Introduction
Cerebrovascular pathology is one of the main causes of morbidity, mortality, and disability, both at a global and national level in the Republic of Moldova. In the Republic of Moldova, there were 77748 patients with cerebrovascular pathologies in 2020 vs. 79691 in 2019, according to the National Public Health Agency data published, with cerebrovascular pathologies having a prevalence of 270.7 in 2020 vs. 277.4 in 2019 per 10,000 people. The incidence of cerebrovascular pathologies was 5523 in 2020 and 7320 in 2019, which represents 19.2 in 2020 vs. 25.5 in 2019 per 10,000 people.
Clinical registries play an important role in the health services assessment and, indirectly, determine their improvement. Since 2016, Moldova is part of the ESO-EAST project (European Stroke Organization Enhancing and Accelerating Stroke Treatment) of the European Stroke Organization [1-5]. ESO EAST aims to improve the quality of stroke care in the population of Eastern European countries, which is delivered from the admission of a patient through his or her discharge from that hospital, as in Eastern European countries the incidence and prevalence of this disease are impressive and constantly progressing. Continuous monitoring of stroke care quality allows hospital-to-hospital and country-to-country benchmarking and identification of the gaps and needs in health care. The quality of stroke care relates to imaging, acute care, and prevention of complications, secondary prevention, and rehabilitation. Therefore, the main objective of the Registry of Stroke Care Quality (RES-Q) project is to improve the quality of healthcare provided to stroke patients by translating the data collected by RES-Q into effective health policies at the national and international level by collecting data over a period of one month or several years consecutively [5-8].
The Institute of Emergency Medicine from Chisinau joined the registry in 2017 and has enrolled 489 patients.
Our aim was to investigate whether in-hospital quality indicators in stroke patients changed between 2017 – 2022.
Materials and methods
A retrospective analysis of all consecutive acute stroke patients from the Institute of Emergency Medicine of Chisinau, Republic of Moldova, was performed. We have analyzed the data introduced in the RES-Q registry between March 1 and March 31, 2022, and compared it with the same period for 2017, 2018, 2019, 2020, and 2021.
A wide range of factors were recorded in the RES-Q registry, including patient characteristics and care received in hospital. The factors investigated in the study included: sociodemographic, such as age and sex; health behaviors and comorbidities, such as presence of atrial fibrillation (AF) and smoking status; stroke-related factors, such as stroke severity assessed by the National Institutes of Health Stroke Scale (NIHSS); stroke type; in-hospital stroke; time from stroke onset to hospital arrival, and door-to-needle time for intravenous thrombolysis; discharge information, such as length of hospital stay and discharge destination; and evidence-based processes of care provided while in hospital.
The data collection in our country is performed as part of routine clinical practice and quality assurance and therefore does not require special approval from local ethical committees. The protocol of this study is approved by the Ethical Committee of St. Anne's University Hospital, Czech Republic.
Results
The Institute of Emergency Medicine from Chisinau joined the registry in 2017 and has enrolled 489 patients. The COVID-19 pandemic has left its mark on the number of stroke hospitalizations, a fact observed in all countries of the world, including the Republic of Moldova, as evidenced by the data of the RES-Q registry (tab. 1) [9-13].
Patient Characteristics
In 2021, there were more hospitalized men (58.3% in 2021 vs. 48.65% in 2018), more patients with ischemic stroke (86.67% in 2021 vs. 60.78% in 2019). No age (68 years) difference was noted (tab. 1). More than one fourth of the patients (tab. 1) were current smokers, and the proportion was four times greater in men compared to women.
The presence of atrial fibrillation (patients known to have AF) for ischemic stroke and TIA was found in 35.5% of patients in 2022, compared to 50% in 2020 (tab. 1). AF was detected during hospitalization for ischemic stroke and TIA in 6.5% of patients in 2022 vs. 5.77% in 2020 by electrocardiogram (ECG).
Stroke Severity and Stroke Type
At admission, the median National Institute of Health Stroke Scale score indicating stroke severity was between 7 in 2017 and 12 points in 2021 Tab. 1).
There were 21.25% – 35.9% of cases presenting with a loss of consciousness (drowsy or comatose) at admission. The majority of patients were found to have ischemic stroke (60.78% – 91.14%), followed by intracerebral hemorrhage (7.6 – 13.33%), while only a very small proportion had subarachnoid hemorrhage (1.27% – 2.1%).
Table 1. Characteristic of RES-Q Registrants for Stroke in the Institute of Emergency Medicine for one month (March), 5 years consecutively (2017 – 2022). | ||||||
Year | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
Number of cases | 79 | 111 | 102 | 60 | 60 | 71 |
Sociodemographic | ||||||
Age in years, median | 69 | 69 | 68 | 69 | 66 | 67 |
Prestroke health | ||||||
Current smoker (%) | 20.31 | 23.28 | 12.64 | 10.86 | 20.2 | 18.3 |
The presence of AF (known AF) for ischemic stroke and TIA (%) | 36.11 | 26.96 | 23.46 | 50 | 23.08 | 29 |
Detected during hospitalization for ischemic stroke and TIA (%) | 4.17 | 4.35 | 4.95 | 5.77 | 3.85 | 6.5 |
Newly detected at admission (%) | – | 2 | 3.7 | – | – | – |
Stroke-related factors | ||||||
Stroke severity |
|
|
|
|
| |
NIHSS median | 7 | 7 | 11 | 9 | 12 | 8 |
Loss of consciousness (drowsy/comatose) (%) | 35.9 | 25.9 | 21.25 | 32.7 | 21.67 | 25.7 |
Type of stroke | ||||||
Ischemic stroke (%) | 91.14 | 78.38 | 60.78 | 83.33 | 86.67 | 84.5 |
Intracerebral hemorrhagic (%) | 7.6 | 12.61 | 17.65 | 13.33 | 13.33 | 9.9 |
Subarachnoid hemorrhagic (%) | 1.27 | 2.1 | 1.8 | 0 | 0 | 0 |
Note: AF – atrial fibrillation; TIA – transient ischemic attack; NIHSS – National Institutes of Health Stroke Scale or NIH Stroke Scale/Score. | ||||||
Processes of Care
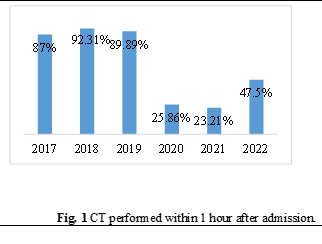
Almost all hospitalized patients with stroke received neuroimaging, so between 2017 – 2022 the percentage of brain CT scans did not change much (100% in 2022, 93.3% in 2021, 96.7% in 2020, 90% in 2019, 97.2% in 2018, and 98.72% in 2017), but a significant decrease in CT performed in the first hour after admission was noted (23.21% in 2021, 25.86% in 2020, vs 92.31% in 2018) (Fig. 1).
Among those with ischemic stroke, more than a half of patients received carotid investigation ≤7 days after hospital admission. Carotid artery imaging was less performed in the pandemic period (77.4% in 2022 and 65.38% in 2021 vs. 87.5% in 2017) (Fig. 2, Tab. 2).
Carotid endarterectomy or angioplasty/stenting was done or planned for patients with ischemic stroke with internal carotid artery stenosis >50% among 33.33% of the patients with ischemic stroke eligible for the procedures in 2021 vs. 16.67% in 2019 (Tab. 2).
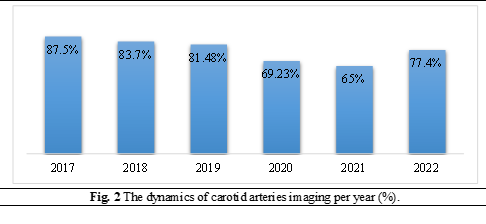
Table 2. Processes of care of RES-Q Registrants. | ||||||
| Year | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
| Neuroimaging (%) | 98.72 | 97.2 | 90 | 96.7 | 93.3 | 100 |
| CT performed in the first hour after admission (%) | 87.01 | 92.31 | 89.89 | 25.86 | 23.21 | 47.5 |
| Carotid investigation ≤7 days after hospital admission for ischemic stroke (%) | 87.5 | 83.7 | 81.48 | 69.23 | 65 | 77.4 |
| Carotid endarterectomy or angioplasty/stenting done or planned for carotid stenosis >50% (%) | 66.67 | 66.67 | 16.67 | 0 | 33.33 | – |
| Intravenous thrombolysis (%) | 2.78 | 4.6 | 11.29 | 10 | 7.69 | 20 |
| Endovascular treatment (%) | – | – | 3.23 | – | 5.77 | 10 |
| Time to needle (minutes) (%) | 85 | 93.5 | 53 | 25 | 48 | 51.5 |
| Patients put on ventilator (%) | unknown | 18.56 | 16.88 | 19.57 | 30.51 | 16.7 |
| Assessment for rehabilitation needs ≤72 hours after hospital admission (%) | 86.62 | 91.3 | 61.84 | 63.16 | 55 | 90.9 |
| Dysphagia screening (%) | 37.74 | 77.13 | 58 | 78.9 | 48.34 | 82.1 |
| Antihypertensive agent (%) | 98.44 | 97.8 | 92.86 | 95.56 | 89.47 | 96.9 |
| Cholesterol-lowering medication (%) | 58.33 | 56.99 | 44.44 | 44.23 | 59.09 | 60 |
| Prescribed antiplatelets to patients without AF (%) | 100 | 100 | 81.63 | 100 | 92 | 88.9 |
| Anticoagulants in AF (%) | 70.83 | 100 | 35.71 | 71.43 | 100 | 55 |
Note: AF – atrial fibrillation; CT – computed tomography scan. | ||||||
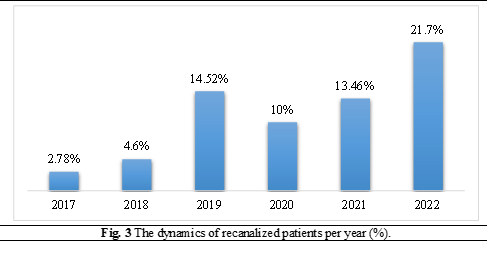
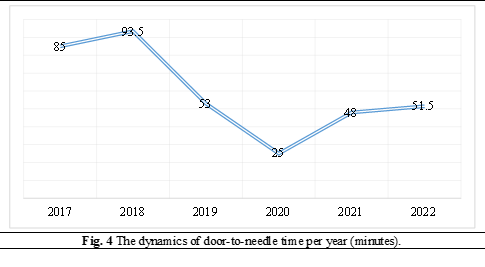
The number of recanalized patients was not affected by COVID-19 pandemic (21.7% in 2022, 13.46% in 2021 and 10% in 2020 vs. 14.62% in 2019, 4.6% in 2018 and 2.78% in 2017) (Fig. 3). The proportion of patients with ischemic strokes receiving thrombolysis therapy has substantially increased from 2.78% in 2017 to 20% in 2022, and the median door-to-needle time decreased from 85 minutes (2017) to 48 minutes (2021) (Fig. 4). Thrombectomy began to be performed in 2018 at the Institute of Emergency Medicine, the proportion of patients with ischemic strokes receiving thrombectomy increased from 3.23% in 2019 to 10.0% in 2022, and the median door-to-groin time decreased from 228.5 minutes in 2019 to 102 minutes in 2021.
All these data demonstrate the effort to improve the quality of stroke care at this hospital.
Approximately two-thirds of the participants in 2021 and 90.9% in 2022 had assessments for rehabilitation needs ≤72 hours after hospital admission. Almost a third of patients (37.74%) in 2017, three quarters of patients (78.9%) in 2020 and in 2022 (82.1%) with stroke received dysphagia assessment or screening. In general, more than 80% of patients received secondary prevention therapies that were level-1 evidence-based processes of care: antihypertensive agents (89.47% – 98.44%), antiplatelet drugs (81.63% – 100%), anticoagulants for patients with atrial fibrillation (70.83% in 2017 vs. 100% in 2021), but cholesterol-lowering medication was prescribed to approximately a half of the participants (44.23% – 60.0%). There were no differences between men and women in the care received (Tab. 2).
In the pandemic period, there were more patients put on ventilator: 19.57% in 2020, 30.51% in 2021, vs. 18.56% in 2018 and 16.88% in 2019 (Tab. 2).
There were more deaths in the pandemic years (36.67% in 2021, 23.33% in 2020, vs. 14.71% in 2019) (Tab. 3, Fig. 5).
Table 3. Discharge destination. | ||||||
Home (%) | 67.09 | 80.18 | 80.39 | 68.33 | 51.67 | 78.3 |
Rehabilitation facility (%) | 13.92 | 3.6 | 4.9 | 8.34 | 8.33 | 9.1 |
Other hospital (%) | 0 | 0 | 0 | 0 | 3.33 | 0.2 |
Died (%) | 18.99 | 16.22 | 14.71 | 23.33 | 36.67 | 12.4 |
Median hospital stay | 9 | 10 | 10 | 8 | 8 | 10 |
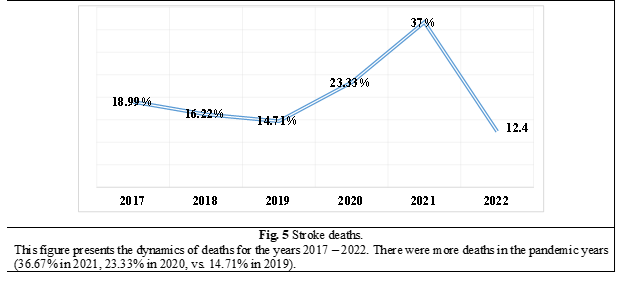
An important part of centralized stroke care is also rehabilitation (during the acute disease phase as well as long-term rehabilitation). In 2021, 55% of patients benefited from rehabilitation measures during inpatient treatment, with the majority of stroke patients being subsequently discharged at home (51.67%), only 8.33% of patients being transferred for rehabilitation purposes to another center, and 36.67% died (Tab. 2). So, in 2020 – 2021 the pandemic had a predominantly negative impact on the diagnostic process and on the evolution of stroke, but an improvement in the quality of stroke management during the 2022 year is remarkable: 90.9% of patients benefited from rehabilitation measures, with the majority of stroke patients being subsequently discharged at home (78.3%), only 9.1% of patients being transferred for rehabilitation purposes to another center, and 12.4% died (Tab. 3).
Discussion
The number of recanalized patients was not affected by COVID-19 pandemic (21.7% in 2022, 13.46% in 2021 and 10% in 2020 vs. 14.62% in 2019, 4.6% in 2018 and 2.78% in 2017). The proportion of patients with ischemic strokes receiving thrombolysis therapy has substantially increased from 2.78% in 2017 to 20% in 2022, and the median door-to-needle time decreased from 85 minutes (2017) to 48 minutes (2021).
Thrombectomy began to be performed in 2018 at the Institute of Emergency Medicine; the proportion of patients with ischemic strokes receiving thrombectomy increased from 3.23% in 2019 to 10.0% in 2022; the median door-to-groin time decreased from 228.5 minutes in 2019 to 102 minutes in 2021, demonstrating the effort to improve the quality of stroke care at this hospital.
The considerable delay in time from stroke onset to hospital arrival remains an important issue. More than 70% of those with stroke admitted to our hospital did not arrive ≤4.5 hours after experiencing stroke symptoms, and therefore they were potentially ineligible for intravenous thrombolysis therapy. The median door-to-needle time at the hospital, which has decreased to 48 minutes in 2021 and 51.5 minutes in 2022, has met the American Heart Association/American Stroke Association’s initial goal (≤60 minutes for at least 50% of acute ischemic strokes patients) [14, 15].
Some aspects of care, such as assessment for dysphagia screening, AF screening, rehabilitation needs, and carotid investigation, appeared to be less than optimal. The reasons for the lack of assessment for dysphagia screening, AF screening, rehabilitation needs and carotid investigation after hospital admission included the patients’ condition, which did not allow for assessment, as well as lack of personnel and equipment, such as Holter ECG for AF screening. Between 2017 and 2022, AF was detected during hospitalization for ischemic stroke and TIA in 3.85% – 6.5% patients by electrocardiogram. Holter ECG is an important tool for detecting cardioembolic strokes and for optimal secondary prevention. It is recommended for all ischemic strokes where the etiology is not clearly identified. One of the indicators of the RES-Q database is the percentage of the Holter ECG indication for those types of ischemic stroke.
The data collection of indicators of stroke care quality brings feedback to each stroke center and controls its activity and results. The determination of the type of an ischemic stroke is important, especially for secondary prevention [16]. This is related to the implementation of ECG Holter monitoring for ischemic strokes. The detection of swallowing disorder is also important for the prevention and treatment of subsequent complications as well as for nursing care.
The occurrence of infection complications is an important issue during stroke care. A good example of personalized medicine in cerebrovascular diseases is the prediction of the risk of infection-related complications developing in an individual stroke patient [17]. The incidence of infectious complications during stroke treatment is not part of the RES-Q registry. However, infectious complications are required to be assessed as a part of hospital nosocomial infection monitoring.
There are currently more than 70 hospitals across the Republic of Moldova [18]. There are limited resources and infrastructure for stroke care and treatment, including a shortage of staff with expertise in stroke or who are up skilled to manage stroke according to best practice in hospitals. No more than 3 stroke units are available to service a population of more than 2.6 million [19, 20], suggesting that the vast majority of patients may not receive adequate evidence-based care. Therefore, there is an urgent need for more stroke units, and improved management of stroke as a medical emergency, and greater provision of specialized care across the country.
In 2021, we successfully implemented the new RES-Q Comprehensive form, which collects information about: (1) risk factors, medication, the modified Rankin Scale score (mRS), blood glucose, blood pressure, and cholesterol on admission; (2) antidotes for oral anticoagulants, rtPA dosage, and the TICI score; (3) brain imaging details (ASPECTS score, CTA/MRA occlusion, and CT/MR perfusion deficit), brain imaging after 24 hours and detection of hemorrhages/infarcts; (4) physiotherapy, ergotherapy, NIHSS at discharge and mRS at 90 days. These data will allow us to better understand the risk factors for stroke, to better reflect needs in understanding modern treatments for stroke, and to assess the clinical outcomes by the most widely used disability score – modified Rankin Scale (mRS) score at hospital discharge and at 3 months (90 days) following hospital discharge. Documentation of a mRS obtained within the 90-day timeframe (75 to 105 days after hospital discharge) via telephone or in-person is acceptable. If the patient cannot be interviewed because of communication deficits or other limitations, an interview with the patient's caregiver is acceptable.
Good management of risk factors can lead to dramatic changes in the incidence of stroke, and RES-Q Comprehensive form offered the possibility to study some of them [21]. The mean age of stroke patients in 2021 was 66.73 ± 11.45 years old, and in 2022 it was 67.71 ± 10.55 years old. In 2021, diabetes mellitus was noticed in 31.25% of patients, and only 63.2% of diabetic patients were receiving antidiabetic treatment, but in 2022, there were 28.2% of diabetic patients, and 65% were receiving treatment. In 2021, dyslipidemia was noticed in 46.85% of subjects (vs. 15.5% in 2022), congestive heart failure in 28.13% (vs. 14.1% in 2022), 23.08% had AF (vs. 29% in 2022), and 20.2% were smokers (vs. 7.04% in 2022). 6.25% of AF patients were receiving warfarin, and 15.62% received rivaroxaban in 2021, but the next year, warfarin was recommended for 10.5% of patients, and rivaroxaban for 11.0%. 81.25% of patients were receiving aspirin treatment at stroke onset. In 2021, the mean values of systolic and diastolic blood pressure at admission were 148.33 ± 37.45 mmHg and, respectively, 85.55 ± 23.64 mmHg, but in 2022, they were 166.05 ± 30.46 mmHg and, respectively, 92.39 ± 16.08 mmHg. In 2021, the mean value of blood sugar at admission was 7.62 ± 3.59 mmol/l, but in 2022, it was 7.97 ± 3.16 mmol/l, and the mean value of serum cholesterol was 5.05 ± 1.02 mmol/l and, respectively, in the following year, it was 4.51 ± 1.54 mmol/l. In 2021, 23.33% of stroke patients were tested for COVID-19, while in 2022 a smaller number (8.5%) were tested. A rate of 16.4% of patients in 2021, and a rate of 8.5% of patients in 2022 had repeated strokes.
In 2022, it was found that the average period from the onset of the disease to admission to the hospital was 249.5 ± 275.01 minutes, and only 33.8% of patients with stroke were admitted during the therapeutic window period.
Conclusions
Most hospitalized patients with acute stroke admitted to the Institute of Emergency Medicine, Chisinau, Republic of Moldova, received evidence-based care. The COVID-19 pandemic has left its mark on the number of stroke hospitalizations, but the quality of in-hospital stroke care was not dramatically affected. However, the considerable delay in time from stroke onset to hospital arrival remains an important issue. More than 70% of those with stroke admitted to our hospital did not arrive in less than 4.5 hours after experiencing stroke symptoms, and they were then potentially ineligible for intravenous thrombolysis therapy.
List of abbreviations used
RES-Q – the Registry of Stroke Care Quality; AF – atrial fibrillation; TIA – transient ischemic attack; CT – computed tomography; CTA – computed tomography angiography; MRA – magnetic resonance angiography; ECG – electrocardiogram; NIHSS – National Institutes of Health Stroke Scale; mRS – modified Rankin Scale score.
Competing interests
None declared
Authors’ contributions
SG interpreted the data, drafted the manuscript, and revised the manuscript critically; NC collected the data, made statistical analysis, drafted the manuscript, and interpreted the data; IC interpreted the data and drafted the manuscript; SP interpreted the data and drafted the manuscript; EZ revised the manuscript critically; IS collected the data. All the authors revised and approved the final version of the manuscript.
Funding
RES-Q is supported by an unrestricted European Stroke Organization grant. RES-Q development and data collection have been supported by the COST Association – the IRENE COST Action, CA18118. Additional financial support is provided by St. Anne's University Hospital Brno – International Clinical Research Center. The authors are independent and take responsibility for the integrity of the data and the accuracy of the data analysis.
Authors’s ORCID ID
Stansilav Groppa - https://orcid.org/0000-0002-2120-2408
Natalia Ciobanu - https://orcid.org/0000-0002-9492-8058
Igor Crivorucica - https://orcid.org/0000-0002-0816-4339
Eremei Zota - https://orcid.org/0000-0003-1365-2633
Sorin Plotnicu - https://orcid.org/0000-0002-0008-6954
Irina Smetanca - https://orcid.org/0000-0002-2199-6578
References
Manole E., Lisnic V., Groppa S., Costru-Taşnic E., Filioglo A., Odainic O., Ciobanu N., More V., Dragan Gh. Registrul RES-Q în Republica Moldova – primele rezultate naţionale în cadrul unui proiect international [RES-Q Registry in the Republic of Moldova – the first national results in an international project]. Bull Acad Sci. Med Sci., 2017; (5): 72-77. Romanian.
Groppa S. The registry of stroke care quality (RES-Q) in Republic of Moldova. European Stroke Journal, 2019; Vol. 4 (1S): 779–789.
Groppa S., Manole E. Ciobanu N, et al. The registry of stroke care quality (RES-Q) in the Republic of Moldova: the first nation-wide data on stroke care quality. In: 8th European Teaching Course on Neurorehabilitation; 2018 June 29 - July 1; Eforie Nord, România: Book of Abstracts, 2018; Issue 4, p. 33-34.
Manole E., Groppa S. Costru-Tasnic E., Filioglo A., Odainic O., Ciobanu N., More V., Dragan G., Bornstein N. M., Lisnic V. In-Hospital management in the Republic of Moldova – Analysis of first data of the RES-Q as part of ESO-EAST project. European Stroke Journal. Göteborg, Suedia, 2018; vol. 3 (1S), p. 321-322.
Manole E., Ciobanu N., Crivorucica I., Odainic O., Lisnic V., Zota E., Plotnicu S., Țurcanu Gh., Groppa S., Harco A., Cravcenco N., Cretu N., Todirean R., Dolghier V., Barbaros V., Crijanovschi S., Eleniuc D., Salcuțanu V. Four years’ experience of participation of the Republic of Moldova in the RES-Q Registry. 7th Congress of the Society of Neurologists Issue of the Republic of Moldova, 2021; Vol. 64, p. 34-34.
Mikulík R., Caso V., Bornstein N. M., Svobodova V. Enhancing and accelerating stroke treatment in Eastern European region: Methods and achievement of the ESO EAST program. Eur. Stroke J., 2020; 5 (2): 204-212. doi: 10.1177/2396987319897156.
Groppa S., Zota E., Bodiu A., Gasnas A., Manole E., Ciobanu N., Leahu P., Efremova D., Crivorucica I., Glavan D., Balanuta T. Diagnosis and management of ischemic stroke: time is critical. Mold. Med. J., 2020; 63 (4): 65-74. doi: 10.5281/zenodo.4016820.
Pandey A. S., Daou B. J., Tsai J. P., Zaidi S. F., Salahuddin H., Gemmete J. J., Oliver M. J., Singer J., Elder T. A., Mbabuike N., Adel J. G., Gujrati Y., Saleemi M. A., Siddiqui F. M., Elias A. E., Rehman M. F., Marin H., Chebl A. B., Kole M., Wilseck J. M., Kazmierczak C. D., Mick J. M., Majjhoo A. Q., Naravetla B. R., Rayes M., Luqman A. W., Richards B. F., Kelkar P., Burgess R., Thompson B. G., Chaudhary N., Mazaris P. A., Qahwash O., Razak M. A., Jumaa M. A. Letter: COVID-19 pandemic: the bystander effect on stroke care in Michigan. Neurosurgery, 2020 Jun 4; 87 (3): E397-E399. Available at: [https://doi.org/10.1093/neuros/nyaa252]. Accessed on: 02.02.2022.
Aguiar de Sousa D., van der Worp H. B., Caso V., Cordonnier C., Strbian D., Ntaios G., Schellinger P. D., Sandset E. C. European Stroke Organisation. Maintaining stroke care in Europe during the COVID-19 pandemic: Results from an international survey of stroke professionals and practice recommendations from the European Stroke Organisation. Eur. Stroke J., 2020; 5 (3): 230-236. doi: 10.1177/2396987320933746.
Rudilosso S., Laredo C., Vera V., Vargas M., Renú A., Llull L., Obach V, Amaro S, Urra X., Torres F., Jiménez-Fàbrega F.X., Chamorro Á. Acute stroke care is at risk in the era of COVID-19: experience at a comprehensive stroke center in Barcelona. Stroke, 2020; 51 (7): 1991-5. doi: 10.1161/STROKEAHA.120.030329.
World Health Organization. COVID-19: operational guidance for maintaining essential health services during an outbreak: interim guidance, 25 March 2020. Geneva; World Health Organization, 2020. Available at: [https://apps.who.int/iris/handle/10665/331561]. Accessed on: 04.02.2022.
Siegler J. E., Heslin M. E., Thau L., Smith A., Jovin T. G. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J. Stroke Cerebrovasc. Dis., 2020; 29 (8): 104953. doi: 10.1016/j.jstrokecerebrovasdis.2020.104953.
Powers W. J., Rabinstein A. A., Ackerson T., et al. 2018 guidelines for the early management of patients with acute Ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke., 2018; 49 (3): e46-e110. doi: 10.1161/STR.0000000000000158.
Powers W., Rabinstein A., Ackerson T., Adeoye O., Bambakidis N., Becker K., Biller J., Brown M., Demaerschalk B. M., Hoh B., Jauch E. C., Kidwell C. S., Leslie-Mazwi T. M., Ovbiagele B., Scott P. A., Sheth K. N., Southerland A. M., Summers D. V., Tirschwell D. L. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke., 2019; 50 (12): e344-e418. doi: 10.1161/STR.0000000000000211.
Hankey G. J. Secondary stroke prevention. Lancet Neurol., 2014; 13 (2): 178-194. doi: 10.1016/S1474-4422(13)70255-2.
De Raedt S., De Vos A., Van Binst A-M., De Waele M., Coomans D., Buyl R., De Keyser J. High natural killer cell number might identify stroke patients at risk of developing infections. Neurol. Neuroimmunol. Neuroinflammation., 2015; 2 (2): e71. doi: 10.1212/NXI.0000000000000071.
Guvernul Republicii Moldova [Government of the Republic of Moldova]. Hotărârea nr. 379 din 07.05.2010 cu privire la Programul de dezvoltare a asistenţei medicale spitaliceşti pe anii 2010-2012 [Decision No 379 of 07.05.2010 on the Program for the development of hospital care for the years 2010-2012]. Monitorul Oficial al Republicii Moldova., 2010; (72-74): art. 450. Romanian. Available at: [https://www.legis.md/cautare/getResults?doc_id=2365&lang=ro]. Accessed on: 04.02.2022.
Manole E., Groppa S., Zota E., Crivorucica I., Manea D., Odainic O., Filioglo A., Grecu A., Bornstein N. M. Disparities of in-hospital stroke care quality indicators between moldavian centers with and without stroke units based on stroke registry (res-q), three years data analysis. International Journal of Stroke., 15 (1S): 325.
Glavan D., Gasnaş A., Ciobanu N., Oglindă-Catirău G., Groppa S. Reducing the impact of stroke in the Republic of Moldova – current state and perspectives. Cercetarea în biomedicină și sănătate: calitate, excelență și performanță., 20-22 octombrie 2021; Chişinău, Republica Moldova: 2021, p. 203.
Groppa S, Ciobanu N, Efremova D. Stroke risk factors in the population of the Republic of Moldova. J. Neurol. Sci., 2017; 381(Suppl): 411. Available at: [https://doi.org/10.1016/j.jns.2017.08.3373]. Accessed on: 04.02.2022.