only through RS approach. A retrospective study on AN, starting from 2010 to 2019 in our country, revealed that 65 patients with histologically confirmed AN were operated in 2 high level neurosurgery departments. According to this study, most of the tumors operated on were large or giant in size, a fact that led to many postoperative complications. The late diagnosis of AN in these cases revealed a series of problems such as: insufficient study of this pathology and inadequate or insufficient use of imaging methods, especially MRI [11].
Case presentation
The 60-year-old patient was hospitalized in the ENT department of Timofei Moșneaga Clinical Republican Hospital “ with the diagnosis of bilateral sensorineural hearing loss for cochlear implantation surgery on the right ear (Fig. 1).
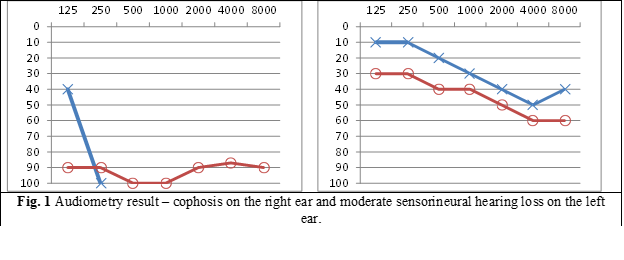
The bilateral hearing loss has been present for more than 10 years, but since 2018 a progressive hearing loss developed in the right ear. Beside the hearing loss, other symptoms were present, such as: permanent high frequency tinnitus on the right ear, which increased with tiredness; periodical vertigo; permanent moderate headache, that was influenced by emotional, physical or atmospheric pressure; unsteadiness and disturbed coordination, especially when walking in the dark. In order to perform the planned surgery (cochlear implantation surgery), patient underwent a brain MRI examination that revealed a 3rd grade CPA tumor on the right side (Fig. 2).
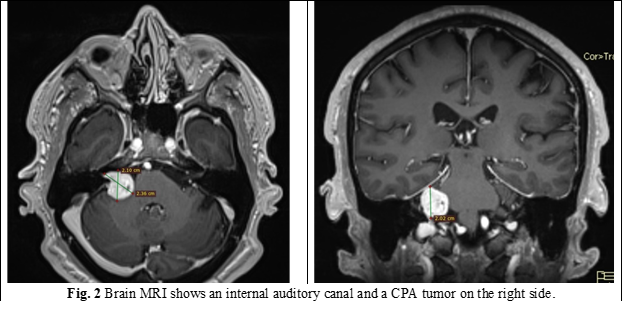
According to the obtained results, the diagnosis of a 3rd grade right AN (by Koos classification) was established.
Afterwards, the patient was consulted by a neurosurgeon and a decision has been taken to switch from cochlear implantation surgery to vestibular schwannoma surgery through a TL approach. The surgery was performed at the Diomid Gherman Institute of Neurology and Neurosurgery by a team of surgeons from the above-mentioned institute, A.I. Kolomiychenko Institute of Otolaryngology from Kiev, Ukraine and colleagues from the Nicolae Testemițanu State University of Medicine and Pharmacy and Timofei Moșneaga Republican Clinical Hospital.
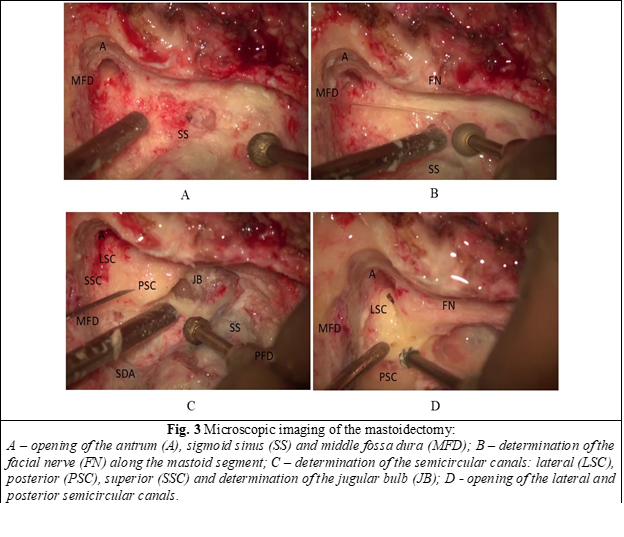
Intraoperatively, a large mastoidectomy was performed, with opening of the middle and posterior fossa dura. The facial nerve was identified along the mastoid segment, the sigmoid sinus was uncovered down to the jugular bulb, and all three semicircular canals were determined. Subsequently, a labyrinthectomy was performed by drilling the lateral, superior and posterior semicircular canals (Fig. 3).
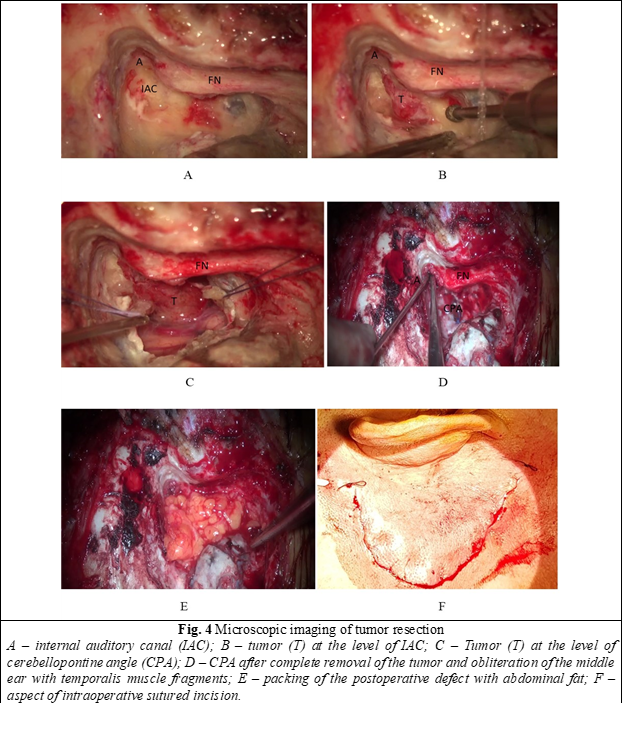
The internal auditory canal (IAC) was visualized and delimited from the lateral, superior, and inferior side. An incision of the dura mater was performed at the level of IAC and CPA and a total resection of the tumor was accomplished. The dura was sutured and the incus was removed. Subsequently, the middle ear has been obliterated with temporalis muscle fragments and the postoperative defect was packed with pieces of abdominal fat (Fig. 4).
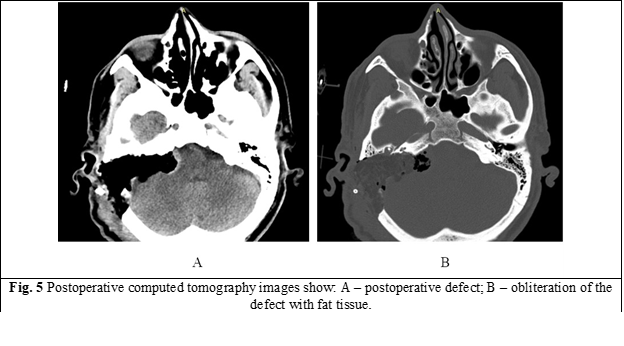
The surgery was performed under the permanent control of the facial nerve function with the help of intraoperative neuro-monitoring. The postoperative patient’s condition was favorable without any signs of facial nerve paralysis. Postoperatively, on the second day, patient underwent a brain computed tomography that showed the volume of the performed intervention which did not reveal any complications (Fig. 5).
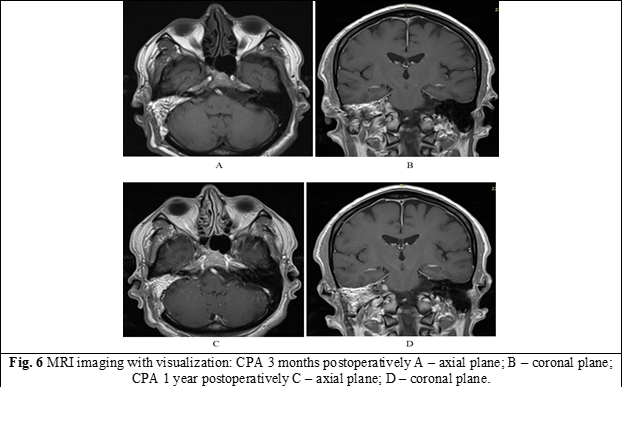
The patient was discharged from medical institution on 20.12.2021 in a satisfactory condition. A brain MRI with contrast was performed 3 months and one year postoperatively, both of them did not reveal any complications or signs of tumor recurrence (Fig. 6).
Discussion
The role of MRI is essential in the diagnosis of AN and it is the gold standard in diagnosing this type of tumor. According to a systematic review made by Fortnum et al., the incidence of AN has increased over the last 30 years due to of the widespread of MRI. This is why Celis-Aguilar et al. concluded that an MRI is strictly necessary in cases of unilateral sensorineural hearing loss [12]. Also, according to the protocol of the European Academy of Otology and Neuro-otology, sensorineural hearing loss of more than 20 decibels in two near frequencies or 15 decibels in frequencies between 2000 – 8000 Hz or unilateral tinnitus serve as recommendations for an MRI examination [13]. The current case revealed an acoustic tumor accidentally found on a MRI examination that was performed during preparation for a cochlear implant, in a patient who mainly complained for bilateral hearing loss and tinnitus for more than 2 years. Nowadays, the most used approaches in AN surgery remain to be the RS and TL approach. The RS approach is mainly used by neurosurgeons, has the advantage of removing CPA tumors of different dimensions, while preserving hearing. The TL approach is performed by a team an otologist and a neurosurgeon, allows for the removal of tumors of any dimension without the need for cerebellar retraction and permits identifying the facial nerve in all its segments. However, because it sacrifices hearing, it is preferably used in patients with profound or total hearing loss [14]. Many studies discuss the comparative results of both approaches and according to Cole et al., the TL approach decreases the risk of facial nerve injury in comparison to RS approach [15]. Also, Pogoda et al., after performing a systematic review about postoperative headache, concluded that it is more frequent in RS approach than in TL approach [16]. Obaid et al. concluded that both approaches have almost similar results in AN surgery, but the TL approach is associated with a less complication rate, making it preferable for patients with profound hearing loss [17]. Despite these findings, Tonn et al. and de Boer et al. stated that both RS and TL approach remain safe and efficient in AN surgery [18-19]. In addition, according to a systematic review performed by Hadjipanayis et al., there is no clear superiority of one approach over the other [20].
In our case, we performed an AN surgery through TL approach because of the cophosis on the affected side and total removal of the tumor was accomplished without any postoperative complications.
Conclusion
The current report, which described an accidental diagnosis of AN, during preparation for a cochlear implantation surgery, resulted in an AN surgery through the TL approach and it serves as an eloquent example of why, in cases of sensorineural hearing loss or tinnitus, it is necessary to perform initially an MRI examination. TL approach in acoustic neuroma surgery allows removal of any size tumors without affecting the brain, especially the cerebellum. In our case, the patient had cophosis on the side of tumor, and it was the most appropriate surgical approach.
Competing interests
None declared.
Authors’ contributions
Concept and design of study, acquisition of data, interpretation of data, revising the manuscript critically for important intellectual content – MB, SV, OB, GZ, VM. All authors have read and approved the final version of the manuscript.
Acknowledgements and funding
A great contribution to the first translabyrinthine surgery of acoustic neuroma in our country had Oleksandr Papp, an Ukrainian otoneurosurgeon from the department of Microsurgery and Otoneurosurgery of A.I. Kolomiychenko Institute of Otolaryngology of the National Academy of Medical Sciences of Ukraine who, being on duty as a surgeon in his homeland, tragically died on 16.05.2022 as a result of Russia’s war in Ukraine. Gone but never forgotten. Rest in peace our dear friend and colleague. The study had no external funding.
Patient consent
Obtained.
Ethics approval
Not needed for this study.
Authors’ ORCID IDs
Marin Buracovschi –https://orcid.org/0000-0001-8939-5886
Oleg Borysenko – https://orcid.org/0000-0003-0125-2990
Grigore Zapuhlîh – https://orcid.org/0009-0008-3654-9974
Sergiu Vetricean – https://orcid.org/0009-0002-3168-9747
Vladimir Moraru – https://orcid.org/0000-0003-4174-1414
References
Roosli C, Linthicum FH Jr, Cureoglu S, Merchant SN. What is the site of origin of cochleovestibular schwannomas? Audiol Neurootol. 2012;17(2):121-5. doi: 10.1159/000331394.
Kshettry VR, Hsieh JK, Ostrom QT, Kruchko C, Barnholtz-Sloan JS. Incidence of vestibular schwannomas in the United States. J Neurooncol. 2015 Sep;124(2):223-8. doi: 10.1007/s11060-015-1827-9.
Zhang S, Liu W, Hui X, You C. Surgical treatment of giant vestibular schwannomas: facial nerve outcome and tumor control. World Neurosurg. 2016 Oct;94:137-144. doi: 10.1016/j.wneu.2016.06.119.
Lees KA, Tombers NM, Link MJ, Driscoll CL, Neff BA, Van Gompel JJ, et al. Natural history of sporadic vestibular schwannoma: a volumetric study of tumor growth. Otolaryngol Head Neck Surg. 2018;159(3):535-542. doi: 10.1177/0194599818770413.
Schnurman Z, Nakamura A, McQuinn MW, Golfinos JG, Roland JT, Kondziolka D. Volumetric growth rates of untreated vestibular schwannomas. J Neurosurg. 2019;2:1-7. doi: 10.3171/2019.5.JNS1923.
House JW, Waluch V, Jackler RK. Magnetic resonance imaging in acoustic neuroma diagnosis. Ann Otol Rhinol Laryngol. 1986;95(1 Pt 1):16-20. doi: 10.1177/000348948609500104.
Hentschel M, Scholte M, Steens S, Kunst H, Rovers M. The diagnostic accuracy of non-imaging screening protocols for vestibular schwannoma in patients with asymmetrical hearing loss and/or unilateral audiovestibular dysfunction: a diagnostic review and meta-analysis. Clin Otolaryngol. 2017 Aug;42(4):815-823. doi: 10.1111/coa.12788.
Singh K, Singh MP, Thukral C, Rao K, Singh K, Singh A. Role of magnetic resonance imaging in evaluation of cerebellopontine angle schwannomas. Indian J Otolaryngol Head Neck Surg. 2015 Mar;67(1):21-7. doi: 10.1007/s12070-014-0736-0.
Pellet W. History of vestibular schwannoma surgery. Prog Neurol Surg. 2008;21:6-23. doi: 10.1159/000156555.
Doyle NM, Doyle JF, Walter EJ. The life and work of Harvey Cushing 1869-1939: a pioneer of neurosurgery. J Intensive Care Soc. 2017 May;18(2):157-158. doi: 10.1177/1751143716673076.
Buracovschi M, Sandul A, Borysenko O, Zapuhlîh G, Moraru V, Glavan I. Studiu retrospectiv al schwanomului vestibular în Republica Moldova [Vestibular schwannoma – a retrospective study in the Republic of Moldova]. ORL.Ro. 2022;15(56/3). doi: 10.26416/ORL.56.3.2022.6922. Romanian.
Celis-Aguilar E, Obeso-Pereda A, Castro-Bórquez KM, Dehesa-Lopez E, Vega-Alarcon A, Coutinho-De Toledo H. Multiple audiometric analysis in the screening of vestibular schwannoma. Cureus. 2022;14(1):e21492. doi: 10.7759/cureus.21492.
Waterval J, Kania R, Somers T. EAONO position statement on vestibular schwannoma: imaging assessment. What are the indications for performing a screening MRI scan for a potential vestibular schwannoma? J Int Adv Otol. 2018;14(1):95-99. doi: 10.5152/iao.2018.5364.
Zanoletti E, Mazzoni A, Martini A, Abbritti RV, Albertini R, Alexandre E, et al. Surgery of the lateral skull base: a 50-year endeavour. Acta Otorhinolaryngol Ital. 2019;39(Suppl. 1):S1-S146. doi: 10.14639/0392-100X-suppl.1-39-2019.
Cole T, Veeravagu A, Zhang M, Azad T, Swinney C, Li GH, et al. Retrosigmoid versus translabyrinthine approach for acoustic neuroma resection: an assessment of complications and payments in a longitudinal administrative database. Cureus. 2015;7(10):e369. doi: 10.7759/cureus.369.
Pogoda L, Nijdam JS, Smeeing DPJ, Voormolen EHJ, Ziylan F, Thomeer HGXM. Postoperative headache after surgical treatment of cerebellopontine angle tumors: a systematic review. Eur Arch Otorhinolaryngol. 2021 Oct;278(10):3643-3651. doi: 10.1007/s00405-021-06627-6.
Obaid S, Nikolaidis I, Alzahrani M, Moumdjian R, Saliba I. Morbidity rate of the retrosigmoid versus translabyrinthine approach for vestibular schwannoma resection. J Audiol Otol. 2018;22(4):236-243. doi:10.7874/jao.2018.00164.
Tonn JC, Schlake HP, Goldbrunner R, Milewski C, Helms J, Roosen K. Acoustic neuroma surgery as an interdisciplinary approach: a neurosurgical series of 508 patients. J Neurol Neurosurg Psychiatry. 2000;69(2):161-166. doi:10.1136/jnnp.69.2.161.
de Boer NP, Koot RW, Jansen JC, et al. Prognostic factors for the outcome of translabyrinthine surgery for vestibular schwannomas. Otol Neurotol. 2021;42(3):475-482. doi: 10.1097/MAO.0000000000002980.
Hadjipanayis CG, Carlson ML, Link MJ, Rayan TA, Parish J, Atkins T, et al. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guidelines on Surgical Resection for the Treatment of Patients with Vestibular Schwannomas. Neurosurgery. 2018 Feb 1;82(2):E40-E43. doi: 10.1093/neuros/nyx512.