Introduction
The mandibular third molar is the most frequent impacted permanent tooth [1]. Various studies show a prevalence of 9.5 to 39% of third mandibular molars that fail to erupt into the oral cavity [2]. Mandibular molar impactions are usually mesioangular, distoangular, vertical, and horizontal. The position and type of impaction may affect the development of pericoronitis [3]. Pericoronitis is an inflammatory and infectious condition that usually affects an incompletely erupted mandibular third molar. The localized inflammation may range from major regional reactions, such as cellulitis, trismus, pain, and bleeding, to general reactions, such as fever and asthenia [4]. Studies show that pericoronitis is the most common acute problem associated with third molars, and there are several predisposing factors related to the etiology of the disease. One of them is the position of impaction; thus, understanding the relationship between the occurrence of pericoronitis and the clinical and radiographic conditions of the lower third molars is the key for the determination of the clinical behavior of these teeth [5]. The status of impaction can be judged radiographically on orthopantomography and cone beam computed tomography (CBCT). This kind of investigation provides information on assessing the position and status of the tooth. The aim of this study is to determine the most common positions of impaction of the lower wisdom teeth as a risk factor for pericoronitis.
Materials and methods
The present study was conducted in the department of Oro-Maxillo-Facial Surgery and Oral Implantology „Arsenie Guțan” and involved 120 (66 women and 54 men) patients with an age range of 17 – 46 years (mean 27 ± SD 6), who came for dental surgical treatment during 2017–2022.
The study was approved by the Ethics Committee of the Nicolae Testemițanu State University of Medicine and Pharmacy, No.82 from 26.04.2017 and informed consents were obtained from all subjects involved in the study.
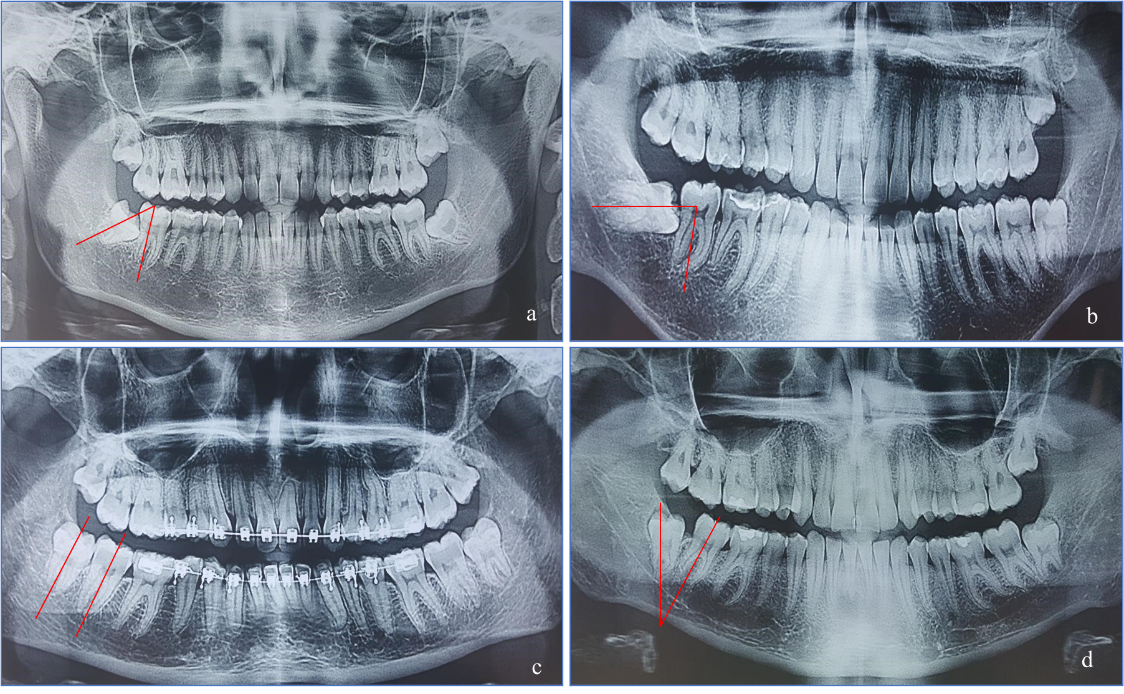
Patients with partially erupted third molars and radiographic evidence of impaction were included in the study. Clinical conditions such as redness, pus or exudate, pain, trismus, and sensitivity over the pericoronal flap have been evaluated. During the radiological examination, all participants were subjected to CBCT in all three planes scan, operating at 120 kVp, 15 mA, and 18s, and Ortopantomography scan operating at 120 kVp, 15 mA, and 18s, taken with a Planmeca machine. To classify the third molar position of impaction, we used the Winter classification (Figure 1). Reported to the second molar axis, we classified it into vertical (10°), mesioangular (+11°–70°), distoangular (−11°–70°), and horizontal (>70°) positions. All obtained images were read by three independent doctors to increase the accuracy of the study.
|
Fig. 1 Third molar impaction by Winter classification (OPG). (a) – mesio-angular impaction, (b) – horizontal impaction, (c) – vertical impaction, (d) – disto-angular impaction. |
Obtained results were subjected to statistical analysis using the SPSS statistical software (IBM SPSS) version 26.0. Independent t‑test and Chi‑square test were used to determine the significant association between the two variables. P value < 0.05 was considered significant.
Results
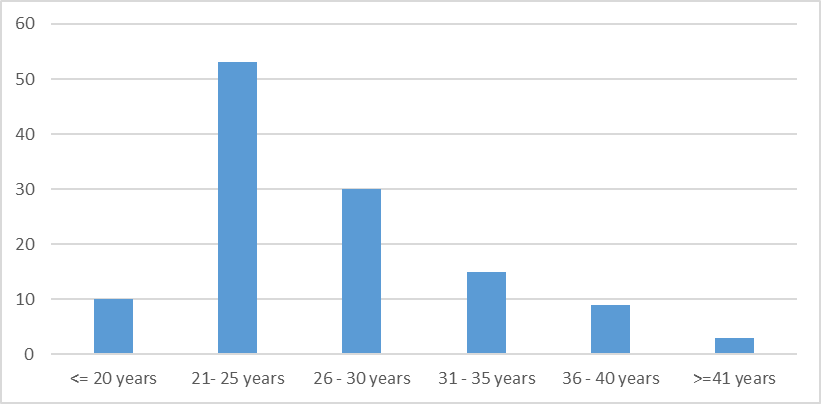
Table 1 shows that in our study we involved 120 patients (66 women and 54 men) with an age range of 17 – 46 years (mean 27 ± SD 6). Table 1 shows that the maximum number of cases of pericoronitis was observed in the age group 21–25 years (53 patients), followed by 26 – 30 years in 30 cases, and 31 – 35 years in 15 cases. The result was statistically significant at P < 0.05
Table 1. Classification of patients by age group. | |||
Age, groups | <= 20 years | Total | 10 |
Column N % | 8,3% | ||
95.0% Lower CL for Column N % | 4.4% | ||
95.0% Upper CL for Column N % | 14.3% | ||
21 – 25 years | Total | 53 | |
Column N % | 44.2% | ||
95.0% Lower CL for Column N % | 35.5% | ||
95.0% Upper CL for Column N % | 53.1% | ||
26 – 30 years | Total | 30 | |
Column N % | 25.0% | ||
95.0% Lower CL for Column N % | 17.9% | ||
95.0% Upper CL for Column N % | 33.3% | ||
31 – 35 years | Total | 15 | |
Column N % | 12.5% | ||
95.0% Lower CL for Column N % | 7.5% | ||
95.0% Upper CL for Column N % | 19.3% | ||
36 – 40 years | Total | 9 | |
Column N % | 7.5% | ||
95.0% Lower CL for Column N % | 3.8% | ||
95.0% Upper CL for Column N % | 13.2% | ||
>=41 years | Total | 3 | |
Column N % | 2.5% | ||
95.0% Lower CL for Column N % | 0.7% | ||
95.0% Upper CL for Column N % | 6.5% | ||
Note: CL – confidence limit; N – number; Upper 95% confidence limit (CL) – sample mean + (1.96); Lower 95% CL – sample mean – (1.96). | |||
|
Fig. 2 Categories of patients by age group. |
As shown in table 2, there is a significant statistic difference between obtained distribution and the theoretic one (uniform).
Table 2. One-Sample Chi-Square Test Summary. | |
Total N | 120 |
Test Statistic | 86.200a |
Degree Of Freedom | 5 |
Asymptotic Sig. (2-sided test) | .000 |
Note: There are 0 cells (0%) with expected values less than 5. The minimum expected value is 20. | |
Based on the results of our study, the biggest number of cases of pericoronitis was observed in the vertical position (92 cases) by Winter, followed by the mesioangular position (24 cases) and the distoangular position (4 cases), as shown in table 3. In the study, we did not detect any patients with a horizontal position.
Table 3. Wisdom tooth position by Winter classification. | |||
Tooth position by Winter classification | Vertical | Total | 92 |
Column N % | 76.7% | ||
95.0% Lower CL for Column N % | 68.5% | ||
95.0% Upper CL for Column N % | 83.5% | ||
Mesioangular | Total | 24 | |
Column N % | 20.0% | ||
95.0% Lower CL for Column N % | 13.6% | ||
95.0% Upper CL for Column N % | 27.8% | ||
Distoangular | Total | 4 | |
Column N % | 3.3% | ||
95.0% Lower CL for Column N % | 1.1% | ||
95.0% Upper CL for Column N % | 7.7% | ||
Horizontal | Total | 0 | |
Column N % | 0.0% | ||
95.0% Lower CL for Column N % | . | ||
95.0% Upper CL for Column N % | . | ||
Note: CL – confidence limit; N – number; Upper 95% confidence limit (CL) – sample mean + (1.96); Lower 95% CL – sample mean – (1.96). | |||
According to the classification by Pell and Gregory shown in Table 4, most cases belonged to Class I (73 cases). Third molars classified in position A (92 cases) had a greater chance of pericoronitis when compared to those in position B (24 cases) or C (4 cases).
Table 4. Wisdom tooth position by Pell&Gregory classification. | |||
Tooth position by Pell&Gregory classification | I | Total | 73 |
Column N % | 60.8% | ||
95.0% Lower CL for Column N % | 51.9% | ||
95.0% Upper CL for Column N % | 69.2% | ||
II | Total | 42 | |
Column N % | 35.0% | ||
95.0% Lower CL for Column N % | 26.9% | ||
95.0% Upper CL for Column N % | 43.8% | ||
III | Total | 5 | |
Column N % | 4.2% | ||
95.0% Lower CL for Column N % | 1.6% | ||
95.0% Upper CL for Column N % | 8.9% | ||
Tooth position by Pell&Gregory classification | A | Total | 92 |
Column N % | 76.7% | ||
95.0% Lower CL for Column N % | 68.5% | ||
95.0% Upper CL for Column N % | 83.5% | ||
B | Total | 24 | |
Column N % | 20.0% | ||
95.0% Lower CL for Column N % | 13.6% | ||
95.0% Upper CL for Column N % | 27.8% | ||
C | Total | 4 | |
Column N % | 3.3% | ||
95.0% Lower CL for Column N % | 1.1% | ||
95.0% Upper CL for Column N % | 7.7% | ||
Note: CL – confidence limit; N – number; Upper 95% confidence limit (CL) – sample mean + (1.96); Lower 95% CL – sample mean – (1.96). | |||
Discussions
Pericoronitis is an inflammation that occurs in the soft tissues around an erupting tooth. Due to the fact that pericoronitis is particularly related to the complications caused by the eruption of teeth, the third molars, especially the lower ones, are particularly more affected, since they present more limitations and difficulties in the complete eruption, mainly due to lack of space and bad dental positioning [5].
Patients with pericoronitis experience pain, discomfort, swelling, pus discharge, lymphadenopathy, dysphagia, systemic disorders, and serious complications [6].
Clinical studies suggested that the microbiota predominantly responsible for pericoronitis is mainly anaerobic and contains Campylobacter species, Capnocytophaga species, Fusobacterium species, Micromonas (Peptostreptococcus) micros, Prevotella intermedia, Prevotella nigrescens, and Veillonella species. Streptococci, staphylococci, actinomycetes, and enterobacteria, as well as protozoa and fungi, have also been described [7].
Based on the results of our study, we can affirm that pericoronitis is more frequently encountered in females as compared to males; this can be explained by the multiple theories from the specialized literature, such that as female`s jaws stop growing when the third molars just begin to erupt, in contrast to males, in whom the growth of the jaws continues beyond the time of the eruption of the third molars [8]. Our study shows that maximum number of cases of pericoronitis was observed in the age group 21–25 years (53 patients), followed by 26–30 years in 30 cases, and 31–35 years in 15 cases. These results are very similar to those of the studies by Shin et al. [9] that found that the age group 20–29 years exhibited a maximum number of pathoses associated with a lower third molar and long‑term exposure to irritants from the oral cavity. The present study showed that the biggest number of cases of pericoronitis were observed in the vertical position according to Winter. Similar results were noticed in the study conducted by Galvão et al., and McArdle et al, which concluded that a vertically impacted molar is commonly associated with pericoronitis [5, 10]. According to the classification of Pell&Gregory, there is a greater chance of pericoronitis in the position A, in contrast to the results by Galvão et al., who observed that pericoronitis is common in B position. The common symptoms such as swelling, trismus, pain, and difficulty in swallowing, were mostly seen in patients.
Conclusions
Mandibular third molar impaction is a common pathology encountered in young age groups. Dividing the patients into 6 age groups, the maximum number of cases of pericoronitis was observed in the age group 21–25 years, followed by 26–30 years. According to Pell&Gregory’s classification, the most common impaction position in pericoronitis occurrence is vertical, followed by the mesioangular position. According to another classification by Pell and Gregory, most cases belonged to class I, position A.
Competing interests
None declared
Financial disclosure statement
The research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author’s ORCID ID
Gabriela Motelica - https://orcid.org/0000-0003-1694-2038
References
Singh R., Devanna R., Tenglikar P., Gautam A., Anubhuti., Kumari P. Evaluation of mandibular third molar position as a risk factor for pericoronitis: A CBCT study. J. Family Med. Prim. Care., 2020 Mar 26; 9 (3): 1599-1602.
Ramamurthy A., Pradha J., Jeeva S., Jeddy N., Sunitha J., Kumar S. Prevalence of mandibular third molar impaction and agenesis: A radiographic south Indian study. J. Indian Acad. Oral Med. Radiol., 2012; 24: 7.
Tsvetanov T. Association of the mandibular third molar position to the pericoronitis. Int. J. Med. Res. Health Sci., 2018; 7: 35-40.
Wehr C., Cruz G., Young S., Fakhouri W. An Insight into Acute Pericoronitis and the Need for an Evidence-Based Standard of Care. Dent. J. (Basel), 2019 Sep 2; 7 (3): 88.
Galvão E., da Silveira E. et al. Association between mandibular third molar position and the occurrence of pericoronitis: A systematic review and meta-analysis. Arch. Oral Biol., 2019 Nov; 107: 104486.
Al-Dajani M., Abouonq A., Almohammadi T., Alruwaili M., Alswilem R., Alzoubi I. A cohort study of the patterns of third molar impaction in panoramic radiographs in saudi population. Open Dent. J. 2017; 11: 64860.
Katsarou T., Kapsalas A., Souliou C., Stefaniotis T., Kalyvas D. Pericoronitis: A clinical and epidemiological study in greek military recruits. J. Clin. Exp. Dent. 2019 Feb 1; 11(2): e133-e137.
Schalch T., Martimbianco A., Gonçalves M., Motta L., Santos E., Cecatto R., Bussadori S., Horliana A. Interventions for Early-Stage Pericoronitis: Systematic Review of Randomized Clinical Trials. Antibiotics (Basel), 2022 Jan 8; 11 (1): 71.
Shin S., Choi E., Moon S. Prevalence of pathologies related to impacted mandibular third molars. Springer plus 2016; 5: 915.
McArdle L.W., Andiappan M., Khan I., Jones J., McDonald F. Diseases associated with mandibular third molar teeth. Br. Dent. J., 2018 Mar 23; 224 (6): 434-440.