Introduction
Globally, the age of motherhood has increased over the previous few decades. According to the report of the Organization for Economic Co-operation and Development, between 1970 and 2021, the average age of women giving birth increased by two to five years in the majority of OECD countries [1]. In numerous high-income countries, the birth rate for women in their late 30s has increased [2].
In 2022, the average age of women at childbirth in Europe varied from 27.8 years in Bulgaria to 32.2 years in Luxembourg, while in Moldova, it was 28 years [3]. Data analysis over the last decade has shown an increase in the birth rate for women aged 35 to 39 in the United States, from 45.9 per 1 000 women in 2010 to 52.7 in 2019. Similarly, there has been an increase in the birth rate for women aged 40 to 44, from 10.2 to 12 per 1 000 [4]. A study conducted in 29 countries across Africa, Asia, the Middle East, and Latin America also revealed that 12.3% of pregnant women fall into the category of advanced maternal age [5]. There is a clear trend of an increasing average age of women at childbirth, partly due to the tendency to delay having their first child [1]. This trend can be explained by women choosing to focus on careers and financial security, thereby postponing maternal age [6]. Furthermore, advances in assisted reproductive technologies have extended the reproductive window, leading to a corresponding increase in the incidence of advanced maternal age [7].
Approximately 21% of total births worldwide, ranging from 6% in low- and middle-income countries to 27% in developed regions, are delivered by cesarean section (CS) [8]. The CS rate continues to rise globally, with reported rates (in 2016) of 24.5% in Western Europe, 32% in North America, and 41% in South America [8, 9]. The reasons for the increasing CS rate are multifactorial, but existing literature suggests that the increase is largely driven by advanced maternal age, especially among nulliparous women [10]. Statistical data indicate higher CS rates among women over 35 years old compared to younger mothers [11]. Additionally, maternal age is considered an independent risk factor for CS or unsatisfactory obstetrical outcomes. Among nulliparous women aged 35 to 39, CS rates are twice as high compared to younger ages and can triple among those over 40 [11, 12]. Consistent research findings have constantly linked increasing maternal age with higher CS rates [13].
Studies have shown that women of advanced maternal age are more likely to have pre-existing chronic diseases (such as chronic hypertension and diabetes) [14], maternal complications (gestational hypertension, gestational diabetes, preeclampsia, placenta previa, and placental abruption) [15], perinatal complications (low birth weight, prematurity, and fetal death) [15], and CS [16]. Additionally, obesity significantly increases the rate of CS, but there is limited evidence in the literature regarding whether elective CS or physiological vaginal delivery (VD) is the optimal mode of delivery for women with morbid obesity [17].
However, unjustified CS can increase short-term and long-term health risks for mothers and their children. Short-term risks include infection, hemorrhage, visceral injuries, placenta accreta, and placental abruption [18]. Long-term risks include asthma and obesity [18]. Additionally, there is a higher likelihood of spontaneous abortion, ectopic pregnancy, and stillbirth in subsequent pregnancies for mothers who have undergone CS [19].
It is important to note that for low-risk women, who typically represent a small proportion of adverse outcomes overall, recovery time after CS is longer compared to VD. Compared to VD, the risk of infection and associated morbidity during a CS can increase by up to 20 times [20]. Therefore, according to the WHO Statement in 2015 regarding CS rates, CS should be performed only when medically necessary [21]. Depending on the location, between 2.5% and 18% of CS performed worldwide are done without medical indications [22, 23].
In low- and middle-income countries, women of advanced reproductive age significantly differ in sociodemographic characteristics [4], which is reflected in parity and mode of delivery. In this context, this study aims to describe the sociodemographic, anthropometric, obstetric, and medical characteristics of women of advanced reproductive age based on the mode of delivery, as well as to evaluate the influence of the interrelationship among these characteristics on the mode of delivery.
The objective of the study is to examine rates of VD and CS among women of advanced reproductive age based on their sociodemographic, anthropometric, medical, and obstetrical characteristics, and to evaluate the relationships among these factors.
Materials and methods
To achieve the stated objective, a selective cross-sectional observational study was conducted with a sample of 528 participants. The inclusion criteria were as follows: women aged between 35 and 49 years who gave birth during advanced reproductive age. As a research tool, a questionnaire developed by the authors was utilized. Interviews were conducted individually using a set of semi-structured questions to gather detailed information about the medical and social characteristics of the participants, in addition to available medical records. Open-ended questions were employed to capture personal experiences and individual perceptions of the participants.
We divided participants into three groups based on the mode of delivery: vaginal delivery, planned cesarean section, emergency cesarean section, and compared the influence of a series of sociodemographic, anthropometric, medical, and obstetrical characteristics using the linear regression method. Additionally, the modification of the effect was analyzed based on a series of variables whose evaluation showed statistically significant variations.
The collected data were analyzed using IBM SPSS Statistics software, version 26.0, following the documentation available at: IBM SPSS Statistics 26 Documentation. Statistical methods appropriate for the type of variables collected were employed. Tests and correlation analyses were utilized to identify potential relationships between medical and social variables. The significance of the results was assessed at a confidence interval of 95%. This methodological approach allowed for a detailed perspective on the socio-medical characteristics of women of advanced reproductive age, contributing to a deeper understanding of this evolving reality.
Results
In the study, 528 pregnant women were included, of whom 77 or 14.6% (95% CI: 12.0% - 18.0%) were aged between 35 and 39 years, and 451 or 85.4% (95% CI: 82.0% - 88.0%) were aged over 40 years. The mean age of the participants was 37.8 ± 2.5 years, with a median of 37.0 (Min=35.0, Max=49.0, IQR=3). The mean age of their partners was 41.7 ± 3.9 years, with a median of 41.0 (Min=34.0, Max=56.0, IQR=7.0) (95% CI: 41.0% – 42.0%).
Primigravidae accounted for 18.9% (95% CI: 16% - 22%), while primipara represented 25.1% (95% CI: 21% - 29%) of the participants. The mean number of pregnancies was 3.2±1.6 pregnancies, with a median of 3.0 (Min=1.0, Max=7.0, IQR=2.0) (95% CI: 3.0 – 3.3%), and the mean number of births was 1.6±1.4 births, with a median of 2.0 (Min=0.0, Max=6.0, IQR=1.3) (95% CI: 1.5% - 1.8%).
The first pregnancy resulted in birth for 66.5% (95% CI: 62% - 71%) of participants, of which 8% (95% CI: 5.6% - 10%) were via Cesarean section (CS). Complicated obstetrical history was reported in 42.0% (95% CI: 38% - 46%) of participants, and pre-existing chronic diseases in 45.3% (95% CI: 41% - 50%) of participants.
VD occurred in 59.5% (95% CI: 55% - 64%) of participants, planned cesarean section (PCS) in 15.9% (95% CI: 13% - 19%), and emergency cesarean section (ECS) in 24.6% (95% CI: 21% - 28%) of participants. Pregnancy complications were recorded in 70.8% (95% CI: 67% - 75%) of participants, and 50.6% (95% CI: 46% - 55%) developed birth complications.
For the identification and evaluation of sociodemographic, anthropometric, obstetrical, and other health-related factors associated with the mode of delivery, a bivariate analysis was conducted.
Table 1 shows the variations in the rates of VD and CS according to the sociodemographic and anthropometric characteristics of women. The mode of delivery differs significantly depending on the mother's age (p=0.013), with a mean of 38.5±2.8 years, a median of 38.0 (Min=35.0, Max=44.0, IQR=4.0) for PCS, and 37.6±2.4 years, a median of 37.0 (Min=35.0, Max=46.0, IQR=3.0) for ECS, and 37.6±2.5 years, a median of 37.0 (Min=35.0, Max=49.0, IQR=3.0) for VD. Similar differences (p=0.001) are also recorded depending on the age of the father, with a mean of 43.0±3.7 years, a median of 43.0 (Min=35.0, Max=53.0, IQR=4.5) for PCS, and 41.5±3.8 years, a median of 41.0 (Min=35.0, Max=53.0, IQR=7.0) for ECS, compared with the mean of 41.4 ±3.9 years, and the median of 41.0 (Min=34.0, Max=56.0, IQR=6.0) for VD.
Statistically significant variations are also established in the evaluation of the relationship between mode of delivery, specifically PCS and ECS, and the following characteristics: area of residence (p=0.003), education (p=0.001), and nature of work (p=0.028). Additionally, comparative evaluation between mode of delivery and workplace exposure (p=0.6), pre-pregnancy BMI (p>0.9), and recommended weight gain during pregnancy (p=0.6) did not reveal statistically significant differences. (Table 1).
Table 1. Relationship between mode of delivery and sociodemographic and anthropometric characteristics | ||||||||
Mode of delivery | VD, N = 3141 | 95% CI2 | PCS, N = 841 | 95% CI2 | ECS, N = 1301 | 95% CI2 | Statistic Test | p-value3 |
Woman`s age | 37.6 (2.5) | 37, 38 | 38.5 (2.8) | 38, 39 | 37.6 (2.4) | 37, 38 | 8,7 | 0.013 |
Partner`s age | 41.4 (3.9) | 41, 42 | 43.0 (3.7) | 42, 44 | 41.5 (3.8) | 41, 42 | 13 | 0.001 |
Area of residence | 12 | 0.003 | ||||||
rural | 150 (47.8%) | 42%, 53% | 35 (41.7%) | 31%, 52% | 39 (30.0%) | 22%, 38% | ||
urban | 164 (52.2%) | 47%, 58% | 49 (58.3%) | 48%, 69% | 91 (70.0%) | 62%, 78% | ||
Education | 18 | 0.001 | ||||||
secondary | 154 (49.0%) | 44%, 55% | 24 (28.6%) | 19%, 38% | 43 (33.1%) | 25%, 41% | ||
vocational | 64 (20.4%) | 16%, 25% | 24 (28.6%) | 19%, 38% | 30 (23.1%) | 16%, 30% | ||
higher | 96 (30.6%) | 25%, 36% | 36 (42.9%) | 32%, 53% | 57 (43.8%) | 35%, 52% | ||
Nature of work | 14 | 0.028 | ||||||
physical | 48 (15,3%) | 11%, 19% | 9 (10.7%) | 4.1%, 17% | 7 (5.4%) | 1.5%, 9.3% | ||
intellectual | 104 (33,1%) | 28%, 38% | 39 (46.4%) | 36%, 57% | 59 (45.4%) | 37%, 54% | ||
mixed | 20 (6,4%) | 3.7%, 9.1% | 5 (6.0%) | 0.89%, 11% | 7 (5.4%) | 1.5%, 9.3% | ||
doesn`t work | 142 (45,2%) | 40%, 51% | 31 (36.9%) | 27%, 47% | 57 (43.8%) | 35%, 52% | ||
Exposure | 2.8 | 0.6 | ||||||
yes | 34 (10.8%) | 7.4%, 14% | 11 (13.1%) | 5.9%, 20% | 11 (8.5%) | 3.7%, 13% | ||
no | 138 (43.9%) | 38%, 49% | 42 (50.0%) | 39%, 61% | 62 (47.7%) | 39%, 56% | ||
Pre-pregnancy BMI | 25.8 (4.3) | 25, 26 | 25.9 (4.3) | 25, 27 | 25.7 (3.8) | 25, 26 | 0.06 | >0.9 |
Weight gain | 12.5 (4.8) | 12, 13 | 12.8 (4.2) | 12, 14 | 12.8 (4.6) | 12, 14 | 0.95 | 0.6 |
Note: 1n (%); Mean (SD); Median (IQR); Minimum Maximum; 2CI = Confidence Interval; 3Pearson's Chi-squared test; Kruskal-Wallis rank sum test | ||||||||
The impact of antenatal care on the mode of delivery was evaluated and presented in Table 2. The study results found that participants who attended antenatal care with a GP had VD in 61.8% (95% CI: 57% - 66%), compared to 44.4% (95% CI: 33% - 56%) among participants who did not attend antenatal care with a GP. Meanwhile, 22.2% (95% CI: 13% - 32%) of participants who did not attend antenatal care with a GP gave birth by PCS, and 33.3% (95% CI: 22% - 44%) by ECS, compared to 14.9% (95% CI: 12% - 18%) of participants who attended antenatal care with a GP and gave birth by PCS, and 23.2% (95% CI: 19% - 27%) by ECS.
The evaluation of the relationship between the average attendance of the GP and the mode of delivery reveals statistically significant deviations (p <0.001). Among participants who had a VD, 40.1% (95% CI: 32% - 49%) had 1-3 GP`s attendances, and 46.5% (95% CI: 41% - 52%) had 4-7 attendances. In comparison, among participants with PCS, 29.8% (95% CI: 11.5% - 48.1%) had 1-3 attendances, and 47.6% (95% CI: 37% - 58%) had 4-7 attendances. For those with ECS, 23.1% (95% CI: 7.7% - 38.4%) had 1-3 attendances, and 55.4% (95% CI: 47% - 64%) had 4-7 attendances.
There is a similar trend observed in the relationship between the average attendances of the obstetrician and the mode of delivery, with statistical deviations yielding p=0.032. The rate of participants with more than 3 attendances of the obstetrician is 70,2% (95% CI: 60% - 80%) for those with PCS and 63.1% (95% CI: 55% - 71%) for those with ECS, compared to participants with up to 3 attendances, representing 29.8% (95% CI: 20% - 40%) for PCS and 36.9% (95% CI: 29% - 45%) for ECS. Simultaneously, the rate of participants with VD is approximately identical for both attendance groups, constituting 55.4% (95% CI: 50% - 61%) for those with > 3 attendances and 44.6% (95% CI: 39% - 50%) for those with 1-3 attendances.
The role of informed decision-making regarding pregnancy and childbirth in women of advanced reproductive age is underscored by statistically significant differences in CS rates based on the timing and content of information about age-related reproductive risks (p=0.005). It is noteworthy that participants who had VD were informed at similar rates either before becoming pregnant or during pregnancy, at 38.9% (95% CI: 33% - 44%) and 38.5% (95% CI: 33% - 44%), respectively. In contrast, for participants who underwent PCS or ECS, the rate of those informed before pregnancy was approximately twice as high compared to those informed during pregnancy, accounting for 59.5% (95% CI: 49% - 70%) and 28.6% (95% CI: 19% - 38%) for PCS, while it was 50.8% (95% CI: 42% - 59%) and 33.8% (95% CI: 26% - 42%) for ECS.
It is noteworthy that in this study, no statistically significant differences were identified for the relationship between the availability and utility of the perinatal book and the mode of delivery in women of advanced reproductive age (p=0.5).
Table 2. Relationship between mode of delivery and antenatal care | ||||||||
VD, N = 3141 | 95% CI2 | PCS, N = 841 | 95% CI2 | ECS, N = 1301 | 95% CI2 | Statistic test | p-value3 | |
GP attendance | 7.8 | 0.020 | ||||||
yes | 282 (89.8%) | 86%, 93% | 68 (81.0%) | 73%, 89% | 106 (81.5%) | 75%, 88% | ||
32 (10.2%) | 6.8%, 14% | 16 (19.0%) | 11%, 27% | 24 (18.5%) | 12%, 25% | |||
Timing of initiation of antenatal care | 1.4 | 0.5 | ||||||
first trimester | 226 (72.0%) | 67%, 77% | 55 (65.5%) | 55%, 76% | 90 (69,2%) | 61%, 77% | ||
second/third trimester | 88 (28.0%) | 23%, 33% | 29 (34.5%) | 24%, 45% | 40 (30.8%) | 23%, 39% | ||
GP attendances | 34 | <0.001 | ||||||
1-3 | 126 (40.1%) | 32%, 49% | 25 (29.8%) | 11,5%, 48,1% | 30 (23.1%) | |||
4-7 | 146 (46.5%) | 41%, 52% | 40 (47.6%) | 37%, 58% | 72 (55.4%) | 47%, 64% | ||
>7 | 10 (3.2%) | 1.2%, 5.1% | 3 (3.6%) | -0.40%, 7.5% | 3 (2.3%) | -0.27%, 4.9% | ||
0 | 32 (10.2%) | 6.8%, 14% | 16 (19.0%) | 11%, 27% | 24 (18.5%) | 12%, 25% | ||
Number of USG exams | 5.6 | 0.2 | ||||||
<=2 | 56 (17.8%) | 14%, 22% | 8 (9.5%) | 3.2%, 16% | 16 (12.3%) | 6.7%, 18% | ||
>2 | 255 (81.2%) | 77%, 86% | 76 (90.5%) | 84%, 97% | 113 (86.9%) | 81%, 93% | ||
0 | 3 (1.0%) | -0.12%, 2.0% | 0 (0.0%) | 0.0%, 0.0% | 1 (0.8%) | -0.73%, 2.3% | ||
Obstetrician attendances | 6.9 | 0.032 | ||||||
1-3 | 140 (44.6%) | 39%, 50% | 25 (29.8%) | 20%, 40% | 48 (36.9%) | 29%, 45% | ||
> 3 | 174 (55.4%) | 50%, 61% | 59 (70.2%) | 60%, 80% | 82 (63.1%) | 55%, 71% | ||
Risk factors information | 15 | 0.005 | ||||||
before pregnancy | 122 (38.9%) | 33%, 44% | 50 (59.5%) | 49%, 70% | 66 (50.8%) | 42%, 59% | ||
after pregnancy
| 121 (38.5%) | 33%, 44% | 24 (28.6%) | 19%, 38% | 44 (33.8%) | 26%, 42% | ||
uninformed | 71 (22.6%) | 18%, 27% | 10 (11.9%) | 5.0%, 19% | 20 (15.4%) | 9.2%, 22% | ||
Pregnancy book | 3.6 | 0.5 | ||||||
Useful | 262 (83.4%) | 79%, 88% | 71 (84.5%) | 77%, 92% | 104 (80.0%) | 73%, 87% | ||
Useless | 31 (9.9%) | 6.6%, 13% | 10 (11.9%) | 5.0%, 19% | 13 (10.0%) | 4.8%, 15% | ||
Not available | 21 (6.7%) | 3.9%, 9.5% | 3 (3.6%) | -0.40%, 7.5% | 13 (10.0%) | 4.8%, 15% | ||
Note: 1n (%); 2CI - Confidence Interval; 3Pearson's Chi-squared test; Kruskal-Wallis rank sum test; GP – General practitioner. | ||||||||
The results of the evaluation of the mode of delivery based on obstetrical characteristics are presented in Table 3. Of the studied group, 59.5% (95% CI: 55% - 64%) of the participants gave birth vaginally, 15.9% (95% CI: 13% - 19%) by PCS, and 24.6% (95% CI: 21% - 28%) by ECS. It is relevant that the evaluation of the mode of delivery based on parity shows statistically significant differences (p<0.001), where, for primiparous, C-section was predominant at 57.9%, including 31.6% ECS, compared to multipara women, where VD was predominant, constituting 65.3%. In the same context, it was found that births among primiparous constituted 17.8% (95% CI: 14% - 22%) of VD, 41.7% (95% CI: 31% - 52%) of PCS, and 32.3% (95% CI: 24% - 40%) of ECS compared to 82.2% (95% CI: 78% - 86%) of VD, 58.3% (95% CI: 48% - 69%) of PCS, and 67.7% (95% CI: 60% - 76%) of ECS in multipara women, representing statistically significant differences (p=0.001).
In the conducted study, the mean number of previous births among participants who delivered via PCS was 1.2±1.3 births, with a median of 1.0 (Min=0.0, Max=5.0, IQR=2.0), 1.3±1.2 births, median 1.0 (Min=0.0, Max=5.0, IQR=2.0) for those with ECS, and 1.9±1.4 births, median 2.0 (Min=0.0, Max=6.0, IQR=2.0) for those who had VD. These differences are statistically significant (p<0.001). The same trend is observed when comparing the number of pregnancies in medical history (p<0.001). Correlation with other variables such as pre-existing chronic diseases (p=0.2), complicated obstetrical history (p=0.13), history of medical abortion (p=0.9), history of spontaneous abortion (p=0.7), and mode of conception (p=0.4) did not reveal statistically significant differences.
Meanwhile, the proportion of primigravidae who delivered via PCS and ECS is approximately twice as high compared to those who had VD, comprising 29.8% (95% CI: 20% - 40%) and 23.1% (95% CI: 16% - 30%) respectively, compared to 14.3% (95% CI: 10% - 18%). Additionally, the rate of multigravidas who delivered vaginally is about 6 times higher compared to primigravidae, 3.3 times higher for those via ECS, and 2.3 times higher via PCS, constituting 85.7% (95% CI: 82% - 90%) for VD, 70.2% (95% CI: 60% - 80%) for PCS, and 76.9% (95% CI: 70% - 84%) for ECS. These differences reach statistical significance with p=0.002.
According to the results of the present study, among participants who had ECS, 81.5% (95% CI: 75% - 88%) had pregnancy complications, and among those who had PCS, 73.8% (95% CI: 64% - 83%) had pregnancy complications, compared to 65.6% (95% CI: 60% - 71%) among participants with VD (p=0.003).
Of particular interest is the finding that the proportion of women who experienced birth complications is significantly lower among participants who had PCS compared to those who had VD or ECS, comprising 25% (95% CI: 16% - 34%) of OCS, compared to 53.8% (95% CI: 48% - 59%) and 59.2% (95% CI: 51% - 68%) of participants who had VD or ECS, respectively, showing statistically significant differences (p < 0.001).
Table 3. Relationship between the mode of delivery and medical and obstetrical characteristics | ||||||||
VD, N = 3141 | 95% CI2 | PCS, N = 841 | 95% CI2 | ECS, N = 1301 | 95% CI2 | Statistic Test | p-value3 | |
Preexisting chronic conditions | 3.1 | 0.2 | ||||||
yes | 133 (42.4%) | 37%, 48% | 44 (52.4%) | 42%, 63% | 62 (47.7%) | 39%, 56% | ||
no | 181 (57.6%) | 52%, 63% | 40 (47.6%) | 37%, 58% | 68 (52.3%) | 44%, 61% | ||
Gravidity | 3.4 (1.6) | 3.3, 3.6 | 2.8 (1.6) | 2.4, 3.1 | 2.9 (1.5) | 2.6, 3.1 | 20 | <0.001 |
Parity | 1.9 (1.4) | 1.8, 2.1 | 1.2 (1.3) | 0.89, 1.5 | 1.3 (1.2) | 1.1, 1.5 | 31 | <0.001 |
Abortion history | 0.4 (0.8) | 0.27, 0.43 | 0.3 (0.7) | 0.15, 0.45 | 0.3 (0.7) | 0.19, 0.42 | 0.23 | 0.9 |
Spontaneous abortion history | 0.2 (0.6) | 0.17, 0.30 | 0.3 (0.7) | 0.15, 0.47 | 0.3 (0.7) | 0.18, 0.43 | 0.78 | 0.7 |
Ectopic pregnancy history | 0.0 (0.1) | 0.00, 0.03 | 0.1 (0.3) | 0.01, 0.14 | 0.0 (0.2) | 0.00, 0.09 | 6.6 | 0.037 |
Parity | 25 | <0.001 | ||||||
primipara | 56 (17.8%) | 14%, 22% | 35 (41.7%) | 31%, 52% | 42 (32.3%) | 24%, 40% | ||
multipara | 258 (82.2%) | 78%, 86% | 49 (58.3%) | 48%, 69% | 88 (67.7%) | 60%, 76% | ||
Mode de conception | 1.7 | 0.4 | ||||||
Natural | 306 (97.5%) | 96%, 99% | 80 (95.2%) | 91%, 100% | 124 (95.4%) | 92%, 99% | ||
IVF | 8 (2.5%) | 0.80%, 4.3% | 4 (4.8%) | 0.21%, 9.3% | 6 (4.6%) | 1.0%, 8.2% | ||
Complicated obstetric history | 4.1 | 0.13 | ||||||
yes | 121 (38.5%) | 33%, 44% | 41 (48.8%) | 38%, 59% | 60 (46.2%) | 38%, 55% | ||
no | 193 (61.5%) | 56%, 67% | 43 (51.2%) | 41%, 62% | 70 (53.8%) | 45%, 62% | ||
Mode of first pregnancy delivery | 75 | <0.001 | ||||||
VD | 227 (72.3%) | 67%, 77% | 26 (31.0%) | 21%, 41% | 56 (43.1%) | 35%, 52% | ||
CS | 7 (2.2%) | 0.60%, 3.9% | 15 (17.9%) | 9.7%, 26% | 20 (15.4%) | 9.2%, 22% | ||
Nulliparae | 80 (25.5%) | 21%, 30% | 43 (51.2%) | 41%, 62% | 54 (41.5%) | 33%, 50% | ||
Pregnancy complications | 12 | 0.003 | ||||||
yes | 206 (65.6%) | 60%, 71% | 62 (73.8%) | 64%, 83% | 106 (81.5%) | 75%, 88% | ||
no | 108 (34.4%) | 29%, 40% | 22 (26.2%) | 17%, 36% | 24 (18.5%) | 12%, 25% | ||
Delivery complications | 27 | <0.001 | ||||||
yes | 169 (53.8%) | 48%, 59% | 21 (25.0%) | 16%, 34% | 77 (59.2%) | 51%, 68% | ||
no | 145 (46.2%) | 41%, 52% | 63 (75.0%) | 66%, 84% | 53 (40.8%) | 32%, 49% | ||
Gestational age | 12 | 0.017 | ||||||
22-28 weeks | 14 (4.5%) | 2.2%, 6.7% | 0 (0.0%) | 0.00%, 0.00% | 2 (1.5%) | -0.58%, 3.7% | ||
29-35 weeks | 31 (9.9%) | 6.6%, 13% | 5 (6.0%) | 0.89%, 11% | 21 (16.2%) | 9.8%, 22% | ||
36-40 weeks | 269 (85.7%) | 82%, 90% | 79 (94.0%) | 89%, 99% | 107 (82.3%) | 76%, 89% | ||
Apgar score at 1 min | 7.0 (1.1) | 6.9, 7.2 | 7.6 (0.9) | 7.4, 7.8 | 7.2 (1.1) | 7.0, 7.4 | 19 | <0.001 |
Apgar score at 5 min | 7.8 (1.0) | 7.7, 7.9 | 8.3 (0.8) | 8.1, 8.5 | 7.9 (1.0) | 7.7, 8.1 | 19 | <0.001 |
Multiple pregnancy | 8.3 | 0.016 | ||||||
yes | 3 (1.0%) | -0.12%, 2.0% | 5 (6.0%) | 0.89%, 11% | 5 (3.8%) | 0.54%, 7.2% | ||
no | 311 (99.0%) | 98%, 100% | 79 (94.0%) | 89%, 99% | 125 (96.2%) | 93%, 99% | ||
Inpatient days | 2.6 (1.2) | 2.4, 2.7 | 3.7 (1.4) | 3.4, 4.0 | 3.6 (1.4) | 3.4, 3.9 | 98 | <0.001 |
Note: 1n (%); Mean (SD); Median (IQR); Minimum Maximum; 2CI - Confidence Interval; 3Pearson's Chi-squared test; Kruskal-Wallis rank sum test; IVF – in vitro fertilization; VD – vaginal delivery; CS – cesarean section. | ||||||||
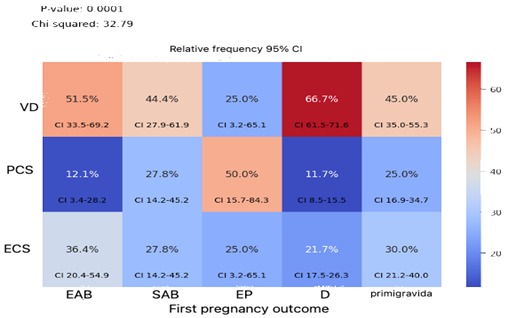
There are significant variations in the mode of delivery based on the outcomes of the first pregnancy (p=0.0001), which show that participants whose first pregnancy ended in delivery had a VD rate of 66.7% (95% CI: 61.5% - 71.6%) and an ECS rate of 21.7% (95% CI: 17.5% - 26.3%), compared to participants whose first pregnancy ended in miscarriage, where 51.5% (95% CI: 33.5% - 69.2%) had a VD and 36.4% (95% CI: 20.4% - 54.9%) had an ECS. This highlights the higher rate of VD among participants whose first birth ended in delivery compared to primipara and primigravidae, emphasizing the role of first pregnancy outcomes on the mode of delivery in subsequent pregnancies (Figure 1).
|
Fig. 1 Relationship between the mode of delivery and the results of the first pregnancy. Note: VD – vaginal delivery, PCS – planned cesarean section, ECS – emergency cesarean section, EAB – elective abortion, SAB – spontaneous abortion, EP – ectopic pregnancy |
The same situation is observed in the comparative evaluation of the mode of delivery for the first and present pregnancy delivery, revealing that 73.5% (95% CI: 68.2% - 78.3%) of participants whose first pregnancy ended in VD subsequently had a VD, compared to 16.7% (95% CI: 7.0% - 31.4%) for those whose first pregnancy ended in CS. Conversely, among participants who had a CS, 8.4% (95% CI: 5.6% - 12.1%) had a PCS and 18.1% (95% CI: 14.0% - 22.9%) had an ECS among those whose first pregnancy ended in VD, compared to 35.7% (95% CI: 21.6% - 52.0%) by PCS and 47.6% (95% CI: 32.0% - 63.2%) by ECS among those whose first pregnancy ended in CS. Of interest is that 45.2% (95% CI: 37.7% - 52.8%) of nulliparae had VD, 24.3% (95% CI: 18.2% - 31.3%) by PCS, and 30.5% (95% CI: 23.8% - 37.9%) by ECS (Fig. 2). These results show significant statistical variations (p=0.0000), demonstrating the importance of obstetrical history on the mode of delivery. It is evident that these data could potentially be influenced by elective CS.
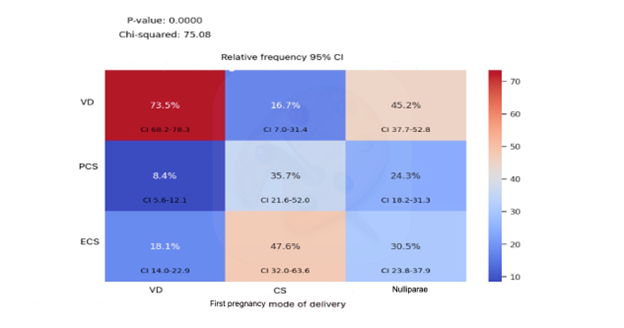 |
Fig. 2 Relationship between mode of first and present pregnancy delivery Note: VD – vaginal delivery, CS – cesarean section, PCS – planned cesarean section, ECS – emergency cesarean section. |
The evaluation of the relationship between mode of delivery and a series of parameters revealed significant statistical differences for pregnancy complications (p=0.003), delivery complications (p<0.001), gestational age (p=0.017), Apgar score at 1 minute (p<0.001), Apgar score at 5 minutes (p<0.001), multiple pregnancy (p=0.016), and length of hospital stay (p<0.001) (Table 3).
Further exploration through multivariate analysis based on multiple parameters such as mode of delivery, obstetrical history, and pregnancy complications found significant statistical deviations (p=0.004, Chi2=11.06049) among participants with complicated obstetric history and pregnancy complications, who had PCS in 85.4% (95% CI: 74.5% - 96.2%) and ECS in 86.7% (95% CI: 78.1% - 95.3%), compared to participants without complicated obstetric history and pregnancy complications, who delivered via PCS in 62.8% (95% CI: 48.3% - 77.2%) and ECS in 77.1% (95% CI: 67.3% - 87%), highlighting the role of complicated obstetric history in the rate of CS (Table 4).
Table 4. Relationship between mode of delivery and obstetrical history and pregnancy complications | |||||
Pregnancy complications | % | 95% CI2 | Statistic Test | p-value3 | |
Complicated obstetric history | Mode of delivery | ||||
Yes | VD | 64.5 | 55.9%, 73.0% | M^2 = 11.06049, dof = 2 | 0.004 |
PCS | 85.4 | 74.5%, 96.2% | |||
ECS | 86.7 | 78.1%, 95.3% | |||
No | VD | 66.3 | 59.7%, 73.0% | ||
PCS | 62.8 | 48.3%, 77.2% | |||
ECS | 77.1 | 67.3%, 87.0% | |||
Note: 2CI - Confidence Interval; 3Pearson's Chi-squared test; Kruskal-Wallis rank sum test; VD – vaginal delivery, PCS – planned cesarean section, ECS – emergency cesarean section. | |||||
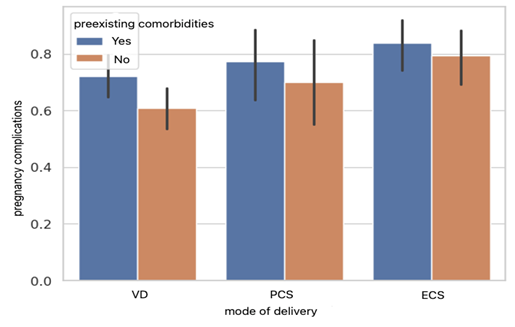
Results of the evaluation of the relationship between mode of delivery, pre-existing chronic conditions, and pregnancy complications reveal significant statistical deviations (p=0.0042, Chi2 test=10.9559). Among participants with pregnancy complications and pre-existing chronic conditions, 72.2% (95% CI: 64.6% - 79.8%) had VD, compared to 60.8% (95% CI: 53.7% - 67.9%) of participants without pre-existing chronic conditions. Additionally, participants with pregnancy complications and pre-existing chronic conditions delivered via PCS in 77.3% (95% CI: 64.9% - 89.7%), compared to 70% (95% CI: 55.8% - 84.2%) of those without pre-existing chronic conditions. Furthermore, participants with pregnancy complications and pre-existing chronic conditions who had ECS constituted 83.9% (95% CI: 74.7% - 93.0%), compared to 79.4% (95% CI: 69.8% - 89.0%) of participants without pre-existing chronic conditions (Fig. 3).
|
Fig. 3 Relationship between mode of delivery and pre-existing chronic conditions and delivery complications Note: VD – vaginal delivery, PCS – planned cesarean section, ECS – emergency cesarean section. |
Discussions
This study aimed to analyze the rates of vaginal and cesarean deliveries among women of advanced reproductive age based on sociodemographic, anthropometric, medical, and obstetrical characteristics and to assess their relationship. The study evaluated the effects of age on the mode of delivery in women of advanced reproductive age, with results showing an increased rate of CS based on several determinant factors. These findings are consistent with recent studies suggesting that advanced reproductive age is a potential risk factor for higher rates of CS and a higher incidence of obstetrical complications. [11, 12].
Results found increased rates of CS, specifically 15,9% (95% CI: 13% - 19%) of participants delivered via PCS and 24.6% (95% CI: 21% - 28%) via ECS. These findings are supported by research indicating that the mean maternal age tends to correlate with higher rates of CS, with older women being more likely to deliver via CS [24]. According to an American study, the incidence of CS increased with maternal age (under 25 years, 11.6%; over 40 years, 43.1%) [24]. Women aged over 25 had a 3.6% chance of CS, while those over 40 had a 21.1% chance. In a German study, 77.1% of women over 22 years old and 53.1% of those over 32 years old delivered spontaneously, whereas 14.5% of women under 22 and 32.3% of those over 32 underwent CS [25].
The evaluation of the relationship between mode of delivery and pregnancy complications (p=0.003) and delivery complications (p<0.001) reveals statistically significant differences. The lowest rate of pregnancy complications is observed in participants who had VD, constituting 65.6% (95% CI: 60% - 71%), compared to the highest rate of 81.5% (95% CI: 75% - 88%) observed in participants who had ECS. Additionally, the association with pre-existing chronic conditions in the multivariate analysis shows the highest rate of ECS at 83.9% (95% CI: 74.7% - 93.0%) in participants with pre-existing chronic conditions, compared to 79,4% (95% CI: 69.8% - 89.0%) in participants without pre-existing chronic conditions, and 77.3% (95% CI: 64.9% - 89.7%) in participants with pre-existing chronic conditions via PCS, compared to 70% (95% CI: 55.8% - 84.2%) in participants without pre-existing chronic conditions.
Complications during pregnancy and pre-existing chronic conditions are potential indicators for cesarean section among women of advanced reproductive age. Recent studies have indicated that pregnant women with medical conditions such as hypertensive disorders, diabetes mellitus, mild renal insufficiency, and multiple sclerosis tend to opt for repeat CS, suggesting that pregnancy complications influence the choice of mode of delivery [26]. All this evidence underscores the importance of managing pre-existing chronic conditions during family planning and antenatal care to reduce the rate of CS among women of advanced reproductive age. It highlights the significance of antenatal care and consultations with obstetricians in determining the appropriate delivery approach, aiming to lower the rate of ECS among participants with pregnancy complications.
Supporting this finding are the results of the evaluation of the mode of delivery based on delivery complications, which indicate that the rate of women who experienced birth complications is twice as low in participants who had PCS compared to those who had VD or ECS. This rate is 25% (95% CI: 16% - 34%) for participants who had PCS, compared to 53.8% (95% CI: 48% - 59%) and 59.2% (95% CI: 51% - 68%) for participants who had VD or ECS, respectively.
Even though there are recognized clinical indicators for opting for CS, non-clinical factors often play a significant role in the decision-making process. It is important to consider the risks associated with subsequent pregnancies and deliveries due to the decision to undergo CS in the absence of medical indications. Pregnant women with a history of CS are at higher risk of developing various complications such as placenta previa, uterine rupture, postpartum hemorrhage, hysterectomy, preterm birth before 37 weeks of gestation, fetal distress, hypertension, and gestational diabetes [27]. The basis of the decision about the mode of delivery often lies in the interaction between the woman and the healthcare provider, and there is a probability that the woman's preferences and beliefs about childbirth, as well as the clinician's subjective assessment of her obstetric risks and perception of the preferred mode of delivery, influence the choice to give birth by CS [28].
Respecting human rights by ensuring each woman's right to complete and accurate information about the risks associated with pregnancy and childbirth at advanced reproductive age empowers women to make informed decisions and actively participate in their health decision-making process. The study's results found that the rate of participants who were informed before becoming pregnant is approximately twice as high as those who were informed during pregnancy, comprising 59.5% (95% CI: 49% - 70%) and 28.6% (95% CI: 19% - 38%) for PCS, and 50.8% (95% CI: 42% - 59%) and 33.8% (95% CI: 26% - 42%) for ECS. In comparison, participants who had VD had similar rates of being informed either before becoming pregnant or during pregnancy, 38.9% (95% CI: 33% - 44%) and 38.5% (95% CI: 33% - 44%). These data demonstrate the impact of information about the risks associated with advanced reproductive age on the decision to give birth in this category of women.
Of course, particular attention is given to understanding and interpreting the information received, as well as the method of information delivery, since risks are often perceived differently by women and healthcare providers. The doubled rate of antenatal information among women who gave birth via CS may result from a high level of responsibility and pregnancy planning among women at increased risk, or an exaggerated interpretation of risk information leading to elective CS. In this regard, an evidence-based tool called the Safe Motherhood Initiative has been implemented by most World Health Organization-associated countries for nearly 30 years [29, 30]. According to WHO recommendations, pregnant women should have at least four antenatal attendances, as the use of antenatal care plays a significant role in the decision-making process regarding the mode of delivery. Women who underwent more than 4 antenatal attendances more often undergo CS, though the exact cause of this phenomenon remains unknown. Additionally, there is a probability that a cautious approach to women with pregnancy difficulties contributed to the preference for CS. The goal of antenatal care is to reduce health risks, identify anomalies early in pregnancy, and, if necessary, take corrective measures to prepare both mother and fetus, ensuring a healthy start in life for every newborn [31]. In 2016, the World Health Organization (WHO) suggested that antenatal care be increased from four to eight consultations with medical professionals during pregnancy. Compared to the previous four attendances, the aim of increasing the number of antenatal attendances is to reduce perinatal deaths by 8 per 1000 live births [32].
The study results also found that women who had regular GP attendances had a significantly higher likelihood – by 50% – of giving birth vaginally compared to those who did not have such attendances (p=0,02). At the same time, there were no statistically significant differences in evaluating the impact of GP attendances in the first trimester or later on the mode of delivery (p=0.5). A different situation was observed in the evaluation of the relationship between the number of GP attendances (p<0.001) or the number obstetrician’s attendances (p=0.032) and the mode of delivery, which showed statistically significant deviations. The ratio between the rate of women who had 4-7 GP attendances compared to 1-3 varied between 1.16 attendances for participants with VD and 2.4 for those with ECS, constituting 1.6 for participants with PCS.
A similar trend was observed in the evaluation of services provided by the obstetrician, which found that the proportion of participants who had more than 3 obstetrician attendances was approximately twice as high among participants with PCS and ECS compared to those who had up to 3 attendances and was approximately identical among participants who gave birth vaginally.
In the absence of other evidence and analyses of associated characteristics, this finding can be interpreted ambiguously. One viable interpretation is that higher attendance at antenatal care services by women with high-risk pregnancies influences the increase in the rate of CS. Additionally, without evaluating the reasons for this high GP and obstetrician attendance, there is a possibility that the increased rate of CS is due to voluntary attendance of participants without medical indications, leading to elective cesareans. Furthermore, consideration must be given to the possibility of overdiagnosis caused by medical staff's desire to prevent pregnancy and delivery complications, given that advanced reproductive age is a risk factor.
The evaluation of the impact of the mode of first delivery on subsequent deliveries identified statistically significant differences (p<0.001), indicating a probability approximately 2 times higher for VD among women whose first delivery ended vaginally, compared to a probability approximately 8 times higher for cesarean delivery among women whose first delivery ended in a CS. This demonstrates the impact of a CS history on subsequent pregnancies.
As reported in several studies, a previous CS has been predictably associated with a subsequent CS. According to a study from Brazil, a previous CS was linked to cesarean delivery in the current pregnancy [33]. Published research also indicates that women who have previously undergone a CS are more likely to experience placenta previa, placental abruption, and uterine rupture in subsequent pregnancies [34].
A significant aspect is the interrelation between the mode of delivery and parity, noting statistically significant differences (p<0.001) and revealing that every 6th woman who delivers vaginally is primipara, compared to every 3rd woman who delivers by ECS, and every 2 out of 5 who deliver by PCS. Supporting these findings, several studies highlight that the risk of CS, including ECS, in women of advanced reproductive age is considerably higher in primipara women, whereas the risk of preeclampsia is significantly higher in multipara women [35]. Like other studies, we found that the effects of increasing age were significantly more pronounced among primipara women than among multipara women [36]. This difference could be influenced by the higher likelihood of older primipara women opting for elective CS [37]. Some studies indicate that the risk of CS increases with age among both nulliparous and multipara women [38]. These findings may result from the higher probability of younger women being healthier and not suffering from preexisting chronic conditions that pose potential risks for pregnancy and delivery. Additionally, the influence of institutional culture and the expertise level of the healthcare provider could potentially affect women's decision-making processes regarding the mode of delivery [39].
Furthermore, in accordance with a previous study, our research demonstrated a positive correlation between maternal age and the likelihood of preterm birth (p=0.007) [40].
Conclusions
Our study identified the influence of biopsychosocial factors on the mode of delivery. Pregnancy at advanced reproductive age is associated with an increased rate of CS. Factors such as area of residence and education were found to have a significant impact on the mode of delivery. Women with higher levels of education are more likely to opt for CS. Previous CS, parity, pregnancy and delivery complications, and preexisting chronic conditions were also identified as contributing factors to CS. Proper information about pregnancy risks and the importance of antenatal care, including managing preexisting chronic conditions, plays a significant role in preventing adverse pregnancy and birth outcomes in this age group. These results highlight that advanced reproductive age can be an individual risk factor, emphasizing that providing detailed information to mothers over 35 about factors affecting pregnancy outcome improves them, particularly for primipara women.
Competing interests
None declared.
Authors’ contributions
RS conceptualized the project, drafted the first manuscript and interpreted the data. LS added some conceptual ideas and critically revised the manuscript. Both authors revised and approved the final version of the manuscript.
Acknowledgements and funding
The study had no external funding.
Patient consent
Obtained.
Ethics approval
The study protocol was approved by the Research Ethics Committee of Nicolae Testemițanu State University of Medicine and Pharmacy, minutes No.16, from 13th of February 2012.
Authors’ ORCID IDs
Rodica Scutelnic – https://orcid.org/0009-0006-1081-3429
Larisa Spinei – https://orcid.org/0000-0002-5370-9801
References
Organization for Economic Co-operation and Development Family database. Age of mothers at childbirth and age-specific fertility [Internet]. Paris: OECD; 2022- [cited 2024 Jun 5]. Available from: https://www.oecd.org/content/dam/oecd/en/data/datasets/family-database/…
Bréart G, Barros H, Wagener Y, Prati S. Characteristics of the childbearing population in Europe. Eur J Obstet Gynecol Reprod Biol. 2003;111 Suppl 1:S45-S52. doi: 10.1016/j.ejogrb.2003.09.005.
Statista.com. Average age of mothers in Europe 2022, by country [Internet]. London: Statista.com; 2022 [cited 2024 Jun 1]. Available from: https://www.statista.com/statistics/612088/mean-age-of-woman-at-childbi…
Hamilton BE, Martin JA, Osterman MJK. Births: provisional data for 2019. Vital Statistics Rapid Release: Report No 008, May 2020 [Internet]. Hyattsville, Maryland: National Center for Health Statistics; 2020 [cited 2024 Jun 1]. Available from: https://www.cdc.gov/nchs/data/vsrr/vsrr-8-508.pdf?ref=stanfordreview.org
Laopaiboon M, Lumbiganon P, Intarut N, et al. Advanced maternal age and pregnancy outcomes: a multicountry assessment. BJOG. 2014;121(Suppl 1):49-56. doi: 10.1111/1471-0528.12659.
Sauer MV. Reproduction at an advanced maternal age and maternal health. Fertil Steril. 2015;103(5):1136-43. doi: 10.1016/j.fertnstert.2015.03.004.
Kawwass JF, Badell ML. Maternal and fetal risk associated with assisted reproductive technology. Obstet Gynecol. 2018;132(3):763-772. doi: 10.1097/AOG.0000000000002786.
Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS One. 2016;11(2):e0148343. doi: 10.1371/journal.pone.0148343.
Gibbons L, Belizan JM, Lauer JA, Betran AP, Merialdi M, Althabe F. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: overuse as a barrier to universal coverage. World Health Report. 2010;30:1-31.
Gerli S, Favilli A, Pericoli S, Di Renzo GC. Re: Moore EK, Irvine LM. The impact of maternal age over forty years on the caesarean section rate: six year experience at a busy district general hospital. J Obstet Gynaecol. 2015;35(4):435. doi: 10.3109/01443615.2014.960825.
Frederiksen LE, Ernst A, Brix N, et al. Risk of adverse pregnancy outcomes at advanced maternal age. Obstet Gynecol. 2018;131(3):457-463. doi: 10.1097/AOG.0000000000002504.
Marozio L, Picardo E, Filippini C, et al. Maternal age over 40 years and pregnancy outcome: a hospital-based survey. J Matern Fetal Neonatal Med. 2019;32(10):1602-1608. doi: 10.1080/14767058.2017.1410793.
Klemetti R, Gissler M, Sainio S, Hemminki E. At what age does the risk for adverse maternal and infant outcomes increase? Nationwide register-based study on first births in Finland in 2005-2014. Acta Obstet Gynecol Scand. 2016;95(12):1368-1375. doi: 10.1111/aogs.13020.
Goetzinger KR, Shanks AL, Odibo AO, Macones GA, Cahill AG. Advanced maternal age and the risk of major congenital anomalies. Am J Perinatol. 2017;34(3):217-222. doi: 10.1055/s-0036-1585410.
Lean SC, Derricott H, Jones RL, Heazell AEP. Advanced maternal age and adverse pregnancy outcomes: a systematic review and meta-analysis. PLoS One. 2017;12(10):e0186287. doi: 10.1371/journal.pone.0186287.
Xie M, Lao TT, Du M, et al. Risk for Cesarean section in women of advanced maternal age under the changed reproductive policy in China: a cohort study in a tertiary hospital in southwestern China. J Obstet Gynaecol Res. 2019;45(9):1866-1875. doi: 10.1111/jog.14048.
Nuthalapaty FS, Rouse DJ. The impact of obesity on obstetrical practice and outcome. Clin Obstet Gynecol. 2004;47(4):898-981. doi: 10.1097/01.grf.0000135358.34673.48.
Keag OE, Norman JE, Stock SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: systematic review and meta-analysis. PLoS Med. 2018;15(1):e1002494. doi: 10.1371/journal.pmed.1002494.
Bowman ZS, Smith KR, Silver RM. Cesarean delivery and risk for subsequent ectopic pregnancy. Am J Perinatol. 2015;32(9):815-820. doi: 10.1055/s-0034-1543952.
Saeed KB, Greene RA, Corcoran P, O'Neill SM. Incidence of surgical site infection following caesarean section: a systematic review and meta-analysis protocol. BMJ Open. 2017;7(1):e013037. doi: 10.1136/bmjopen-2016-013037.
World Health Organization. WHO statement on Caesarean section rates [Internet]. Geneva: WHO; 2015 [cited 2023 Nov 15]. Available from: https://iris.who.int/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pd…
Green B, Evans J, Subair S, Liao LM. Maternal request for caesarean section: audit of a care pathway. J Obstet Gynaecol. 2014;34(4):317-321. doi: 10.3109/01443615.2013.873776.
Mazzoni A, Althabe F, Liu NH, et al. Women's preference for caesarean section: a systematic review and meta-analysis of observational studies. BJOG. 2011;118(4):391-399. doi: 10.1111/j.1471-0528.2010.02793.x.
Bayrampour H, Heaman M. Advanced maternal age and the risk of cesarean birth: a systematic review. Birth. 2010;37(3):219-226. doi: 10.1111/j.1523-536X.2010.00409.x.
Voigt M, Rochow N, Zygmunt M, Straube S, Schneider KT, Briese V. Risks of pregnancy and birth, birth presentation, and mode of delivery in relation to the age of primiparous women. Z Geburtshilfe Neonatol. 2008;212(6):206-210. doi: 10.1055/s-0028-1098732.
Sindiani A, Rawashdeh H, Obeidat N, Zayed F, Alhowary AAA. Factors that influenced pregnant women with one previous caesarean section regarding their mode of delivery. Ann Med Surg (Lond). 2020;55:124-130. doi: 10.1016/j.amsu.2020.05.007.
Chen X, Gao J, Liu J, Hu J, Li S, Tang Y, Zhong M, He J, Liao S, Yang J, Liu X, Wang X, Liu X, Liu X, Cao Y, Wang T, Liu C, Sun J. Previous mode of delivery affects subsequent pregnancy outcomes: a Chinese birth register study. Ann Transl Med. 2021;9(14):1135. doi: 10.21037/atm-20-8127.
Nguyen MT, McCullough LB, Chervenak FA. The importance of clinically and ethically fine-tuning decision-making about cesarean delivery. J Perinat Med. 2017;45(5):551-557. doi: 10.1515/jpm-2016-0262.
World Health Organization. World Health Day Safe Motherhood [Internet]. Geneva: WHO; 1998 [cited 2023 Nov 15]. Available from: https://www.who.int/docstore/world-health-day/en/docum ents1998/whd98.pdf
Diniz CSG, Rattner D, d’Oliveira AFPL, Aguiar JM, Niy DY. Disrespect and abuse in childbirth in Brazil: social activism, public policies and providers’ training. Reprod Health Matters. 2018;26(53):19-35. doi: 10.1080/ 09688080.2018.1502019.
World Health Organization. Provision of effective antenatal care: integrated management of pregnancy and childbirth. Geneva: WHO; 2002.
World Health Organization. Pregnant women must be able to access the right care at the right time, says WHO [Internet]. Geneva: WHO; 2016 [cited 2023 Nov 15]. Available from: https://www.who.int/news-room/detail/07-11-2016-pregnant-women-must-be-…
Osava RH, Silva FM, Tuesta EF, Oliveira SM, Amaral MC. Cesarean sections in a birth center. Rev Saude Publica. 2011;45(6):1036-1043. doi: 10.1590/s0034-89102011000600005. Erratum in: Rev Saude Publica. 2012 Aug;46(4):759.
Getahun D, Oyelese Y, Salihu HM, Ananth CV. Previous cesarean delivery and risks of placenta previa and placental abruption. Obstet Gynecol. 2006;107(4):771-778. doi: 10.1097/01.AOG.0000206182.63788.80.
Ogawa K, Urayama KY, Tanigaki S, et al. Association between very advanced maternal age and adverse pregnancy outcomes: a cross sectional Japanese study. BMC Pregnancy Childbirth. 2017;17(1):349. doi: 10.1186/s12884-017-1540-0.
Kenny LC, Lavender T, McNamee R, O'Neill SM, Mills T, Khashan AS. Advanced maternal age and adverse pregnancy outcome: evidence from a large contemporary cohort. PLoS One. 2013;8(2):e56583. doi: 10.1371/journal.pone.0056583.
Fitzpatrick KE, Tuffnell D, Kurinczuk JJ, Knight M. Pregnancy at very advanced maternal age: a UK population-based cohort study. BJOG. 2017;124(7):1097-1106. doi: 10.1111/1471-0528.14269.
Bergholt T, Skjeldestad FE, Pyykönen A, et al. Maternal age and risk of cesarean section in women with induced labor at term: a Nordic register-based study. Acta Obstet Gynecol Scand. 2020;99(2):283-289. doi: 10.1111/aogs.13743.
Kwayke-Ackah G, Burger A, de la Vega G, Kainz G, Rochon M, Quiñones JN. Influence of maternal age in mode of delivery after term induction of labor. J Matern Fetal Neonatal Med. 2022;35(7):1258-1263. doi: 10.1080/14767058.2020.1745180.
Koo YJ, Ryu HM, Yang JH, et al. Pregnancy outcomes according to increasing maternal age. Taiwan J Obstet Gynecol. 2012;51(1):60-65. doi: 10.1016/j.tjog.2012.01.012.