Introduction
COVID-19 infection, that was declared by the World Health Organization (WHO) as pandemic in March 2020, cause a multitude of challenges in the public health system on national and international level. The consequences of the pandemic were felt by triggering an unprecedented crisis that adversely affects not only the physical health of population, but also mental welfare, and socioeconomic wellbeing [1, 2, 3]. Since the start of the pandemic, several variants of SARS-CoV-2 have been identified: alpha, beta, gamma, delta, omicron, each of them with different impact on health and healthcare system. SARS-CoV-2, like other RNA viruses, while adapting to new human hosts, is prone to genetic evolution, resulting in mutant variants that may have different characteristics than the original strains and threatens the progress made so far in limiting the spread of this disease [4]. Only understanding the characteristics of COVID-19 infection and identifying the wide range of factors affecting health and quality of life can be the key to providing viable solutions to improve the management of patients and their physical and psycho-emotional rehabilitation.
The evolution of COVID-19 varies from asymptomatic and mild infection to critical one and death, the most frequent clinical manifestations being fatigue, fever, cough, headache, dyspnea, anosmia, ageusia [5-9]. The presence of comorbidities such as diabetes, malignant tumors, immunosuppression, obesity, chronic renal failure, cardiovascular pathologies, as well as old age are often associated with a more severe course of the disease [10-17]. In aggressive clinical forms, the patients often develop such complications as acute respiratory distress, shock, myocardial damage, heart failure, acute kidney damage, etc. [18-23]. The risk of such complications as venous thromboembolism and pulmonary embolism may persist in some situations and in the post-acute period of COVID-19 [24-29].
The mortality rate during COVID-19 infection varies in different countries and regions, which may reflect differences in the age structure of the population, in the ability to test for suspected cases and seroprevalence, in the manner of reporting death cases, etc. [30-33]. The knowledge of the complexity of COVID-19 disease has evolved over time. Currently reaching the understanding that the risks that the infection presents do not end only at the stage of hospitalization. Acute disease survivors may have various long-term health problems, especially fatigue and cognitive dysfunction [34-40].
The purpose of the present study was to evaluate the impact of SARS CoV-2 infection on the health status of adults hospitalized with the diagnosis of COVID-19 in specialized clinics in the Republic of Moldova. The study examined epidemiological data, clinical features, comorbid conditions, disease progression, and mortality rate of the patients during the acute period of the disease.
Materials and methods
This study is a retrospective cohort, consisting of a sample of 7441 randomly selected patients aged 18 y/o and older, hospitalized with the diagnosis of COVID-19 in 10 public medical institutions in Chisinau municipality, Republic of Moldova, between March 1, 2020 and June 30, 2021. The diagnosis of COVID-19 was confirmed by the detection of SARS CoV-2 RNA by molecular biology tests. The data from the patients’ medical records were processed and stored according to a unified, pre-established form, developed in accordance with the requirements of the „Covid-19 electronic patient record Register” software. The form included epidemiological, socio-demographic, clinical, paraclinical, laboratory data and information on therapeutic management.
The severity of COVID-19 disease was assessed based on two principles (1) according to the National Clinical Protocol and (2) according to the WHO special committee, that permitted to appreciate not only the need for additional oxygen supply, but also the type of oxygen therapy.
Assessment of the form of the disease according to the criteria of the National Clinical Protocol „New type coronavirus infection (COVID-19), PCN-371” [41]:
mild form: patient with any signs and symptoms without shortness of breath, dyspnea or abnormal chest images (without pneumonia);
moderate form: patient with fever and signs of non-severe pneumonia, no need for additional oxygen;
severe form: patient with signs of severe pneumonia (significant dyspnea FR > 30 / min), or / and hypoxemia SpO2 < 94% at rest, or/and PaO2/FiO2 below 300 mmHg, or/and rapid negative evolution of lung imaging over the last 24-48 hours by more than 50%, or/and progressive decrease in peripheral lymphocyte count and rapid increase in lactate;
critical form: patients with COVID-19 and one or more of the following: ARDS; shock; any organ failure, requiring care in the intensive care unit; other conditions with a major danger to the patient's life.
Assessment of the form of the disease according to the 7-point graded scale developed by the WHO special committee (V. 3.0; 3 March, 2020) in randomized multicenter clinical trials [42]:
score 1: non-hospitalized patients without limitation in activity;
score 2: non-hospitalized patients limited in activity, pre-COVID clinical status;
score 3: hospitalized patients without need for oxygen therapy;
score 4: hospitalized patients with oxygen therapy through the mask or nasal cannula;
score 5: patients hospitalized with oxygen therapy with non-invasive high-flow oxygen ventilation;
score 6: hospitalized patients with intubation and mechanical ventilation oxygen therapy or extracorporeal membrane ECMO-oxygenation;
score 7 (deceased patients).
In the present study, death from COVID-19 was defined as a death, that occurred in a patient with a confirmed case of COVID-19 except where there was another clear cause of death that cannot be related to COVID-19, and where there was no complete recovery period between the disease and the time of death, and where the death was not attributed to a pre-existing disease.
Results
The socio-demographic structure of the people in the study was as follows: from urban regions - 5730 (77.01%) patients, from rural regions - 1711 (22.99%) patients, employed - 4051 (54.44%) patients, retired - 1861 (25.01%) patients, unemployed - 1144 (15.37%) patients, disabled - 293 (3.94%) patients, pupils/students - 92 (1.24%) patients. At the time of hospitalization, 325 (4.37%) patients had no medical insurance.
The patients got referrals to the hospitalization by the Emergency Medical Assistance team in 2948 (39.61%) cases; by the medical specialists - 199 (2.67%) cases, by the family doctor - 171 (2.29%) cases. The patients were hospitalized by means of the transfer from the COVID center, or any other healthcare institutions in 3065 (41.19%) cases. On personal address to the inpatient wards were admitted 1058 (14.21%) patients.
For the last 14 days before the illness only 2234 (30.07%) patients mentioned the presence of a close contact with a COVID-19 positive person, and only 67 (0.9%) patients traveled outside the country. Thus, in the absence of the epidemiological clue, COVID-19 disease was the referral diagnosis only in 3360 (45.15%) cases.
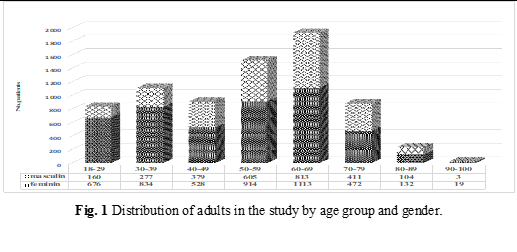
The average age of the patients in the study was 52.83 years, with the prevalence of the 50-59 age group - 20.41% and 60-69 age group - 25.88%. The female gender predominated in the total group – 65.42% (4868 patients), with the male / female ratio below 1 in all age groups (Figure 1).
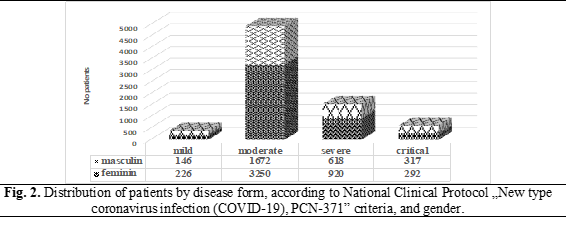
The form of the disease ranged from mild to critical. Mild form was diagnosed in 372 (5,0%) patients, medium - in 4922 (66.15%), severe - 1538 (20.67%), critical - 609 (8.18%) patients (Figure 2). It is essential to specify that the dynamics and profile of hospitalized patients with COVID-19 in the Republic of Moldova has evolved over time according to the severity of the pandemic. Thus, in the first stage, all patients with the confirmed diagnosis of COVID-19 were hospitalized, regardless of age and severity of illnesses (PCN-371 Edition I). In the later stages, starting from mid-June 2020, hospitalization was not mandatory for adults aged 18-60 with asymptomatic and mild forms, without comorbidities and major risk of deterioration (PCN-371 editions II-V). The male/female ratio was under 1 for the mild (0.65), medium (0.51) and severe (0.67) clinical forms, but over 1 in the critical patients (1.08), as seen in Figure 2.
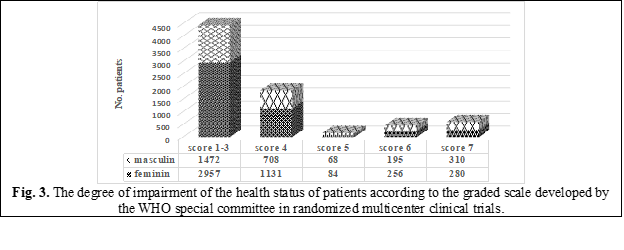
The health impairment of the patients were categorized also according to the graded scale developed by the WHO special committee in randomized multicenter clinical trials that allows assessing the severity of the disease focusing mainly on the need of patients for different types of oxygen therapy. Thus, a score of 3 (no oxygen therapy) had 4429 (59.52%) patients, male/female ratio – 0.50; a score of 4 (oxygen therapy via face mask or nasal cannula) had 1819 (24.45%) patients, male/female ratio – 0.63; a score of 5 (oxygen therapy in ventilation, non-invasive, with the oxygen flow rate increased) - 152 (2.04%) patients, male/female ratio – 0.81; a score of 6 (oxygen therapy by intubation and mechanical ventilation or ECMO) had 451 (6.06%) patients, male / female – 0.76; a score of 7 (deceased) - 590 (7.93%) patients, male/female ratio – 1.11 (Figure 3).
The average age of patients with the mild form of the disease was 42.60 years, moderate form – 50.08 years, severe – 58.02 years, critical – 68.17 years. In general, patients who developed a milder form of the disease had a lower age compared to those who had a more severe course (Table 1).
Table 1. Distribution of patients by age group and disease severity form according to National Clinical Protocol. | ||||||||
| Age group 18-29 (n=836) n (%) | Age group 30-39 (n=1111) n (%) | Age group 40-49 (n=409) n (%) | Age group 50-59 (n=1519) n (%) | Age group 60-69 (n=1926) n (%) | Age group 70-79 (n=883) n (%) | Age group 80-89 (n=236) n (%) | Age group 90-99 (n=23) n (%) |
Mild | 93 (11.12%) | 82 (7.38%) | 64 (7.05%) | 79 (5.20%) | 40 (2.07%) | 13 (1.47%) | 1 (0.42%) | 0 |
Moderate | 675 (80.74%) | 889 (80.01%) | 639 (70.45%) | 993 (65.37%) | 1189 (61.73%) | 453 (51.30%) | 82 (34.74%) | 2 (8.69%) |
Severe | 66 (7.89%) | 130 (11.7%) | 118 (20.72%) | 363 (23.89%) | 477 (24.76%) | 234 (26.50%) | 70 (29.66%) | 10 (43.47%) |
Critical | 2 (0.23%) | 10 (0.9%) | 16 (1.76%) | 84 (5.52%) | 220 (11.42%) | 183 (20.72%) | 83 (35.16%) | 11 (47.82%) |
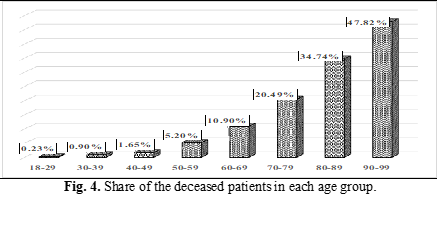
After completing the treatment in the hospital were discharged home 6575 (88.36%) patients, transferred to other public medical and health institutions - 276 (3.70%) patients, died of COVID-19 disease - 590 (7.92%) patients. Thus, each 8-th hospitalized person in the study lot died. The average age of the deceased was 68.37 years, the majority belonging to the age group 60-69 (35.59%) and 70-79 (30.67%). Analyzing the share of the deceased in each age group, the following profile was formed: 18-29 y/o - 2 patients out of 836 died; 30-39 y/o - 10 out of 1111; 40-49 y/o - 15 out of 907; 50-59 y/o - 79 out of 1519; 60-69 y/o - 210 out of 1926; 70-79 y/o - 181 out of 883; 80-89 y/o 82 - out of 236; 90-99 y/o - 11 out of 23 (Figure 4).
The male gender had a negative impact upon the cases of the deceased patients, male/female ratio – 1.1 (310/280), while among the survivors the female sex prevailed: male/female ratio in severe form – 0.67 (618/920), in the medium form – 0.51 (1672/3250), in the mild form – 0.64 (146/226). Similar data of disaggregation by gender with the case-fatality rate greater than 1 for the male sex have been reported by several researchers from different countries affected by COVID-19 [43-46].
During hospitalization the main complaints of patients were: fever - 5742 (77.16%) patients, fatigue or physical asthenia - 6613 (88.87%), cough - 5467 (73.47%), and headache - 4063 (54.60%) patients. Such clinical manifestations as pharyngitis, ageusia and hypo/anosmia were more often complained by young people in the age group 18-29 and 30-39, while such manifestations as dyspnea and vertigo - in people aged over 40, and the newly emerging behavioral changes - in those aged over 70 (Table 2).
Table 2. The most common clinical manifestations during the course of the disease depending on the age group (%) | ||||||||
Clinical manifestation | Age group 18-29 (n=836) n (%) | Age group 30-39 (n=1111) n (%) | Age group 40-49 (n=907) n (%) | Age group 50-59 (n=1519) n (%) | Age group 60-69 (n=1926) n (%) | Age group 70-79 (n=883) n (%) | Age group 80-89 (n=236) n (%) | Age group 90-99 (n=23) n (%) |
Ageusia | 173 (20.69%) | 207 (18.63%) | 92 (10.14%) | 111 (7.31%) | 127 (6.59%) | 45 (5.10%) | 6 (2.54%) | 2 (8.70%) |
Arthralgia | 30 (3.59%) | 55 (4.95%) | 72 (7.94%) | 126 (8.29%) | 172 (8.93%) | 84 (9.51%) | 15 (6.36%) | 2 (8.7%) |
Behavior changes | 3 (0.36%) | 4 (0.36%) | 14 (1.43%) | 12 (0.79%) | 31 (1.61%) | 29 (3.28%) | 9 (3.81%) | 4 (17.39%) |
Cough | 533 (63.76%) | 785 (70.66%) | 675 (74.42%) | 1169 (76.96%) | 1459 (75.75%) | 652 (73.84%) | 181 (76.69%) | 13 (56.52%) |
Diarrhea | 24 (2.87%) | 39 (3.51%) | 33 (3.64%) | 49 (3.23%) | 63 (3.27%) | 21 (2.38) | 90 (3.81%) | 0.00 |
Dyspnea | 168 (20.10%) | 341 (30.69%) | 487 (53.69%) | 945 (62.21%) | 1308 (67.91%) | 604 (68.40%) | 173 (73.31%) | 13 (56.52%) |
Fatigue/asthenia | 726 (86.84%) | 944 (84.97%) | 80 (88.20%) | 1385 (91.18%) | 1749 (90.81%) | 786 (89.01%) | 204 (86.44%) | 19 (82.1%) |
Fever <38.0°C | 515 (61.60%) | 676 (60.85%) | 512 (56.45%) | 878 (57.80%) | 1111 (57.68%) | 528 (59.80%) | 129 (58.90%) | 3 (13.04%) |
Fever >38.0°C | 110 (13.16%) | 196 (17.64%) | 205 (22.60%) | 304 (20.01%) | 359 (18.64%) | 156 (17.67%) | 37 (15.68%) | 13 (56.52%) |
Headache | 477 (57.06%) | 653 (58.78%) | 478 (52.70%) | 815 (53.65%) | 1025 (53.22%) | 471 (53.34%) | 133 (56.36%) | 11 (47.83%) |
Hypo/anosmia | 286 (34.21%) | 346 (31.14%) | 135 (14.88%) | 145 (9.87%) | 171 (8.88%) | 51 (5.78%) | 8 (3.39%) | 2 (8.70%) |
Myalgia | 132 (15.79%) | 212 (19.08%) | 237 (26.13%) | 346 (22.78%) | 4280 (22.22%) | 178 (20.16%) | 42 (17.80%) | 3 (13.04%) |
Pharyngitis | 451 (53.95%) | 501 (45.09%) | 206 (22.71%) | 236 (15.54%) | 261 (13.55%) | 92 (10.42%) | 23 (9.75%) | 2 (8.70%) |
Vertigo | 32 (3.83%) | 53 (4.77%) | 87 (9.59%) | 142 (9.35%) | 177 (9.19%) | 101 (11.44%) | 21 (8.90%) | 2 (8.70%) |
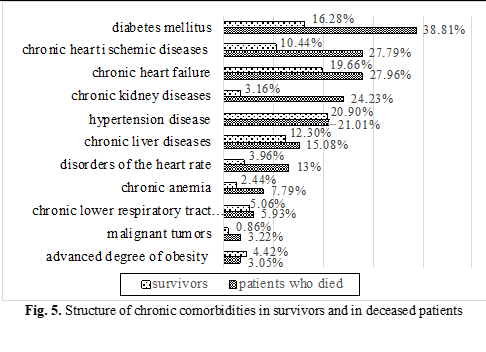
The patients who have died of COVID-19 (590 patients) suffered from various chronic diseases such as hypertension - 124 (21.01%) patients, chronic ischemic heart diseases - 164 (27.79%), disorders of the heart rate - 78 (13.22%), chronic heart failure - 165 (27.96%), diabetes mellitus - 229 (38.81%), chronic kidney diseases - 143 (24.23%); chronic liver diseases - 89 (15.08%), chronic anemia - 46 (7.79%), chronic lower respiratory tract diseases - 35 (5.93%), malignant tumors - 19 (3.22%), advanced degree of obesity - 18 (3.05%). Chronic comorbidities of survivors discharged at home (6575 patients) were as follows: hypertension diseases - 1374 (20.90%) patients; chronic ischemic heart diseases - 687 (10.44%), disorders of the heart rate - 261 (3.96%), chronic heart failure - 1293 (19.66%), diabetes mellitus - 1071 (16.28%), chronic liver diseases - 809 (12.30%), chronic kidney diseases - 208 (3.16%), chronic lower respiratory tract diseases 333 (5.06%), advanced degree of obesity - 291 (4,42%), chronic anemia - 161 (2.44%), malignant tumors - 57 (0.86%) patients (Figure 5). Thus, the presence of such chronic comorbidities as diabetes mellitus, chronic heart failure, chronic ischemic heart diseases, heart rate disorders, chronic kidney diseases, malignant tumors, chronic anemia – increase statistically significantly the probability of patients having an unfavorable prognosis in COVID-19 (P = 0.0001 in the Fisher test).
Antibiotic treatment was administered in 6819 (91.64%) cases, including: 359 (5.26%) patients with no lung imaging pathologies detected during the disease and 253 (3,71%) patients diagnosed with mild form of the disease.
The average duration of hospitalization varied depending on the form of the disease and the age of the patients. The fewest days of hospitalization - 13 days had patients aged under 40 years, while the duration of hospitalization in patients aged over 40 years was 15-16 days. The mean duration of hospitalization in deceased patients was 12 days. It should be mentioned that the duration of hospitalization, especially in mild and moderate severity cases, was influenced by the discharge criteria stipulated in the orders and recommendations in force that evolved over time according to the severity of the pandemic and the capacities of the health system (PCN-371 editions I-V).
In COVID-19 the quality of life is affected not only during the acute period of the disease, but also long after. People who were discharged at home continued to complained of different clinical manifestations such as fatigue, physical asthenia, cough, headache, dyspnea, myalgia, sub-febrility in 2646 (40.25%) cases. Out of 3929 patients who had no complaints at discharge in 2207 (56.17%) cases pulmonary imaging (Rx or CT) were abnormal.
Discussions
The source of SARS-CoV-2 infection remains unrevealed in most cases. Thus, out of the 7441 COVID-19 patients included in the study less than 1/3 mentioned the presence of contact with a COVID-19 positive. According to the WHO recommendations, the identification of the source of infection by case investigation „backward tracing” is essential to detect the transmission chains of SARS-CoV-2 [47]. Respectively, in more than ⅔ of the cases, neither the source of infection nor the risk factors that would favor the transmission of the infection to the patients were identified, leading to the delaying in applying of anti-epidemic prophylactic measures in general population. The similarity of clinical manifestations of COVID-19 with other respiratory infections in the absence of epidemiological connection with the source of infection also explains that in more than ½ of the cases the referral diagnosis was other than COVID-19 infection.
More than ¼ of those hospitalized have severe or critical forms of COVID-19 and more than 1/3 of patients require oxygen therapy, and every 6-th patient needs non-invasive high-flow oxygen ventilation or mechanical ventilation.
Patients aged over 50 years tend to have more severe clinical manifestations and a higher fatality rate, which means that they require more careful monitoring and more comprehensive medical interventions. Thus, every 9-th patient over 60 years, every 5-th patient over 70 years, every 3-rd patient over 80 years, 2-nd patient over 90 years died. According to our study, the proportion of patients who died (7.93%) was higher compared to some studies in other countries.
The non-specific complains of the patients with COVID-19 do not allow, without special laboratory investigations, their differentiation from other pathologies of the respiratory tract. Most patients manifest physical fatigue or asthenia, fever, cough, and each 2-nd - headache. Such complaints as pharyngitis, ageusia, and hypo/anosmia are characteristic mainly of young people, and dyspnea and behavioral changes - of the elderly. Disorders of the gastrointestinal system caused by COVID-19 are insignificant in number and intensity in all age groups.
The presence of certain comorbidities such as diabetes mellitus, chronic heart failure, chronic ischemic heart diseases, heart rhythm disorders, chronic kidney diseases, malignant tumors, chronic anemia increase significantly the likelihood of patients having an unfavorable prognosis in COVID-19 (deceased vs survivors). Thus, the vaccination for COVID-19 should not be delayed in this category of patients. Surprisingly, in our study, chronic lower respiratory tract diseases do not influence dramatically the evolution of COVID-19, as was suggested previously.
Antibiotics were administered empirically, without laboratory validation, in majority of the hospitalized patients. In pandemic period, when there is a very high level of hospitalization, the excessive and unjustified administration of antibiotics can become dangerous, leading to different complication, including infection with Clostridium difficile, which can only aggravate the evolution of COVID-19 disease.
Discharge from the hospital does not mean recovery for majority of the patients, who continue to present different clinical manifestations, imaging and paraclinical pathologies. There should be additional investigations regarding clinical manifestation of Long-Covid and duration of the recovery period of the hospitalized patients. In COVID-19 the favorable prognosis and complete recuperation at discharge is most commonly associated with young age under 40 years, female sex and the lack of chronic comorbidities.
Conclusions
The uncertainty of the source of infection lead to delay specific anti-epidemic prophylactic public health measures, contributing to uncontrolled spread of COVID-19 and maintaining pandemic situation.
In providing a hospital-type medical care to the patients with COVID-19 the emphasis should be placed mainly on adults over the age of 50.
There is no specific clinical manifestation in COVID-19, characteristic for majority of the patients, that would allow to distinguish the disease from other pathologies, without special laboratory investigations.
Age over 60, male sex, chronic cardiovascular diseases, diabetes mellitus, chronic kidneys diseases, and malignant tumors unfavorable influence the evolution of COVID-19.
Antibiotic administration remains at a high level in hospitalized patients and is often unjustified and unnecessary.
The most of the discharged patients need supplementary period to complete recovery.
Competing interests
None declared
Authors’ contributions
All authors contributed equally to the research, data analysis, and writing of the manuscript. Final manuscript was read and approved by all authors
Authors’ ORCID IDs
Galina Buta - https://orcid.org/0000-0002-7376-1498
Stela Cojocaru - https://orcid.org/0000-0002-1420-8772
Raisa Puia - https://orcid.org/0000-0003-4988-7442
Tudor Costru - https://orcid.org/0000-0002-9245-1399
References
Haldane V., De Foo C., Abdalla S.M., et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nature Medicine, 2021; 27 (6): 964-980. doi: 10.1038/s41591-021-01381-y.
Akay A. The local and global mental health effects of the Covid-19 pandemic. Econ Hum Biol.; 2022; 45:101095. doi: 10.1016/j.ehb.2021.101095.
Hasan M.Z., Neill R., Das P., et al. Integrated health service delivery during COVID-19: a scoping review of published evidence from low-income and lower-middle-income countries. BMJ Glob Health, 2021; 6 (6): e005667. doi: 10.1136/bmjgh-2021-005667.
Long B., Carius B.M., Chavez S., et al. Clinical update on COVID-19 for the emergency clinician: Presentation and evaluation. Am. J. Emerg. Med.; 2022; 54: 46-57. doi: 10.1016/j.ajem.2022.01.028.
Tsai P.H., Lai W.Y., Lin Y.Y., et al. Clinical manifestation and disease progression in COVID-19 infection. Journal of the Chinese Medical Association; 2021; 84 (1): 3-8. doi: 10.1097/jcma.0000000000000463.
Koupaei M., Mohamadi M.H., Yashmi I., et al. Clinical manifestations, treatment options, and comorbidities in COVID-19 relapse patients: A systematic review. J. Clin. Lab. Anal.; 2022; Apr 8:e24402. doi: 10.1002/jcla.24402.
Blair P.W., Brown D.M., Jang M., et al. The Clinical Course of COVID-19 in the Outpatient Setting: A Prospective Cohort Study. Open Forum Infectious Diseases; 2021; 8 (2): ofab007. doi: 10.1093/ofid/ofab007.
Sung H.K., Kim J.Y., Heo J., et al. Clinical Course and Outcomes of 3,060 Patients with Coronavirus Disease 2019 in Korea, January-May 2020. Journal of Korean Medical Science; 2020; 35 (30): e280. doi: 10.3346/jkms.2020.35.e280.
Guan W.J., Ni Z.Y., Hu Y., et al. Clinical Characteristics of Coronavirus Disease 2019 in China. New English Journal of Medicine; 2020; 382 (18): 1708-1720. doi: 10.1056/NEJMoa2002032.
Sanyaolu A., Okorie C., Marinkovic A., et al. Comorbidity and its Impact on Patients with COVID-19. SN Comprehensive Clinical Medicine; 2020; 2 (8): 1069-1076. doi: 10.1007/s42399-020-00363-4.
Kaur H., Thakur J.S., Paika R., et al. Impact of Underlying Comorbidities on Mortality in SARS-COV-2 Infected Cancer Patients: A Systematic Review and Meta-Analysis. Asian Pac. J. Cancer Prev.; 2021; 22 (5): 1333-1349. doi: 10.31557/APJCP.2021.22.5.1333.
Singh A.K., Gupta R., Ghosh A., et al. Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab. Syndr.; 2020; 14 (4): 303-310. doi: 10.1016/j.dsx.2020.04.004.
Li J., Huang D.Q., Zou B., et al. Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J. Med. Virol.; 2021; 93 (3): 1449-1458. doi: 10.1002/jmv.26424.
Cheng Y., Luo R., Wang K., et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int.; 2020; 97 (5): 829-838. doi: 10.1016/j.kint.2020.03.005.
Hessami A., Shamshirian A., Heydari K., et al. Cardiovascular diseases burden in COVID-19: Systematic review and meta-analysis. Am. J. Emerg. Med.; 2020; S0735-6757(20)30908-6. doi: 10.1016/j.ajem.2020.10.022.
Holban T., Cojocaru S., Iarovoi L., Băstrițchi I., Russu I., Potâng-Rașcov V. Manifestările clinice și particularitățile evolutive în infecția COVID-19 (review). Moldovan Journal of Health Science. Chișinău, vol 24 (2), 2020, 70-83. ISSN ISSN 2345-1467.
Ng W.H., Tipih T., Makoah N.A., et al. Comorbidities in SARS-CoV-2 Patients: a Systematic Review and Meta-Analysis. mBio.; 2021; 12 (1): e03647-20. doi: 10.1128/mBio.03647-20.
Wang Y., Lu X., Li Y., et al. Clinical Course and Outcomes of 344 Intensive Care Patients with COVID-19. Respir. Crit. Care Med.; 2020; 201 (11): 1430-1434. doi: 10.1164/rccm.202003-0736LE.
Yang X., Yu Y., Xu J., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med.; 2020; 8 (5): 475-481. doi: 10.1016/S2213-2600(20)30079-5.
Contou D., Cally R., Sarfati F., et al. Causes and timing of death in critically ill COVID-19 patients. Crit. Care; 2021; 25 (1): 79. doi: 10.1186/s13054-021-03492-x.
Roquetaillade C., Bredin S., Lascarrou J.B., et al. Timing and causes of death in severe COVID-19 patients. Crit. Care.; 2021; 25 (1): 224. doi: 10.1186/s13054-021-03639-w.
Elezkurtaj S., Greuel S., Ihlow J., et al. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci. Rep.; 2021; 11 (1): 4263. doi: 10.1038/s41598-021-82862-5.
Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet; 2020; 395 (10229): 1054-1062. doi: 10.1016/S0140-6736(20)30566-3.
Elsoukkary S.S., Mostyka M., Dillard A., et al. Autopsy Findings in 32 Patients with COVID-19: A Single-Institution Experience. Pathobiology; 2021; 88(1): 56-68. doi: 10.1159/000511325.
Satturwar S., Fowkes M., Farver C., et al. Postmortem Findings Associated With SARS-CoV-2: Systematic Review and Meta-analysis. Am. J. Surg. Pathol.; 2021; 45 (5): 587-603. doi: 10.1097/PAS.0000000000001650.
Suh Y.J., Hong H., Ohana M., et al. Pulmonary Embolism and Deep Vein Thrombosis in COVID-19: A Systematic Review and Meta-Analysis. Radiology; 2021; 298 (2): E70-E80. doi: 10.1148/radiol.2020203557.
Jevnikar M., Sanchez O., Humbert M., et al. Prevalence of pulmonary embolism in patients with COVID-19 at the time of hospital admission and role for pre-test probability scores and home treatment. Eur. Respir. J.; 2021; 2101033. doi: 10.1183/13993003.01033-2021.
Van Twist D.J.L., Luu I.H.Y., Kroon F.P.B., et al. Pulmonary Embolism in COVID-19: The Actual Prevalence Remains Unclear. Radiology; 2021; 299 (2): E254. doi: 10.1148/radiol.2021204671.
Malas M.B., Naazie I.N., Elsayed N., et al. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: A systematic review and meta-analysis. E.Clinical Medicine; 2020; 100639. doi: 10.1016/j.eclinm.2020.100639.
Ioannidis J. Infection fatality rate of COVID-19 inferred from seroprevalence data. Bull. World Health Organ; 2021; 99 (1): 19-33F. doi: 10.2471/BLT.20.265892.
Karlinsky A., Kobak D. The World Mortality Dataset: Tracking excess mortality across countries during the COVID-19 pandemic. medRxiv; 2021; 2021.01.27.21250604. doi: 10.1101/2021.01.27.21250604.
Islam N., Shkolnikov V.M., Acosta R.J., et al. Excess deaths associated with covid-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. B.M.J.; 2021; 373: n1137. doi: 10.1136/bmj.n1137.
Fountoulakis K.N., Fountoulakis N.K., Koupidis S.A., et al. Factors determining different death rates because of the COVID-19 outbreak among countries. J. Public Health (Oxf.); 2020; 42 (4): 681-687. doi:10.1093/pubmed/fdaa119.
Nalbandian A., Sehgal K., Gupta A., et al. Post-acute COVID-19 syndrome. Nat. Med.; 2021; 27 (4): 601-615. doi: 10.1038/s41591-021-01283-z.
Darcis G., Bouquegneau A., Maes N., et al. Long-term clinical follow up of patients suffering from moderate to severe COVID-19 infection: A monocentric prospective observational cohort study; J. Infect. Dis.; 2021; 109: 209–16. doi: 10.1016/j.ijid.2021.07.016.
Bourmistrova N.W., Solomon T., Braude P., et al. Long-term effects of COVID-19 on mental health: A systematic review. J. Affect. Disord.; 2022; Feb 15; 299: 118-125. doi: 10.1016/j.jad.2021.11.031.
Lopez-Leon S., Wegman-Ostrosky T., Perelman C., et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci. Rep.; 2021; 11 (1):16144. doi: 10.1038/s41598-021-95565-8.
Davis H.E., Assaf G.S., McCorkell L., et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. E. Clinical Medicine; 2021; Jul 15: 101019. doi: 10.1016/j.eclinm.2021.101019.
Beghi E, Helbok R, Ozturk S, et al. Short- and long-term outcome and predictors in an international cohort of patients with neuro-COVID-19. Eur. J. Neurol.; 2022; 29 (6): 1663-1684. doi: 10.1111/ene.15293.
Drake T.M., Riad A.M., Fairfield C.J., et al. Characterisation of in-hospital complications associated with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol UK: a prospective, multicentre cohort study. Lancet; 2021; 398 (10296): 223-237. doi: 10.1016/S0140-6736(21)00799-6.
MSMPS, „Infecția cu coronavirus de tip nou (Covid-19), PCN 371,” https://msmps.gov.md/.
Ader F., Discovery French Trial Management Team. Protocol for the DisCoVeRy trial: multicentre, adaptive, randomised trial of the safety and efficacy of treatments for COVID-19 in hospitalised adults. B.M.J.; 2020; 10 (9): e041437. doi: 10.1136/bmjopen-2020-041437.
Thompson K., Vassallo A., Finfer S., Woodward M. Renewed rationale for sex- and gender-disaggregated research: A COVID-19 commentary review. Womens Health (Lond.); 2022;18:17455065221076738. doi:10.1177/17455065221076738.
Jin J.M., Bai P., He W., et al. Gender Differences in Patients With COVID-19: Focus on Severity and Mortality. Front Public Health; 2020; Apr. 29; 8:152. doi: 10.3389/fpubh.2020.00152.
Gomez J.M.D., Du-Fay-de-Lavallaz J.M., Fugar S., et al. Sex Differences in COVID-19 Hospitalization and Mortality. J. Womens Health (Larchmt); 2021; 30 (5): 646-653. doi: 10.1089/jwh.2020.8948.
Vahidy F.S., Pan A.P., Ahnstedt H., et al. Sex differences in susceptibility, severity, and outcomes of coronavirus disease 2019: Cross-sectional analysis from a diverse US metropolitan area. PLoS One; 2021;16 (1): e0245556. doi: 10.1371/journal.pone.0245556.