Introduction
Today, the COVID-19 pandemic continues to have a significant impact worldwide, as the global scientific community remains focused on discovering new therapeutic approaches, identifying mortality predictors, and implementing these findings into clinical practice. The goal is to achieve better clinical outcomes, manage symptoms effectively, and reduce both critical complications and overall mortality rates [1].
Ozone therapy is a promising complementary treatment with a wide range of therapeutic applications [2]. A systematic review of the literature indicates that ozone therapy can be used as a monotherapy or as a complementary treatment to standard protocols for COVID-19 patients. The scientific evidence suggests that this therapy has contributed to improvements in clinical symptoms, paraclinical markers, and radiological signs of inflammation, all without significant side effects [3].
Oxygen-ozone therapy, due to its antioxidant, anti-inflammatory, and antithrombotic properties, may play a crucial role in combating hyperinflammation, immunodeficiency, hypercoagulability, and poor response to conventional therapies induced by COVID-19. Based on the studies published so far, researchers suggest that oxygen-ozone treatment might be a promising adjunctive therapy for mild to severe cases of SARS-CoV-2 infection [4, 5].
Despite encouraging preliminary results from clinical studies and expert opinions, there is still not enough evidence to prove that ozone therapy is a viable treatment for COVID-19 [1, 5]. Therefore, to confirm ozone therapy as a feasible complementary treatment for COVID-19, to guide further clinical applications, and to assess its effect on the progression of SARS-CoV-2 infection, randomized controlled trials are needed [6].
In this context, the purpose of the study is to assess the clinical efficacy of ozone treatment (major ozonated autohemotherapy) in patients with SARS-CoV-2.
Material and methods
The present study was carried out at the Valeriu Ghereg Anesthesiology and Resuscitation Department No.1 of Nicolae Testemițanu State University of Medicine and Pharmacy, Republic of Moldova.
To assess the efficacy of ozone therapy (major ozonized autohemotherapy – MAH) in patients with SARS-CoV-2, a prospective, randomized clinical study was conducted. This research evaluated the clinical features of COVID-19 patients based on their treatment regimen (either conventional treatment alone or conventional treatment combined with ozone therapy).
The study included patients aged 18 and older with COVID-19 who were admitted to the Intensive Care Unit (ICU) of the Emergency Medicine Institute (IMU) from July 2020 to February 2021. The author identified the patients for the study at the time of their admission to IMU. All patients admitted during the reference period who met the inclusion criteria were enrolled in the study.
To improve the accuracy of sample size calculation and increase precision, the Chi-squared power test was used. The data analysis focused on testing the hypothesis that ozone therapy is related to survival, using the following parameters:
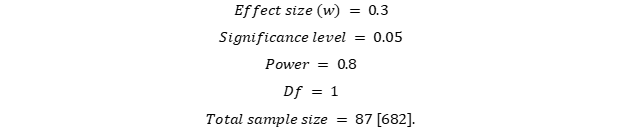
For a 95.0% confidence interval, the required sample size was calculated to include at least 87 patients. The representative study sample involved 100 patients for a 5% margin of error, thus, exceeding the minimum threshold of 88 patients. The patients were randomly divided into two groups with a 1:1 ratio: 50 COVID-19 patients were treated based on the National Clinical Protocol combined with ozone therapy (major ozonated autohemotherapy) in the COVID-19 ICU of IMU (main study group), and 50 COVID-19 patients received only the conventional treatment as outlined in the National Clinical Protocol in the COVID-19 ICU of IMU (control group).
The study was conducted in several stages:
Stage 1: Patients included in the study underwent clinical and paraclinical assessments (including laboratory and instrumental diagnostic methods).
Stage 2: Statistical processing of the results obtained.
Stage 3: Evaluation of the main indicators characterizing the study groups. Comparative assessment of clinical features, biochemical and imaging indicators depending on the treatment method. Improving the treatment algorithm for COVID-19 patients.
Stage 4: Data presentation.
Inclusion in the study required written informed consent from each patient for the investigations, treatment, collection of relevant clinical data, and outcome assessment.9
To provide greater research accuracy, a set of inclusion and exclusion criteria was used to define the study parameters and thus focusing on a specific representative group.
Inclusion criteria for the study were as following:
Patients diagnosed with COVID-19 based on WHO guidelines and confirmed by real-time reverse transcription polymerase chain reaction (RT-PCR) for SARS-CoV-2 RNA from nasopharyngeal swabs (a molecular biology technique).
Patients with COVID-19 aged ≥18 years.
Patients with COVID-19 who have a mildly reduced oxygenation index (PaO2/FiO2 >200-≤300 mmHg) and SpO2 levels between 88-96%.
Patients with COVID-19 with radiologically confirmed pneumonia and a Brixia score within 6-10 points.
Patients without contraindications for systemic ozone therapy.
Patients who have read and signed the informed consent for participation in the study.
Exclusion criteria for the study included:
Patients under 18 years old.
Patients with multiple organ failure syndrome.
Pregnant women, postpartum women, and breastfeeding women.
Patients on immunosuppressive therapy.
Individuals undergoing mechanical ventilation at the time of study enrollment.
Patients with contraindications for systemic ozone therapy.
Patients who refused to participate in the study.
The cases were randomized using block randomization procedures. According to the estimated sample size, 100 consecutive patients (who were not excluded) were selected for analysis and allocated to one of two groups: (a) the experimental group or (b) the control group. The study is based on the hypothesis that early systemic oxygen-ozone therapy may be effective in improving disease progression and/or partially improving the onset of "cytokine storm" syndrome, at least partially, having a significant impact on patient prognosis.
Upon confirming eligibility, patients with COVID-19 were fully informed about the study's purpose, objectives, the benefits and risks associated with the research and the treatment, the expected outcomes, as well as the practical applications of the study.
Standard medical care and monitoring for all COVID-19 patients were administered in accordance with national and institutional protocols for inpatient and outpatient management of this patient population.
The study protocol was approved by the Research Ethics Committee of Nicolae Testemițanu State University of Medicine and Pharmacy (Minutes No. 1 dated 20.07.2020).
All patients included in the study were examined using the following research methods:
Clinical methods. Clinical, biochemical, and imaging indicators were assessed, as well as rates of invasive and non-invasive mechanical ventilation, mortality rates, and length of hospital stay. Data were collected from medical records, including initial and follow-up visits, as well as clinical, instrumental, and laboratory investigations conducted both during and after treatment. The data were then analyzed comparatively, assessing changes over time between the two study groups.
Treatment methods. The standard treatment for patients infected with SARS-CoV-2 in ICU followed the guidelines set forth in the National Clinical Protocol, Provisional Editions III and IV [7, 8], and the Practical Guide for Managing Severe Complications from COVID-19 [9].
Ozone therapy included:
Conventional or standard treatment.
MAH – the intravenous infusion of ozonated autologous whole blood under strict aseptic and antiseptic conditions. Specifically, 80-120 ml of venous blood mixed with 10 ml of 3.13% sodium citrate solution (as an anticoagulant) was enriched with a gas mixture of oxygen and ozone at a 1:1 ratio, with an ozone concentration of 40 µgN/mL. The mixture was thoroughly agitated for 5 minutes. Following ozonation, the blood was reinfused into the same vein over approximately 10-15 minutes. This procedure was repeated 7 times, with one session every 24 hours for 7 consequent days [10]. The ozone was generated by the Medozon Herrman medical device.
All ozone therapy methods used in patients with COVID-19 comply with the recommendations of the World Federation of Oxygen and Ozone Therapy (WFOT Review of Evidence-Based Ozone Therapy) and international guidelines (The International Scientific Committee of Ozone Therapy “Madrid Declaration on Ozone Therapy”) and are included into the ozone generator software [5].
Clinical assessment. Fever was defined as an armpit temperature of ≥37.5°C [2]. Clinical improvement was characterized by a two-point reduction on a 6-point severity scale [11] (while comparing the patient's condition on the first day in the ICU), either upon transfer from the ICU to the COVID-19 ward, at discharge, or at the time of death:
6 points = death
5 points = hospitalization for invasive mechanical ventilation
4 points = hospitalization for non-invasive ventilation or high-flow oxygen therapy
3 points = hospitalization for oxygen therapy (excluding high-flow oxygen therapy or non-invasive ventilation)
2 points = hospitalization with no need for oxygen therapy
1 point = while the patient being transferred to the COVID-19 ward, met the discharge criteria, or discharged from the hospital alive.
Table 1. Standard Treatments for SARS-CoV-2 Infected Patients in the ICU | |
|
|
| Methylprednisolone: Administer 0.75 to 2 mg/kg/day (based on the CRP level at admission, divided into two doses as determined by the attending physician). |
| Enoxaparin: Administer 4000 IU (40 mg) subcutaneously twice daily. |
| Antibiotic options included macrolides, second- and third-generation cephalosporins, and carbapenems. Doses and treatment length were customized based on the attending physician's decision. |
|
|
| Fluid intake restriction, by maintaining a mean arterial pressure above 60 mmHg, the urinary output greater than 0.5 ml/kg/h, with no increase in nitrogen retention by-products, as well as the hematocrit level at 30%. |
Note: ICU- intensive care unit; HFNC- High-Flow Nasal Cannula; NIV- Non-Invasive Ventilation; MV- Mechanical Ventilation; CRP- C-reactive protein; Enoxaparin 4000IU- Anti Xa IU/0,4 ml. | |
The discharge criteria showed a clinical recovery, including fever management, respiratory rate of <24 breaths per minute, oxygen saturation >94% on FiO2 of 0.21%, and no cough for at least 72 hours [11].
One study objective was to measure the time to clinical improvement within 28 days, defined as the time (in days) from study randomization to the day of a 2-point decline on a 6-point ordinal scale (from 1 = discharge to 6 = death) or discharge from hospital alive, whichever occurred first [11].
Decisions regarding invasive mechanical ventilation and non-invasive ventilation were made based on clinical standards and the medical consultant's assessment.
Biochemical methods. Hematological tests were conducted, including a complete blood count (CBC), counts of lymphocytes and neutrophils, the neutrophil-to-lymphocyte ratio (NLR), and platelet count. Biochemical assessments included procalcitonin (PCT), C-reactive protein (CRP), creatinine, urea, electrolytes (sodium and potassium), total bilirubin, aspartate aminotransferase (AST), creatine kinase (CK), fibrinogen, and D-dimers. These tests were performed using the HumaStar 300SR Mindray BS-240Pro automatic biochemical analyzer in the Biochemistry Laboratory at IMU [12].
D-dimer levels were measured using an immunofluorescence assay and reported in fibrinogen-equivalent units (μg/ml) [12].
The following biochemical test values were used for normal reference: D-dimers – <0.5 mg/mL, CRP – 0.8-3.0 mg/L, PCT – <0.5 ng/mL, and leukocytes – 4-10^9/L. Lymphocytopenia was characterized by a lymphocyte count <1500 cells per cubic millimeter of blood. Thrombocytopenia was identified as a platelet count <150,000 cells per cubic millimeter of blood.
X-ray imaging test. A chest X-ray was conducted using the SHIMADZU Mobile Art Evolution portable radiography unit. To assess the severity of COVID-19 pneumonia and guide the selection of appropriate ventilation support, the Brixia score was employed. This score offers a feasible and efficient semi-quantitative evaluation of COVID-19 severity, using an 18-point scale to classify lung involvement based on the type and extent of pulmonary abnormalities [13].
Statistical data processing methods. The primary study data were introduced into an electronic database and processed using functions and modules from SPSS version 16.0 for Windows (SPSS Inc., Belmont, CA, USA, 2008) and Microsoft Office Excel 2019 on a personal computer. Both descriptive and inferential statistical procedures were applied. Pearson's χ² test, Yates' correction, or Fisher's exact test were used to compare categorical variables. The t-test or non-parametric tests were applied to assess the statistical significance of mean differences between the study groups: one-way analysis of variance (ANOVA) was conducted, followed by post-hoc tests to explore multiple mean differences among the study groups; the correlation analysis was performed to determine the strength and direction of statistical associations. A bilateral p-value <0.05 was considered statistically significant.
Results and discussions
Additionally, to conventional treatment, ozone therapy has been proposed as an adjunctive treatment for SARS-CoV-2 infection, due to its therapeutic effects, including antioxidant, anti-inflammatory, antithrombotic, antiviral, and immunomodulatory properties. Oxygen-ozone therapy could play a crucial role in fighting off hyperinflammation, immunodeficiency, hypercoagulability, and inadequate response to treatments caused by COVID-19. Research findings suggest that ozone therapy could be a promising complementary treatment for SARS-CoV-2 infection, including both mild and severe cases [4, 11].
The study compared 50 ICU patients with COVID-19 who received both conventional treatment and ozone therapy (SG) with another 50 ICU patients treated exclusively with conventional methods (CG). The gender distribution was similar across both groups: the study group consisted of 22 men (44.0%) and 28 women (56.0%), while the control group had 23 men (46.0%) and 27 women (54.0%).
The mean age of patients was similar in both study groups: 58.08±9.9 years (ranging 28-73 years old) in SG and 62.36±11.6 years (ranging 34-84 years old) in CG.
The mean time from symptoms onset to ICU admission was also similar between the study groups: 6.86±4.3 days in COVID- 19 patients who underwent ozone therapy and 7.94±3.8 days in those receiving standard treatment (p>0.05).
The mean values for clinical assessments, PaO2/FiO2 ratio, blood parameters, NLR, CRP, PCT, urea (mmol/L), and the Brixia score were similar in both study groups. Several studies found that the mean overall hospital stay length was also similar between patients treated with ozone and those receiving standard treatment (p>0.05): 8 days vs. 28 days [11], 9.37±3.84 days vs. 9.37±5.38 days [14], and 8 days vs. 9 days [15]. The average hospital stay (17.80±8.9 days in the SG and 17.06±10.6 days in the CG, p>0.05) was not significantly different between the study groups. Similarly, the average ICU stay (8.56±5.3 days in the SG and 10.22±9.0 days in the CG, p>0.05) showed only a slight shorter-term trend in the SG.
Mortality rates among COVID-19 patients have varied significantly, from 3.6% to 26.0%, depending on the study sample and disease severity. Previous research has reported a range of mortality rates for patients requiring ICU admission, including 16%, 38%, 62%, 67%, and 78% [16, 17].
In the current study, the mortality rate for COVID-19 patients treated with ozone therapy in the ICU was notably lower, ranging from 12% to 24.0%, compared to 17% to 34.0% for those receiving conventional treatment. However, this difference did not reach a statistical significance (p>0.05). Similar findings have been reported in other prospective cohort and case-control studies: one study reported 11.0% mortality for patients treated with conventional therapy and ozone therapy vs. 22% for those receiving conventional therapy alone (p>0.05) [11, 18], while another study registered 0% mortality for those treated with both approaches compared to 7% for those treated conventionally alone (p>0.05) [14].
The use of oxygen therapy (35 - 70.0% of COVID-19 patients treated with ozone vs. 39 - 78.0% of patients treated conventionally, p>0.05), non-invasive ventilation (35 - 70.0% of patients treated with ozone vs. 38 - 76.0% treated conventionally, p>0.05), and invasive mechanical ventilation (11 - 22.0% of patients treated with ozone vs. 19 - 38.0% treated conventionally, p>0.05) indicated a decreasing trend in patients from the primary group, though it did not reach statistical significance.
The mean durations for oxygen therapy (8.20±5.4 days for ozone-treated patients vs. 9.77±8.7 days for conventionally treated patients, p>0.05), non-invasive ventilation (6.06±3.9 days for ozone-treated patients vs. 6.29±6.8 days for conventionally treated patients, p>0.05), and invasive mechanical ventilation (6.82±5.5 days for ozone-treated patients vs. 7.47±6.8 days for conventionally treated patients, p>0.05) also showed a non-significant decreasing trend in the ozone-treated group.
The treatment led to significant clinical improvements in both study groups. The average clinical improvement score decreased notably, from 3.66±0.5 points on day 1 to 2.52±1.6 points on day 7 (p<0.001) in the ozone therapy group (SG), and from 3.70±0.5 points on day 1 to 2.84±1.8 points on day 7 (p<0.001) in the conventional therapy group (CG). Clinical improvement, characterized by a decrease of two or more points in the score, was seen in 27 (54.0%) of COVID-19 patients treated with ozone and in 25 (50.0%) of those treated with conventional methods (p>0.05) (Table 1).
A research study revealed that, within 10 days of ozone treatment, there was a significant reduction in inflammatory and thromboembolic markers (PCR and D-dimers) with p-values ranging from <0.05 to <0.001, and a significant improvement in major respiratory indices (SpO2/FiO2 ratio). By day 10, all patients showed significant resolution of bilateral interstitial infiltrates [18].
In this study, the average oxygenation index – PaO2/FiO2 – increased significantly in the ozone therapy group (from 246.86±30.3 mm Hg on day 1 to 296.75±105.1 mm Hg on day 7 of treatment; p<0.01), whereas no change was observed in the control group (from 235.86±33.4 mm Hg on day 1 to 232.82±110.6 mm Hg on day 7; p>0.05). Despite similar initial values of the oxygenation index in both groups, the dynamic analysis demonstrated a clear efficacy of ozone treatment. At the end of the first week, the mean oxygenation index was significantly higher in the ozone therapy group compared to the standard treatment group: 296.8±105.1 mm Hg vs. 232.8±110.6 mm Hg (p<0.01). Additionally, the median absolute difference between the oxygenation index on the 7th day of ozone treatment and its initial value was positive – 53.5 (IQR -19.7 to 106) mm Hg, while the control group showed a negative difference of -19 (IQR -85.2 to 56.5) mm Hg (p<0.05). Thus, combined ozone therapy treatment showed a more positive trend in the oxygenation index compared to standard treatment.
Table 1. Clinical, laboratory, and imaging parameters (X±SD) for COVID-19 patients on day 1 and day 7 of treatment, within both study groups | ||||||||
Parameters | Study Group |
p | Control Group | p | p (Day 1) | p (Day 7) | ||
Day 1 | Day 7 | Day 1 | Day 7 | |||||
PaO2/FiO2 (mm Hg) | 246,86±30,3 | 296,75±105,1 | <0,01 | 235,86±33,4 | 232,82±110,6 | NS | NS | <0,01 |
PCR (mg/L) | 75,17±53,9 | 44,88±53,2 | <0,01 | 82,52±59,9 | 44,85±57,9 | <0,001 | NS | NS |
PCT (ng/mL) | 0,18±0,3 | 0,17±0,3 | NS | 0,13±0,1 | 0,14±0,2 | NS | NS | NS |
Brixia Score (points) | 8,30±1,6 | 7,48±4,0 | NS | 8,38±1,3 | 9,44±4,1 | NS | NS | <0,05 |
D-Dimers (µg/mL) | 0,98±0,8 | 2,58±2,9 | <0,01 | 1,98±2,5 | 2,97±2,9 | <0,05 | <0,01 | NS |
Fibrinogen (g/L) | 4,36±0,8 | 3,60±1,2 | <0,01 | 4,36±1,1 | 4,57±2,9 | NS | NS | <0,05 |
Leucocytes (x109/L) | 10,09±5,2 | 9,80±4,1 | NS | 9,25±4,5 | 11,79±7,9 | <0,01 | NS | NS |
Neutrophiles (%) | 71,68±13,3 | 72,08±12,8 | NS | 71,84±10,6 | 74,04±11,5 | NS | NS | NS |
Lymphocytes (%) | 10,42±6,5 | 11,77±7,3 | NS | 11,88±7,1 | 11,30±6,9 | NS | NS | NS |
RNL | 11,78±13,2 | 9,85±7,4 | NS | 9,02±5,9 | 10,74±9,0 | NS | NS | NS |
Monocyte s (x109/L) | 5,48±3,3 | 6,6±3,9 | NS | 5,66±3,0 | 5,58±3,7 | NS | NS | NS |
ESR (mm/h) | 26,22±15,9 | 28,65±16,6 | NS | 26,14±15,4 | 32,58±16,2 | <0,05 | NS | NS |
Platelets (x109/L) | 241,58±91,1 | 284,21±101,0 | <0,01 | 219,84±80,0 | 276,48±112,3 | <0,001 | NS | NS |
Hemoglobin (g/L) | 128,78±14,6 | 119,85±17,1 | <0,001 | 127,24±16,5 | 119,94±18,2 | <0,01 | NS | NS |
Albumin (g/L) | 36,52±4,1 | 31,77±4,1 | <0,001 | 34,80±5,7 | 30,68±4,3 | <0,001 | NS | NS |
Urea (mmol/L) | 7,41±3,4 | 7,32±2,9 | NS | 8,06±5,6 | 9,34±7,7 | <0,05 | NS | NS |
Creatinine (mmol/l) | 100,92±53,9 | 92,42±28,3 | NS | 107,66±63,1 | 99,88±75,5 | NS | NS | NS |
ALAT (U/l) | 52,34±61,8 | 68,58±53,2 | <0,05 | 48,04±33,2 | 67,64±58,8 | <0,01 | NS | NS |
ASAT (U/l) | 46,52±35,3 | 42,50±40,3 | NS | 51,82±39,6 | 42,84±33,1 | NS | NS | NS |
Clinical assessment (points) | 3,66±0,5 | 2,52±1,6 | <0,001 | 3,70±0,5 | 2,84±1,8 | <0,001 | NS | NS |
Note: SD – standard deviation; PaO2/FiO2 – partial pressure of oxygen/fraction of inspired oxygen; CRP – C-reactive protein; PCT – procalcitonin; N/L ratio – neutrophil-to-lymphocyte ratio; VSH – erythrocyte sedimentation rate; ALT – alanine aminotransferase; AST – aspartate aminotransferase; NS – not significant. Data are presented as mean values and standard deviation. Differences in mean values were assessed using the paired t-test or Wilcoxon test. | ||||||||
On the 7th day of treatment, COVID-19 patients from the SG showed a trend towards increased frequencies of normal PaO2/FiO2 ratios (21 - 43.8% and 14 - 28.0% of cases, respectively; p>0.05) and milder ARDS (PaO2/FiO2 >200-≤300 mmHg) (18 - 37.5% and 15 - 30.0% of cases, respectively; p>0.05). In contrast, patients with COVID-19 from the CG experienced a statistically significant increase in worsening ARDS (≤200 mmHg) (21 - 42.0% and 9 - 18.8% of cases, respectively; p<0.05). There was also an increasing trend in oxygenation impairment from moderate (15 - 30.0% and 7 - 14.6% of cases, respectively; p>0.05) to severe (6 - 12.0% and 2 - 4.2% of cases, respectively; p>0.05) in patients from CG.
The average Brixia score was similar between the two groups on day 1 (8.30±1.6 points in SG and 8.38±1.3 points in CG; p>0.05). By day 7, a decreasing trend in the Brixia score was reported towards in SG (7.48±4.0 points; p>0.05), while the CG showed an increasing trend (9.44±4.1 points; p>0.05). However, these changes did not achieve any statistical significance.
A reduced Brixia score in the main cohort was recorded in 50% of cases compared to 42% in the control group (p>0.05). Notably, patients treated with ozone showed a statistically significant improvement in radiological pulmonary findings by the 7th day compared to the control group. On the 7th day of treatment, the average Brixia score was significantly higher in the ozone treatment group (p<0.05). The median absolute change in the Brixia score was 0.5 (IQR – 2.0-3.0) points, compared to 0 (IQR – 4.0-2.0) points in the control group (p<0.05).
Increased levels of D-dimers, C-reactive protein (CRP), ferritin, and interleukin-6 (IL-6) serve as prognostic indicators for patients with COVID-19. These parameters have been associated to an unfavorable prognosis in several studies [10, 19].
In both study groups, there was a statistically significant decrease in the mean hemoglobin levels (128.78±14.6 g/L on day 1 and 119.85±17.1 g/L on day 7, p<0.001 in the study group; 127.24±16.5 g/L on day 1 and 119.94±18.2 g/L on day 7, p<0.01 in the CG) as well as in PCR values (75.17±53.9 mg/L on day 1 and 44.88±53.2 mg/L on day 7, p<0.01 in the SG; 82.52±59.9 mg/L on day 1 and 44.85±57.9 mg/L on day 7, p<0.001 in the CG).
In the SG group, there was a decreasing trend in the mean leukocyte count (10.09±5.2x10^9/L on day 1 and 9.80±4.1x10^9/L on day 7, p>0.05), whereas in the CG, a statistically significant increase was reported (9.25±4.5x10^9/L on day 1 and 11.79±7.9x10^9/L on day 7, p<0.01). A similar pattern was seen in the mean urea levels: a tendency to decrease in the SG (7.41±3.4 mmol/L on day 1 and 7.32±2.9 mmol/L on day 7, p>0.05) and a statistically significant rise in the CG (8.06±5.6 mmol/L on day 1 and 9.34±7.7 mmol/L on day 7, p<0.05).
Mean platelet values increased significantly in patients in SG (241.58±91.1x10^9/L on day 1 and 284.21±101.0x10^9/L on day 7, p<0.01) and in patients in CG (219.84±80.0x10^9/L on day 1 and 276.48±112.3x10^9/L on day 7, p<0.001). D-dimer levels also showed a statistically significant increase in both groups: in the MG (0.98±0.8 µg/mL on day 1 and 2.58±2.9 µg/mL on day 7, p<0.01) and in the CG (1.98±2.5 µg/mL on day 1 and 2.97±2.9 µg/mL on day 7, p<0.05).
Fibrinogen plays a crucial role in blood coagulation and is also considered an indicator of the severity of inflammation. Data analysis showed that in ozone -treated patients, fibrinogen levels decreased significantly by day 7, with values of 3.6 (IQR 2.7-4.2) g/L compared to 4.3 (IQR 3.9-4.8) g/L at the time of enrollment (p<0.001). In contrast, no significant change in plasma fibrinogen concentration was observed in the control group, with levels of 4.6 (IQR 3.6-4.7) g/L on day 7 and 4.4 (IQR 3.9-4.6) g/L on day 1 (p>0.05). On day 7, the mean fibrinogen value was significantly lower in the ozone treatment group: 3.8 (IQR 2.7-4.2) g/L compared to 4.0 (IQR 3.6-4.7) g/L in the control group (p<0.05). Additionally, the median absolute difference between initial and final fibrinogen concentrations was significantly greater in the ozone-treated group: 0.55 (IQR 0.07-1.52) g/L compared to 0.25 (IQR -0.7-0.7) g/L in the control group (p<0.05).
These findings are consistent with a case-control study showing a significant reduction in fibrinogen levels in patients with COVID-19 and severe bilateral pneumonia (n=14) who received both conventional treatment and ozone therapy (713±112 mg/dL and 572±163 mg/dL, respectively; p<0.05). In contrast, patients treated with only conventional methods had fibrinogen levels of 602±160 mg/dL and 528±149 mg/dL, respectively (p>0.05) [20].
The study's strengths include its prospective and randomized design. Nevertheless, several limitations should be mentioned: a) the small sample size, b) the relatively short follow-up duration, c) inclusion of only patients not requiring mechanical ventilation, d) the study was conducted at a single healthcare center, e) it was not a blinded study in terms of treatment provided, f) a slightly younger age of the main study group undergoing ozone autohemotherapy, and g) the inability to calculate patients' BMI due to pandemic conditions.
Thus, the evidence from specialized literature and the current study results indicate that ozone therapy has clinical benefits for COVID-19 patients. Ozone therapy shows promise as an adjunctive treatment for those infected with SARS-CoV-2. The mechanisms of action of ozone therapy support its combined use with other treatments. Additionally, multiple clinical studies have also reported positive outcomes. Systemic oxygen-ozone therapy is particularly important at the disease's onset and before the condition worsens to the point of requiring mechanical ventilation. It also helps modulate laboratory biomarkers, which are crucial for assessing risk and prognosis in COVID-19 patients.
The lack of statistically significant differences in the current study parameters may be due to the small sample size and the study's unicentric design.
Conclusions
Ozone therapy restrains the progression of the SARS-CoV-2 infection and its complications, promotes the recovery of the clinical condition due to its several beneficial properties such as immunomodulatory, antioxidant, anti-inflammatory, and cytoprotective effects. Our study demonstrated that the mortality rate among COVID-19 patients treated with ozone in the ICU was lower compared to those receiving conventional treatment. The impact of ozone therapy on oxygen metabolism resulted in a statistically significant increase in the mean oxygenation index by reactivating the intracellular and extracellular antioxidant systems, effectively countering long-term oxidative stress in various inflammatory and degenerative processes. If administered early in the course of the disease, ozone therapy can prevent the progression to ARDS and help alleviate the severe effects of COVID-19 on lung tissues. Ozone therapy improves blood flow, facilitates oxygen transport in hypoxemic tissues, and reduces blood clotting phenomena in COVID-19 patients. So, under this therapy, COVID-19 patients showed improved blood circulation and oxygen delivery to ischemic tissue and optimized overall metabolism leading to a trend toward milder ARDS.
Our research study showed a decreasing trend in use of oxygen therapy, non-invasive ventilation, and invasive mechanical ventilation with ozone therapy, specifically major ozonized autohemotherapy in COVID-19 patients. Despite encouraging preliminary data from ongoing clinical trials, as well as expert opinion, there is still insufficient evidence to confirm that ozone therapy is a viabletreatment option for patients with COVID-19
Competing interests
None declared.
Authors’ contributions
NC and RB conceived the study, participated in the study design and assisted in drafting the manuscript. NC data interpretation. IC drafted the manuscript. ICh and SȘ conceived the significant revision of the manuscript and provided significant intellectual involvement. The authors have read and approved the final version of the manuscript.
Acknowledgements and funding
The study had no external funding.
Patient consent
Obtained.
Ethics approval
The study protocol was approved by the Research Ethics Committee of Nicolae Testemițanu State University of Medicine and Pharmacy (minutes No.1, from 20.07.2020).
Authors’ ORCID IDs
Cernei Natalia – https://orcid.org/0000-0002-2031-5881
Serghei Șandru – https://orcid.org/0000-0002-2973-9154
Ivan Cîvîrjîc – https://orcid.org/0000-0002-1360-5485
Ion Chesov – https://orcid.org/0000-0001-5083-4757
Ruslan Baltaga – https://orcid.org/0000-0003-0659-4877
References
Arias-Vázquez P, Arcila-Novelo R, Ramírez-Wakamatzu M. Is Ozone therapy an adjunct treatment for SARS-CoV-2 / COVID-19 infection? Braz J Pharm Sci. 2022;58:e20775. http://dx.doi.org/10.1590/s2175-97902022e20775.
Viebahn-Hänsler R, Fernández O, Fahmy Z. Ozone in medicine: clinical evaluation and evidence classification of the systemic Ozone applications, major autohemotherapy and rectal insufflation, according to the requirements for evidence-based medicine. Ozone Sci Eng. 2016;38(5):322-345. https://doi.org/10.1080/01919512.2016.1191992.
Barbosa R, Santo R, Navegante Z, Santos S, Rivera J, Gomes A. Ozone therapy as a treatment option against COVID-19: a literature review. Res Soc Devel. 2021;10(13):e469101321228. https://doi.org/10.33448/rsd-v10i13.21228.
Hernández A, Viñals M, Isidoro T, Vilás F. Potential role of Oxygen-Ozone therapy in treatment of COVID-19 pneumonia. Am J Case Rep. 2020;21:e925849. doi: 10.12659/AJCR.925849
International Scientific Committee of Ozone Therapy (ISCO3); Schwartz A, Martínez-Sánchez G. Potential use of ozone in SARS-CoV-2 / COVID-19 [Internet]. Madrid: ISCO3; 2020 [cited 2022 Sep 23]. Available from: https://docs.bvsalud.org/biblioref/2020/04/1095104/potential-use-of-ozo….
Harapan B, Harapan T. The role of ozone therapy in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and coronavirus disease 2019 (COVID-19): a review. Med Gas Res. 2023;13(4):165-171. doi: 10.4103/2045-9912.369237.
Ministerul Sănătății al Republicii Moldova [Ministry of Health of the Republic of Moldova]. Infecția cu coronavirus de tip nou (COVID-19): Protocol clinic național provizoriu (PCN-371) [Novel coronavirus infection (COVID-19): National clinical protocol]. 3rd ed. Chisinau: The Ministry; 2020. 65 p. Romanian.
Ministerul Sănătății al Republicii Moldova [Ministry of Health of the Republic of Moldova]. Infecția cu coronavirus de tip nou (COVID-19): Protocol clinic național provizoriu (PCN-371) [Novel coronavirus infection (COVID-19): National clinical protocol]. 4th ed. Chisinau: The Ministry; 2020. 78 p. Romanian.
Ministerul Sănătății al Republicii Moldova [Ministry of Health of the Republic of Moldova]; Cojocaru V, Holban T, Cusnir O, et al. Managementul complicațiilor severe cauzate de infecția provocată de coronavirus (COVID-19): Ghid practic [Management of severe complications caused by the coronavirus infection (COVID-19): Practical guide]. Chișinău; The Ministry; 2020. 67 p. Romanian.
Çolak Ş, Genç Yavuz B, Yavuz M, Özçelik B, Öner M, Özgültekin A, et al. Effectiveness of ozone therapy in addition to conventional treatment on mortality in patients with COVID-19. Int J Clin Pract. 2021;75(8):e14321. doi: 10.1111/ijcp.14321.
Hernández A, Viñals M, Pablos A, Vilás F, Papadakos P, Wijeysundera D, et al. Ozone therapy for patients with COVID-19 pneumonia: preliminary report of a prospective case-control study. Int Immunopharmacol. 2021;90:107261. doi: 10.1016/j.intimp.2020.107261.
Gudumac V, Tagadiuc O, Rîvneac V, Sardari V, PanteaV, Andronache L, et al. Investigaţii biochimice. Vol. 2: Micrometode [Biochemical investigations. Vol. 2: Micromethods]. Chișinău: Elena VI; 2010. 97 p. ISBN 978-9975-106-06-1. Romanian.
Fogante M, Cavagna E, Rinaldi G. Chest X-ray scoring system in COVID-19 pneumonia: an added value in the evaluation of the disease severity. Eurasian J Med Oncol. 2021;5(4):305-310. doi: 10.14744/ejmo.2021.70171.
Tascini C, Sermann G, Pagotto A, Sozio E, De Carlo C, Giacinta A, et al. Blood ozonization in patients with mild to moderate COVID-19 pneumonia: a single centre experience. Intern Emerg Med. 2021;16(3):669-675. doi: 10.1007/s11739-020-02542-6.
Shah M, Captain J, Vaidya V, Kulkarni A, Valsangkar K, Nair P, et al. Safety and efficacy of ozone therapy in mild to moderate COVID-19 patients: a phase 1/11 randomized control trial (SEOT study). Int Immunopharmacol. 2021;91:107301. doi: 10.1016/j.intimp.2020.107301.
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574-1581. doi: 10.1001/jama.2020.5394.
Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect. 2020;80(6):656-665. doi: 10.1016/j.jinf.2020.03.041.
Hernandez A, Viñals M, Pablos A, Vilás F, Papadakos P, Wijeysundera D, et al. Ozone therapy for patients with SARS-COV-2 pneumonia: a single-center prospective cohort study. Insights Biomed. 2020;5(4):13. doi: 10.36648/2572-5610.4.4.75.
Zhang L, Yan X, Fan Q, Liu H, Liu X, Liu Z, et al. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J Thromb Haemost. 2020;18(6):1324-1329.
doi: 10.1111/jth.14859.Fernández-Cuadros M, Albaladejo-Florín M, Álava-Rabasa S, Gallego-Galiana J, Pérez-Cruz G, Usandizaga-Elio I, et al. Compassionate use of rectal Ozone (O3) in severe COVID-19 pneumonia: a case-control study. SN Compr Clin Med. 2021;3(5):1185-1199.
doi: 10.1007/s42399-021-00849-9.