Introduction
Currently, guidelines for the treatment of acne, as well as safety, tolerability and patient preferences are needed to determine the appropriate treatment steps. The literature may support evidence-based physician recommendations based on these factors. Thus, the bibliographic references, are focused on the efficacy and tolerability of the combined topical therapies used in the treatment of acne. Proceeding from the multifactorial pathogenesis of acne and the obstacles to adherence to treatment, scientists opt for optimization of topical anti-acne pharmaceutical forms which shall lead to greater confidence in the future of patients [1].
Acne vulgaris is a chronic dermatological condition that affects about 80% of adolescents globally, of which 20% have a mild and severe form. The age of onset is between 10 and 17 years for females and between 14 and 19 years for males, but it can also occur at an older age [2, 3]. Acne is an inflammatory condition of the pilosebaceous unit of the skin, which occurs through excessive production of sebum, which leads to the formation of comedones, by blocking the pilosebaceous unit, by hyperkeratinization hair, blocking the elimination of sebum, with the formation of blackheads, and by added bacterial infections [4]. Anaerobic Propionibacterium acnes develops in acne lesions, maintaining inflammation and forming whitehead lesions characteristic of acne: papules, pustules, nodules and cysts, as shown in figure 1. Acne is often associated with seborrhea, so it affects especially the areas where the sebaceous glands are more abundant: face, head, neck, upper part (chest and arms) [5].
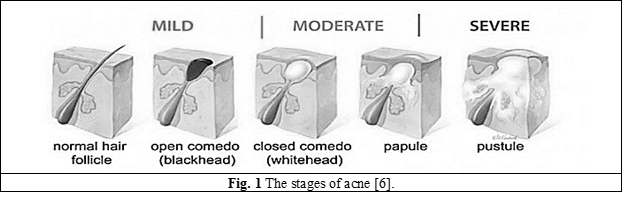
Topical therapy in acne vulgaris includes multiple options: retinoids, antibiotics, substances with antibacterial, keratolytic, antimicrobial action (salicylic acid, sulfur, chloramphenicol, etc.). The choice of topical therapy is influenced by the patient's age, the location of the lesions, their extent and severity, as well as the patient's preference [6, 7].
According to international specialized literature, the most commonly used medications for the treatment of various forms of acne are topical retinoids (vitamin A derivatives), known for 4 generations to bind the specific retinoid receptors at the keratinocyte level, they reduce keratinization and follicular adhesion, leading to inhibition of comedogenesis and increased skin penetration for other topical treatments [8]. In international dermatological practice, retinoids are recommended for topical use due to their anti-comedogenic and anti-inflammatory effects as initiation or maintenance therapy and also for relapse prevention [9-11]. The combination of a topical retinoid with an antimicrobial agent is recommended as a first-line treatment for most patients, as it targets the multiple pathological factors that underlie the appearance of inflammatory and non-inflammatory acne lesions [12]. Retinoids stimulate the turnover of epithelial cells, with the release of the cutaneous pilosebaceous unit, and have anti-inflammatory properties by inhibiting the chemotaxis of neutrophils and monocytes [3]. Their impact varies with vehicle formation, skin type, frequency and mode of application, use of moisturizers, and environmental factors such as sun exposure or temperature [13, 14].
Current research, in accordance with published guidelines and protocols, considering the effectiveness, safety and tolerability of anti-acne treatment, as well as patient allegations can help the physician to achieve an effective evidence-based effect on all factors that cause acne.
The aim of this study is to get an overview of the current and future direction of topical pharmacotherapy for acne and evaluate industrial drugs and magistral formulations available in the Republic of Moldova, also to identify the most prescribed API (active pharmaceutical ingredients) by domestic dermatologists.
Material and methods
In order to achieve the purpose of the paper, the materials used were in the form of scientific publications, national and international guides on the methods of treatment of various forms of acne. As methods of analysis were applied statistical, systemic, informational, and sociological analysis. Analytical evaluation of State Drug Nomenclature and Classification of the administrative authority Agency for Medicines and Medical Devices by pharmaceutical active ingredients and manufacturing countries, also evaluation of the magistral prescriptions of the Vasile Procopisin UPhC (University Pharmaceutical Center) regarding topical pharmaceutical forms used in the treatment of acne by age groups (11-16 y.o., 17-21 y.o., 21-28 y.o., 29 y.o. and more), by pharmaceutical form (ointments, pastes, creams, liniments) and by pharmaceutical active ingredients.
Results and discussions
There is currently a wide variety of anti-acne treatment options available in the R. of Moldova, offering integrative therapeutic approaches so that they are tailored to the patient's needs. The choice of treatment depends on the etiopathogenic cause of the acne, the personal or family history, the treatment used previously and the response obtained to these therapies, in association with a thorough clinical examination of the patient. Due to the fact that acne is a condition that can lead to psychosocial impairment of patients, it is important to start treatment as early as possible [15, 16]. The goals of anti-acne therapy is to reduce the number and severity of existing lesions, to prevent the formation of new lesions and the formation of permanent scars, leading to disfigurement. Thus, for anti-acne therapy, specialists from the R. of Moldova approach a complex treatment, in which topical therapy is associated with systemic therapy. For instance, in the Republic of Moldova at the moment is registered the 1st generation retinoid - isotretinoin - for oral administration in the form of capsules.
Topical therapy is the first intention in mild and moderate cases of acne, and the combination of several topical preparations for various aspects of acne pathogenesis may be useful. Most often dermatologists from different curative-prophylactic institutions opt for industrial pharmaceutical forms and mainly, in the form of ointment, cream, gel, suspension and local applications. In patients with sensitive skin prone to acne, doctors often prescribe such pharmaceutical forms as ointments-emulsions, liquid creams, hydrogels, which have permeable properties (moisturizing), but do not make skin oily, are easily washable, and are more effective from a biopharmaceutical point of view [17]. The penetration of topical drugs into and through the skin can be achieved in two ways: (1) through the pores - the walls of the hair follicles (transfollicular) and less through the sweat glands; (2) transepidermal - passing through the epidermis.
Thus, the skin absorbs the following categories of substances: substances soluble in skin lipoids (nonpolar organic solvents); substances soluble in both oil and water; fat-soluble volatile substances, due to a wide variety of ointment bases [18]. The factors that influence the penetration of topically administered drugs and implicitly the bioavailability and the action of the pharmaceutical form are the factors related to the structure and conditions of the skin, characteristics of the active and auxiliary substances, the composition of the applied topical formula, a special role being played by the vehicle - the excipient or the ointment base.
Nowadays, there is a wide assortment of dermato-products with singular or multicomponent medicines. Pharmaceutical industry has entered a new era, as there is a growing interest in increasing the standards of quality of dosage forms, through the implementation of more structured development and manufacturing technologies [19]. For topical formulation, as a semi-solid dosage form, that has suitable consistency for the treatment of skin diseases caused by bacteria, a key challenge relay to the properties of the active substance in association with excipient bases [20] and the objective in development includes physical-chemical studies of API proprieties and excipients and their compatibility, release rate, stability, in vitro and in vivo drug permeability studies, etc. Industrial topical anti-acne dosage forms are available in various pharmaceutical forms, majority with conventional, unmodified API release, such as: gels, ointments, creams, lotions, etc. On domestic pharmaceutical market are present dermato-products containing benzoyl peroxide, azelaic acid, sulfur and other substances, as displayed in table 1.
Table 1. Topical industrial preparations used in the treatment of acne available in the Republic of Moldova | |
International common name of the API | Pharmaceutical form, concentration |
Benzoyl peroxide | Cream, 5% |
Azelaic acid | Cream 20%, gel 15% |
Erythromycin | Gel 25 mg/g |
Clindamycin | Gel 10 mg/g |
Sulfur | Paste, 10% |
Zinc oxide | Paste, 10%, ointment, 100 mg/g |
Salicylic acid | Ointment 30 mg/g |
Evaluation of registered anti-acne industrial pharmaceutical forms available in our country revealed that the drugs are from different chemical groups starting with:
benzoyl peroxide is used as an alternative to topical retinoids, associated with antibiotics in the treatment of acne. Benzoyl peroxide has comedolytic effects by increasing the renewal rate of epithelial cells and by favoring the opening of pores blocked by excess sebum and cell debris [21, 22]. Benzoyl peroxide side effects occur especially if high doses are used at the beginning of treatment. These side effects are excessive dry skin, flaking, erythema, sensitization and contact dermatitis [23, 24], if the allergic event is severe, the treatment is interrupted; benzoyl peroxide produces photosensitization; like retinoids, it is contraindicated in pregnancy [25]. Benzoyl peroxide used alone can relieve inflammatory acne, with antibacterial, anti-inflammatory and keratolytic action [26]. The decomposition of benzoyl peroxide releases oxygen as a by-product. The oxygen suppresses the growth of anaerobic bacteria P. acnes [27]. By hindering bacterial colonization in sebaceous ducts, oxygen markedly reduces bacterial count (even over 95% during 2 weeks).
azelaic acid, as a dicarboxylic acid, has antibacterial, comedolytic and anti-inflammatory properties. It is considered an effective topical treatment for adult patients with acne and for maintenance therapy. A potential adverse effect of azelaic acid is the appearance of hypopigmented lesions, so it can be used in the treatment of post-inflammatory hyperpigmentation [28, 29].
topical antibiotics, erythromycin and clindamycin are most commonly used in the treatment of acne. Erythromycin is used both in reducing inflammatory lesions and in reducing non-inflammatory lesions. After its use for 6 to 12 weeks, a reduction in lesions was observed in 42% to 74% for inflammatory lesions and between 25% and 74% for non-inflammatory lesions [23]. Combined with zinc, erythromycin is much more effective in reducing pustules and papules [30]. Clindamycin is a lincosamide derivative, with antimicrobial action is effective in fighting gram-positive and gram-negative microorganisms, has the following effects – destroys bacteria, disinfects, regenerates cells, cleanses, dries, whitens [31].
the sulfur commonly prescribed by dermatologists in pharmaceutical suspensions is known to be a very good agent in eliminating acne, it helps to absorb chemicals from the skin that are the main cause of acne. Sulfur acne treatment is done by drying excess fat on the skin and controlling sebum [32]. It makes the surface of the skin to peel off. This exfoliation helps to produce new cells, which leads to firmer and smoother skin.
zinc oxide has the ability to act like a mild astringent. It will keep P. acnes from causing infections and acts as a natural skin-drying agent. Thus, zinc oxide on acne-prone skin treatment may help clear acne-causing bacteria and reduce oil production [33].
salicylic acid is a topical medication and is found in a variety of anti-acne, one-component liquid and semi-solid forms and in combined formulations of alpha and beta hydroxy acids [14].
Doctors recommend starting the treatment with low doses of benzoyl peroxide (2.5%) as they have a lower irritant effect compared to higher concentration preparations [34]. Because of the risk of developing bacterial resistance when erythromycin and clindamycin are used as monotherapy, if prescribed, they should be combined with benzoyl peroxide [25].
After evaluation of State Drug Nomenclature of medicines [35] that are registered in the R. of Moldova, we had established that the major share of topical drugs used in acne belongs to domestic manufacturer of pharmaceuticals and that salicylic acid is the most utilized component in anti-acne products registered from different countries. Local pharmaceutical manufacture Farmaprim LTD produce drugs containing chloramphenicol, salicylic acid, sulfur and benzoyl peroxide, as shown in figure 2.
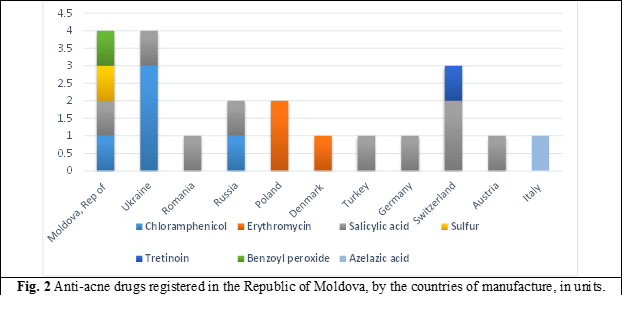
An important direction in anti-acne treatment is emphasized by preparation by compounding pharmaceutical formulations according to medical prescriptions. Dermatologists from various medical institutions from our country prescribe in the treatment of acne magistral or extemporaneous prescriptions for drug preparation in pharmacies as topical formulations containing: salicylic acid, sulfur, chloramphenicol, and others. The evidence-based medication of individual medication maintains the trend for compounding. Pharmacies are still individually responsible for assessing the quality, stability, and effectiveness of every compounded preparation they dispense.
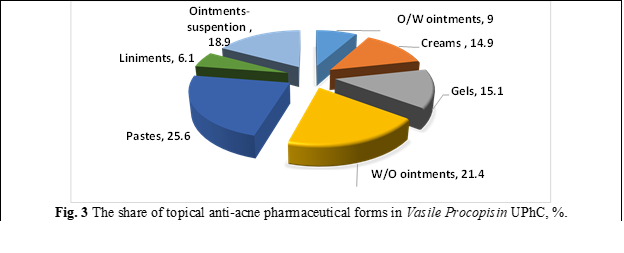
Compounding is an extemporaneous process and a compounded topical anti-acne product, formulated based on individual unique prescription by pharmacists, is more susceptible to physicochemical modifications than manufactured drug products that are made usually by a single drug. Thus, a proper combination of more than one active and inactive ingredients, in consideration of the quality, stability, and effectiveness of compounded preparations, rely on pharmacy technicians. Following the analysis of the prescription from Vasile Procopisin UPhC it was determined that the pharmaceutical forms for topical use (ointments, pastes, gels, ointments-emulsions, ointments-suspensions, creams, etc.) represent 4-6% of the total preparations prescribed by doctors and prepared by pharmacists. Among topical forms that are prepared and released, pastes occupy the largest share – 25.6% (figure 3), followed by ointments with water-oil base – 21.4%, that are considered to have advantages as dermato-cosmetics because after been applied on skin, evaporation occurs and increases the release concentration of the drug that was previously dissolved in water, thus enhancing the API effect and absorption.
Evaluation of prescribed anti-acne API by dermatologists from the R. of Moldova was carried out. Following analysis of the prescriptions, based on the age of the patients, it was found that the most common API indicated in the age groups of 11-16 and 17-21 years (figure 4) is salicylic acid; sulfur is prescribed for both the juvenile segment and the adult group over 29 years of age, including the most common retinol and resorcinol.
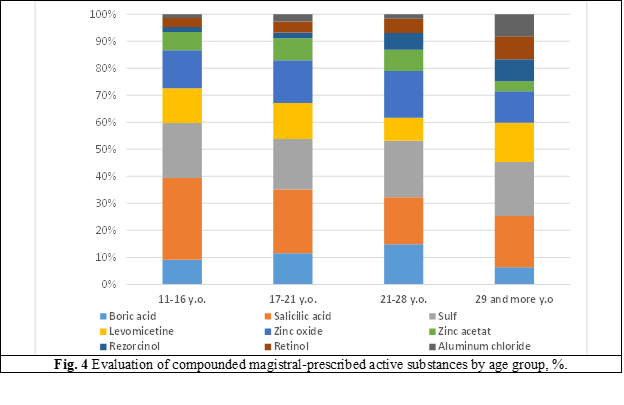
Salicylic acid ointment is prescribed by doctors in a concentration of 1% for magistral formulations. It has a comedolytic effect, but with a lower efficiency than topical retinoids. Sulfur, commonly prescribed by dermatologists in pharmaceutical ointments-suspension, is known to be a very effective agent in eliminating acne because it helps to absorb chemicals from the skin that are the main cause of acne. Sulfur acts on acne on account of keratolytic properties and helps to quickly get rid of dead skin cells that block pores, which causes acne. It also clears comedones and prevents them from forming again. This exfoliation helps to produce new cells, which leads to firmer and smoother skin. The analysis revealed that the treatment of acne in adolescents focuses on combating the causative agent of sebum production, and with increasing age, the aim is to suppress inflammatory processes.
Conclusions
Acne vulgaris is considered a minor clinical problem but has a significant psychosocial impact on the patient's quality of life, leading to psychological stress or depression. Specialists pay attention not only to the physical manifestations of acne, but also to the emotional burdens resulting from the condition.
Currently on the pharmaceutical market there is a wide range of topical industrial forms, favored by salicylic acid. In the production department of Vasile Procopisin UPhC there is a large assortment of anti-acne remedies, with different therapeutically groups of medicinal substances that are prescribed in magistral prescription by dermatologists.
Pharmaceutical compounding of topical anti-acne remedies is opportune for continuous research in pharmaceutical optimization regarding dermato-products perusing an efficient and safety anti-acne pharmacotherapy.
Competing interests
None declared
Authors' contribution
All authors participated equally in the elaboration and writing of the paper. All authors read and approved the final version of the manuscript.
Authors’ ORCID IDs
Adrian Virlan - https://orcid.org/0000-0001-5668-6265
Diana Guranda - https://orcid.org/0000-0001-6296-9114
Cristina Ciobanu - https://orcid.org/0000-0001-6550-6932
References
Yang Z., Zhang Y., Lazic Mosler E., Li H., Hu J., Zhang Y., Liu J., Zhang Q. Topical benzoyl peroxide for acne. Cochrane Database of Systematic Reviews 2014, Issue 6. Art. No.: CD011154. DOI: 10.1002/14651858.CD011154.
- Bagatin, Edileia et al. Adult female acne: a guide to clinical practice. Anais brasileiros de dermatologia vol. 94,1 (2019): 62-75. doi:10.1590/abd1806-4841.20198203.
- Benner N., Sammons D. Osteopathic Family Physician. Overview of the treatment of acne vulgaris. Osteopathic Family Physician. 2013, 5 (5): 185–90. doi:10.1016/j.osfp.2013.03.003.
Simonart T. Immunotherapy for Acne Vulgaris: Current Status and Future Directions. Am J Clin Dermatol. 2013 Dec 1;14(6):429–35.
Titus S., Hodge J. Diagnosis and treatment of acne. Am Fam Physician. 2012 Oct 15;86(8):734–40.
Eichenfield L.F., Draelos Z., Lucky A.W., et al. Preadolescent moderate acne vulgaris: a randomized trial of the efficacy and safety of topical apalenebenzoyl peroxides. J Drugs Dermatol. 2013;12:611-18.
Gonzalez P., Vila R., Cirigliano M. The tolerability profile of clindamycin 1%/ benzoyl peroxide 5% gel vs. adapalene 0.1%/benzoyl peroxide 2.5% gel for facial acne: results of a randomized, single-blind, split-face study. J Cosmet Dermatol 2012;11:251-60. DOI: 10.1111/jocd.12013.
Fox L, Csongradi C, Aucamp M, du Plessis J, Gerber M. Treatment Modalities for Acne. Molecules. 2016 Aug 13;21(8):1063.
- Knutsen-Larson S., Dawson A.L., Dunnick C.A., Dellavalle R.P. Acne vulgaris: pathogenesis, treatment, and needs assessment. Dermatologic Clinics. 2012, 30 (1): 99–106. doi:10.1016/j.det.2011.09.001.
- Practice Guidelines. Acne Vulgaris: Treatment Guidelines from the AAD. J Am Acad Dermatol. May 2016;74(5):945-973.e33. [accessed March 2022].
- Thielitz A., Gollnick H. Topical retinoids in acne vulgaris: update on efficacy and safety. Am J Clin Dermatol. 2008;9(6):369-81. doi: 10.2165/0128071-200809060-00003.
- See J.A., Goh C.L., Hayashi N., Suh D.H., Casintahan F.A. Optimizing the use of topical retinoids in Asian acne patients. J Dermatol. 2018 May;45(5):522-528. doi: 10.1111/1346-8138.14314. Epub 2018 Apr 3. PMID: 29611225; PMCID: PMC5969268.
- Thielitz A., Abdel-Naser M.B., Fluhr J.W., Zouboulis C.C., Gollnick H. Topical retinoids in acne--an evidence-based overview. J Dtsch Dermatol Ges. 2008 Dec;6(12):1023-31. English, German. doi: 10.1111/j.1610-0387.2008.06741.x. Epub 2008 May 13. PMID: 18479477.
- Nedelciuc B., Beţiu M., Guţu A. Acne vulgaris: retrospectives and perspectives. Curierul Medical, nr. 4(56) / 2013 / ISSN 1875-0666, p. 62-65.
Csongradi C., Aucamp M., du Plessis J., Gerber M. Treatment Modalities for Acne. Molecules. 2016 Aug 13;21(8):1063.
Keri J., Shiman M. An update on the management of acne vulgaris. Clinical, Cosmetic and Investigational Dermatology. 2009 Jun;105-10. doi: 10.2147/ccid.s3630.
- Diug E., Guranda D., Ciobanu C. Biofarmacie și farmacocinetică. Compendiu (ediția a II-a). Chișinău: Print Caro, 2019, 156 p.
- Guranda D., Ciobanu C. Rolul substanţelor auxiliare în formularea și dezvoltarea unguentelor magistrale. Revista Farmaceutică a Moldovei, 2021, 47(3), pp. 37-41.
- Guranda D., Solonari R., Ciobanu C., Diug E., Ciobanu N., Vîrlan A. Utilizarea nanotehnologiilor în formularea dermatocosmeticelor. Revista Farmaceutică a Moldovei. 2021, 47(3), pp. 32-36.
- Guranda D., Ciobanu C. Rolul substanţelor auxiliare în formularea și dezvoltarea unguentelor magistrale. Revista Farmaceutică a Moldovei, 2021, 47(3), pp. 37-41.
- Practice Guidelines. Acne Vulgaris: Treatment Guidelines from the AAD. J Am Acad Dermatol. May 2016;74(5):945-973.e33. [accesat March 2022].
- Primary Care Dermatology Society. Acne – Practical Advice and Maintenance. [accessed April 2022] http://www.pcds.org.uk/ee/images/uploads/general/Acne_Treatment_2015-web.pdf.
- Management of acne. Clinical practice guidelines. Ministry of Health Malaysia. [accessed March 2022] https://www.moh.gov.my/moh/attachments/7190.pdf.
- Rallis E., Verros C., Katoulis A., Katsarou A. Topical 5% Benzoyl Peroxide and 3% Erythromycin Gel: Experience with 191 Patients with Papulopustular Acne. Acta Dermatovenerol Croat. 2013;21(3):160-167.
- Pastuszka M., Kaszuba A. Role of topical combination drug containing clindamycin and benzoyl peroxide in the treatment of common acne. Postep Derm Alergol 2012; XXIX, 4: 279–285 DOI: 10.5114/pdia.2012.30468
Titus S., Hodge J. Diagnosis and treatment of acne. Am Fam Physician. 2012 Oct 15;86(8):734–40.
- Ningsih D. R. et al. Synthesis of Anti-Acne Ointment of Ethanol Extract of White Plumeria Leaves (Plumeria Alba L.). IOP Conf. Ser.: Mater. Sci. Eng., 2017, 172 012013. doi:10.1088/1757-899X/172/1/012013.
Clive B. Archer. Atopic dermatitis. Medicine, Volume 45, Issue 6, 2017, pp. 379-382, ISSN 1357-3039. doi. org/10.1016/j.mpmed. 2017.03.001.
- James W.D. Acne. New England Journal of Medicine. 2005, 352 (14): 1463–2. doi:10.1056/NEJMcp033487.
- Feucht C.L., Allen B.S., Chalker D.K., Smith J.G. Jr. Topical erythromycin with zinc in acne. A double-blind controlled study. J Am Acad Dermatol. 1980 Nov;3(5):483-91. doi: 10.1016/s0190-9622(80)80114-9. PMID: 6452464.
- Guay D.R. Topical clindamycin in the management of acne vulgaris. Expert Opin Pharmacother. 2007 Oct;8(15):2625-64. doi: 10.1517/14656566.8.15.2625.
Csongradi C., Aucamp M., du Plessis J., Gerber M.. Treatment Modalities for Acne. Molecules. 2016 Aug 13;21(8):1063.
- Andronachi A., Guranda D., Ciobanu C., Diug E., Solonari R. Study of magistral topical pharmaceutical forms used in the treatment of psoriasis. Materialele Congresului "Congresul consacrat aniversării a 75-a de la fondarea Universității de Stat de Medicină şi Farmacie „Nicolae Testemiţanu”", Chişinău, Moldova, 21-23 octombrie 2020 Pag. 644-644.
- Mills O.H. Jr, Kligman A.M., Pochi P., Comite H. Comparing 2.5%, 5%, and 10% benzoyl peroxide on inflammatory acne vulgaris. Int J Dermatol. 1986 Dec;25(10):664-7. doi: 10.1111/j.1365-4362.1986.tb04534.x. PMID: 2948929.
- State Nomenclature of Drugs of the Republic of Moldova. Online database. [Accessed March 2022]. http://nomenclator.amdm.gov.md/.