Introduction
Textiloma denotes a cotton foreign body or textile matrix remaining inside the patient's body after the end of a surgical procedure. Most commonly, they are diagnosed in the abdominal cavity [1, 2]. The unintentional leaving of gauze sponges in the abdomen following a laparotomy is a rare but serious medical error. Depending on its location and evolution, the remaining foreign body can either undergo aseptic encapsulation, which leads to pseudotumor appearance, or cause a local acute inflammatory response with abscess development [3, 4]. The time interval before detection of textiloma can vary from the immediate postoperative period to decades after surgery. The diagnosis of a textile foreign body is often difficult due to the rarity of the condition, which is usually unexpected by clinicians, possible long-term previous asymptomatic evolution, and nonspecific and imaging findings that are poorly familiar to radiologists [3, 5].
The present study was conducted in two medical institutions: The Institute of Emergency Medicine and Gheorghe Paladi Municipal Clinical Hospital No.1. This study was approved by the Research Ethics Committee of the Nicolae Testemițanu State University of Medicine and Pharmacy, protocol No.48, from February 12, 2020. Data from computed tomography (CT) identified and surgically confirmed cases of abdominal textilomas treated over a 15-year period (2006–2020) were analyzed retrospectively using interviews with surgeons who were willing to disclose those cases of foreign body retention. In some patients, CT scans were performed in private medical centers (“Excellence”, “Magnific”, and the German Diagnostic Center). The study recorded several factors related to patients diagnosed with textiloma, including their demographics, previous surgeries, clinical manifestations, preliminary diagnosis, and examination tools used. The study also looked at the interval between the causal procedure and textiloma diagnosis, the type of surgical intervention, the location of the foreign body, and the disease's further evolution.
The study emphasized cases with detailed CT images, which were reconstructed in 3D using thin sections (1 mm) in coronal and sagittal planes to provide a better understanding of the lesion's extent and involvement of adjacent structures. While the data and results of X-rays and abdominal ultrasonography (US) were also considered, the study focused on the clinical significance of CT images.
Thirteen cases of abdominal textiloma were included in our study. Table 1 provides a summary of the patients' characteristics, which showed that 10 of the patients were women (76.9%) and 3 were men (23.1%). The average age of the patients was 38.5±4.7 years, with a range of 20 to 74 years.
Of the 13 cases, 7 patients (53.8%) underwent a primary surgical procedure due to general surgical conditions, while 6 patients (46.1%) underwent obstetric or gynecological surgeries. The average interval between the previous procedure and the diagnosis of textiloma using CT was 25.3±15.2 months, ranging from 1 day to 16 years.
Case 1. A 29-year-old woman underwent a caesarean section. She returned 3 weeks later with abdominal pain and a clearly palpable mass in the right part of the abdomen. On the native CT scan, a well-defined hyperdense mass measuring 85x70x65 mm was revealed in the mesogastric area, slightly to the right of midline, with numerous small gaseous inclusions (Figure 1). A repeat open surgery was performed with the simple retrieval of a textiloma (gauze sponge). There was no involvement of the surrounding organs. Postoperative evolution was favorable.
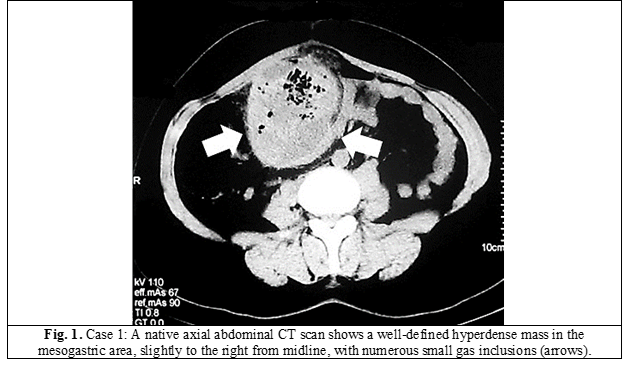
Table 1. Clinical and radiological characteristics of patients with abdominal textiloma. | |||||
No. | Sex, age (years) | Previous surgery | Interval from surgery | Preliminary diagnosis | Location and size of the textiloma on CT |
1 | F, 29 | Cesarean section | 24 days | Infected hematoma | Right mesogastric area; 85х70х65 mm* |
2 | F, 28 | Incisional hernia repair | 5 months | Abdominal mass (textiloma) | Midline pelvis; 37x43x60 mm |
3 | M, 52 | Inguinal hernia repair | 5,5 years | Retroperitoneal cyst | Right iliac area; 40x35x35 mm |
4 | F, 27 | Drainage of postpartum parametrial hematoma | 5 days | Interintestinal hematoma (textiloma) | Left mesogastric area; 88х108х120 mm |
5 | F, 26 | Ruptured ectopic pregnancy | 2 months | Abdominal abscess | Left iliac area; 85x115x95 mm |
6 | F, 32 | Ruptured ectopic pregnancy | 6 months | Abdominal abscess (textiloma) | Right subhepatic space; 72x98x74 mm |
7 | F, 24 | Left hemicolectomy | 2,5 months | Intestinal obstruction | Right mesogastric area; 35х36х68 mm† |
8 | F, 20 | Spleno-renal shunt | 16 years | Ovarian dermoid cyst | Left iliac area; 50x46x52 mm |
9 | F, 74 | Oversewing of the bleeding duodenal ulcer | 3 months | Chronic purulent fistula (textiloma) | Right mesogastric area; 58х69х95 mm |
10 | F, 26 | Cesarean section | 1 day | Foreign body (textiloma) | Right hypogastric area; 40x73x124 mm |
11 | F, 45 | Total hysterectomy | 4 years | Abdominal mass (textiloma) | Left pelvis; 43x65x50 mm |
12 | M, 57 | Distal partial gastrectomy | 16 days | Subhepatic abscess (textiloma) | Midline epigastrium; 60x117x51 mm |
13 | M, 60 | Hartmann’s procedure | 16 days | Abdominal abscess (textiloma) | Left subphrenic space; 109x85x125 mm |
Note: * – the textiloma sizes are presented in the following order: anteroposterior x lateral x vertical; † – the only case of complete intraluminal migration of textiloma and its localization inside the jejunal loop. | |||||
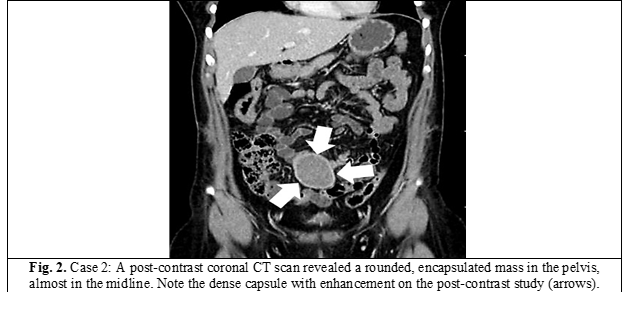
Case 2. A 28-year-old female patient had an incisional abdominal hernia after a lower median laparotomy. Somewhere around 5 months after hernia repair with a synthetic mesh, she developed vague abdominal pain, anorexia, and constipation. In prehospital conditions, US and multidetector contrast CT scans were sequentially performed. On the latter, in the pelvis almost along the midline, a rounded, encapsulated mass measuring 37x43x60 mm with a few air bubbles inside is visualized. The capsule is dense, reaches a thickness of 4 mm, and showed significant enhancement on post-contrast study (Figure 2). Abdominal textiloma was suspected, and the patient was admitted for redo surgery. The foreign body (gauze sponge) was removed via laparotomy. An uncomplicated recovery followed. No pathological clinical events were noted during the patient’s 1-year follow-up.
Case 3. A 52-year-old man underwent inguinal hernia repair using local tissues. After the surgery, the patient remained asymptomatic without any complaints. However, during a follow-up ultrasound examination 5.5 years later, a cystic abdominal mass was discovered. A CT scan was recommended, revealing a well-defined, rounded formation measuring 40x35x35 mm in size with inhomogeneous density in the right iliac area. The patient underwent an elective open surgery, during which an elastic mass, unrelated to surrounding organs, was removed. Upon gross pathological examination of the specimen, a non-degraded gauze swab was found. The patient's postoperative period was uneventful.
Case 4. A 27-year-old woman who underwent a physiological delivery experienced a ruptured cervix, vaginal and parametric hematomas, and intra-abdominal bleeding. A median laparotomy was performed on the following day to address the hematoma and ensure hemostasis. The patient experienced severe abdominal pain, bloating, lack of peristalsis, and signs of intra-abdominal infection during the early postoperative period. Plain radiography and repeated transabdominal ultrasounds were inconclusive. Five days after the primary surgery, a CT scan was conducted, revealing a heterogeneous mass with air bubbles and encysted liquid measuring 88x108x120 mm in the left mesogastric area. Subsequent relaparotomy uncovered a textiloma (a large surgical gauze pad) that was removed. The postoperative course was normal, with wound healing achieved through primary intention.
Case 5. A 26-year-old woman underwent surgery for an ectopic pregnancy with intra-abdominal bleeding and a subsequent tubectomy. Two months later, she was urgently admitted to the surgical department with severe pain in the left iliac fossa, asthenia, and fever. A painful, elastic mass was palpated in the left lower abdomen. An abdominal CT revealed a well-defined oval structure measuring 85x115x95 mm with predominantly air content in the left iliac region, covered with a dense capsule up to 10-15 mm thick. The patient underwent relaparotomy with suspicion of a late postoperative abscess. A foreign body (gauze sponge) was found inside the cavity formed by the omentum and sigmoid colon. The textiloma was removed, and the infected cavity was debrided and drained. However, a large bowel fistula appeared during the postoperative period. Although the fistula eventually closed spontaneously following conservative treatment, the patient's hospital stays lasted 46 days.
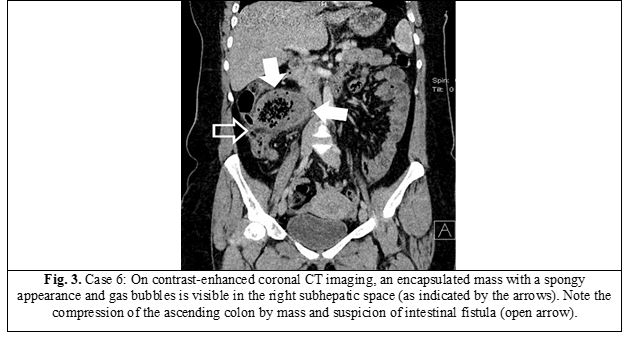
Case 6. A 32-year-old woman presented with sudden and progressively worsening abdominal pain and impaired intestinal passage six months after undergoing a midline laparotomy and tubectomy for an ectopic pregnancy. Despite receiving conservative treatment, the patient's symptoms did not improve, and she sought urgent care at the surgical department. Upon physical examination, her abdomen was swollen, diffuse tender and resistant. Ultrasound imaging showed an isoechoic lesion in the upper right abdomen with an incomplete hyperechoic peripheral wall. An emergent CT scan revealed a 72x98x74 mm encapsulated mass with a cellular pattern and gas bubbles in the right subhepatic space. The mass was also compressing the ascending colon, and the radiologist suspected the presence of an intestinal fistula (as shown in Figure 3). During an emergency relaparotomy, surgeons discovered a foreign object – a gauze sponge soaked in intestinal contents – within the abdominal cavity, causing erosion of the bowel wall. The defect in the ascending colon was primarily closed, and the patient experienced an uneventful postoperative recovery. She was discharged after 15 days.
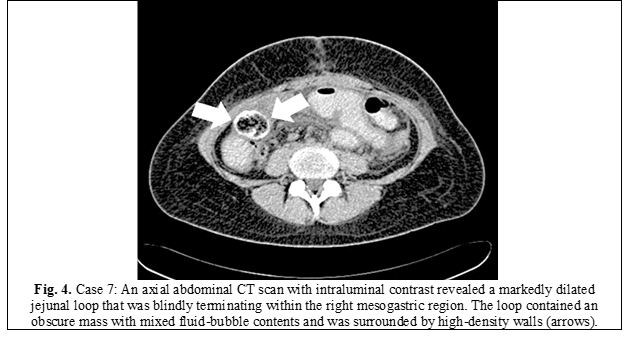
Case 7. A 24-year-old woman was urgently admitted to the surgical department with intermittent diffuse abdominal pain, nausea, and repeated vomiting. Physical examination revealed moderate abdominal distension but no tenderness or peritoneal irritation. Two and a half months before she underwent a left-sided colectomy for dolichocolon and chronic constipation syndrome. Abdominal CT with intraluminal contrast revealed a marked distention of the proximal jejunal loops, as well as a blindly terminating loop of the small bowel within the right mesogastric area with a diameter of up to 5 cm, containing a mass measuring 35x36x68 mm in size with mixed liquid and air bubble contents, surrounded by heterogeneous high-density walls (up to +200 Hounsfield units) (Figure 4). The radiologist identified the mass as an accumulation of barium caused by an incomplete intestinal obstruction. The patient underwent surgery with suspicion of adhesive intestinal obstruction. During laparotomy, numerous dense adhesions were observed between the dilated jejunal loop and anterior abdominal wall, located about 100 cm from the Treitz ligament. While separating the adhesions, the foreign body (a crumpled surgical sponge) was found and removed from the lumen, which had caused the obstruction. After partially resecting the damaged segment, intestinal continuity was restored by an end-to-end anastomosis. The postoperative period was complicated by a deep surgical site infection and a subcutaneous evisceration. The patient stayed in the hospital for 30 days.
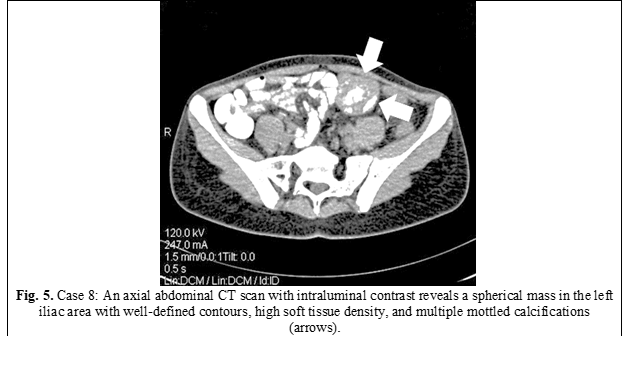
Case 8. A 20-year-old woman was electively admitted to the hospital. Sixteen years ago, at the age of 4, she underwent spleno-renal shunting for prehepatic portal hypertension and bleeding from dilated esophageal varices. An outpatient CT scan with intraluminal contrast revealed a spherical mass in the left iliac region measuring 50x46x46 mm with well-defined contours and high soft tissue density (+46 Hounsfield units), but with hypodense areas (+16 Hounsfield units) and multiple mottled calcifications (Figure 5). The patient was asymptomatic. During laparotomy, a round, tumor-like mass of densely elastic consistency that closely adhered to the small intestine loop was found. The mass was removed without damaging the surrounding organs. A gauze pad was found inside the pseudotumor on gross specimen cutting. The postoperative period was uncomplicated.
Case 9. A 74-year-old woman underwent duodenotomy and hemostatic oversewing of a duodenal ulcer due to recurrent bleeding. In the postoperative period, a chronic purulent fistula opened in the scar after midline laparotomy, without any tendency to close over the next 3 months. An X-ray contrast study of the fistulous canal revealed a large intra-abdominal cavity with amorphous content. On CT, an inhomogeneous, oval-shaped mass measuring 58x69x95 mm with multiple gas inclusions was visualized in the right mesogastric area, surrounded by a capsule up to 6 mm thick. A diagnosis of a retained surgical sponge (textiloma) was made, which was confirmed during a subsequent laparotomy where the gauze sponge was removed. The postoperative course was uneventful.
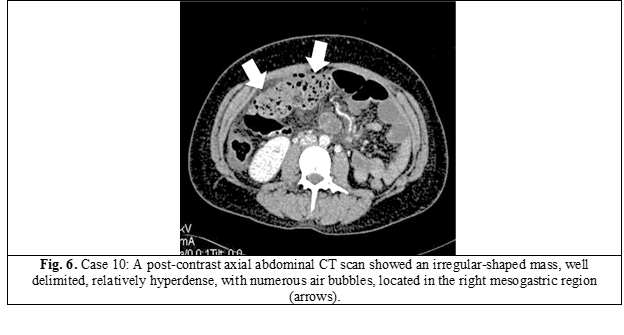
Case 10. A 26-year-old woman at 28-29 weeks of pregnancy was urgently hospitalized for premature detachment of the placenta, and an emergency cesarean section was performed. The next day, due to the patient's poor condition and severe abdominal pain, there was suspicion of intra-abdominal bleeding from spontaneous rupture of the spleen. Abdominal ultrasound and CT scans were performed sequentially. On the CT scan, an irregular-shaped mass, relatively hyperdense, with numerous air bubbles, well delimited from surrounding tissues, measuring 40x73x124 mm was identified in the right mesogastric region (see Figure 6). The radiologist described the findings as a residual textile foreign body in the abdominal cavity, likely a retained surgical sponge. An urgent laparotomy was performed, and the gauze sponge was retrieved. The postoperative period was uneventful.
Case 11. A 45-year-old woman who underwent total hysterectomy 4 years ago presented with moderate abdominal pain. Physical examination revealed a palpable mass in the left suprapubic area. A CT scan of the pelvis revealed a solid mass measuring 43 x 65 x 50 mm with a high density capsule enhancement in the post-contrast phase located to the left of midline. The diagnosis of textiloma (surgical gauze sponge) was made, and elective surgery was performed to remove the mass along with a fragment of a covering omentum. The postoperative period was uneventful.
Case 12. A 57-year-old man had a long-standing duodenal ulcer and presented with marked gastric outlet stenosis. In the early postoperative period following a Billroth-I distal partial gastrectomy, the patient developed progressive signs of abdominal infection: tenderness in the upper abdomen, muscular resistance, peritoneal signs, high fever, and leukocytosis. Abdominal ultrasound showed a well-defined multiseptated fluid collection measuring 75x32x70 mm. CT scan with intravenous contrast revealed a typical “spongiform” structure of 60x117x51 mm, with areas of fluid and entrapped small gas bubbles, located in the epigastrium, in the projection of the omental bursa. The diagnosis of textiloma was not in doubt and was based on the patient's previous surgical history and imaging findings. A surgical gauze sponge was removed through a limited laparotomy on the 16th day after the initial surgical intervention. However, later on, the patient was diagnosed with an abscess in the same area, caused by infected pancreatic necrosis and a gastroduodenal anastomosis fistula. Intensive conservative tratment resulted in a gradual improvement and spontaneous closure of the fistula. However, the patient's hospital stay lasted for a total of 73 days.
Case 13. A 60-year-old man had emergent surgery for acute large bowel obstruction due to an occlusive tumor of the sigmoid colon. He underwent the resection of the sigmoid colon and a terminal colostomy (Hartmann's procedure). The early postoperative period was complicated by diffuse abdominal pain, intestinal paresis, and high fever. Abdominal US was inconclusive, although it suggested an abscess. On CT scan, in the left upper abdomen, a slightly encapsulated mass with a spongiform pattern and multiple gas bubbles inside, measuring 109x85x125 mm in size, is visualized, along with infiltrative changes in adjacent tissues. Thus, 16 days after the primary procedure, a relaparotomy was performed with the removal of a foreign body (gauze sponge). There was a rapid disappearance of the pathological symptoms, and after 4 days he was discharged.
Results
Among the patients included in our study, the primary surgery was performed for urgent indications in 7 (53.8%) cases and in 6 (46.1%) cases on an elective basis. Females made up the vast majority—76.9%. During the analysis of case histories, other possible causes that could explain the unintentional leaving of textile foreign bodies in the abdominal cavity were also established, but they were not the purpose of this study and are not presented here. Only two patients had no pathological symptoms at the time of their textiloma diagnosis. The remaining 11 (84.6%) patients were symptomatic, with abdominal pain and a palpable mass being the most common manifestations.
Plain abdominal radiography and/or contrasted intestinal studies were performed in 9 cases, mainly to confirm or rule out the diagnosis of intestinal obstruction. The lesions did not show a definite pattern on radiographs, and in relation to textilomas, the studies were unremarkable. In only one patient (Case No.4), the radiologist noted an extensive area of homogeneous opacity that displaced bowel loops. In another patient (Case No.7), only a retrospective analysis of a contrast series made it possible to visualize an intraluminal textiloma as an oval structure covered with a barium mass. Finally, in case No.9, the X-ray contrast of a chronic purulent fistula opening in the postoperative scar suggested the presence of an abdominal foreign body.
Ultrasound scanning of the abdominal cavity was performed in 12 patients, except for one case with intestinal obstruction. In some cases, multiple scans were conducted. The presence of an intra-abdominal mass with a typical pattern of ultrasound visualization for textilomas was found in half of the cases (6 patients), which was characterized as a thick-walled hypoechoic mass with strong posterior acoustic shadowing. In four cases, the foreign body was characterized by the radiologist as an abscess, and in two more cases it turned out to be uninformative. However, abdominal ultrasound was not the ultimate diagnostic tool for determining indications for repeated surgery in any of the cases included in our series.
According to the CT results, a textiloma was found in the upper abdomen cavity, including the subphrenic and subhepatic spaces, in three cases; at the mesogastric level, in four cases; in the left and right iliac fossa, in three cases; and in the pelvic cavity, in three cases. The median size of the textiloma was 61x72x77 mm (anteroposterior x lateral x vertical length). The minimal volume of the lesion was 40x35x35 mm, and the maximal was 109x85x125 mm. In the majority of cases (n = 12), the lesion had a clearly defined oval or rounded shape. Only in patient No.10, who had less than 24 hours from the surgical intervention to the discovery of the foreign body, did the pathological mass appear to have an irregular shape. In eight cases (61.5%), the mass had a typical spongiform structure with numerous small air bubbles and was surrounded by a thin capsule. In the other four patients (30.8%), a high-density, well-circumscribed lesion was visualized without any air component inside, but sometimes with mottled calcification and a dense capsule with intense contrast accumulation. It is noteworthy that the interval from causal surgery until the diagnosis of textiloma was 1.71±0.6 months in the “spongiform structure” group, while in the “solid mass” group, it was 78.3±40.8 months. One patient (Case No.7) had an atypical CT scan presentation of a textile pad mimicking a barium mass in a small bowel loop and was diagnosed only during surgery.
Based on surgical history, physical examination, and CT scan findings, a likely diagnosis of textiloma was made before surgery in 11 of 13 cases (84.6%). In all patients, a repeated laparotomy was necessary to remove the textile foreign bodies. In most cases (n = 11), surgery was limited to simple gauze sponge retrieval, but in the other two cases, more complex reconstructive procedures were required, including segmental resection of the jejunal loop with end-to-end anastomosis (Case No.7) and closure of the ascending colon fistula (Case No.6). However, severe complications occurred in the early postoperative period in cases No.5, 7, and 12. These complications included sigmoid colon fistula, subcutaneous evisceration, and gastroduodenal anastomosis leak, respectively, which required intensive conservative treatment and resulted in a prolonged hospital stay.
Discussion
Textiloma is a medical condition defined as a textile foreign body that has been inadvertently left within the patient and is discovered at any time after the patient exits the operating room [6]. The term “textiloma” is derived from “textilis” (tissue, cotton) in Latin and “oma” (tumor, edema) in Greek [7]. Other definitions of the condition in the medical literature include “gossypiboma”, “gauzoma”, “muslinoma”, “cottonoid”, and “cottonballoma” [1, 8, 9]. Retained foreign bodies belong to the category of “never events”, which are caused only by human error and should not occur as they are easily preventable. However, if they do occur, they can lead to tragic consequences for the patient, causing increased morbidity and even mortality [4, 8].
Gauze sponges and pads are the most commonly left objects in patients' cavities and tissues due to their universal use during all surgical procedures, relatively small size, and amorphous structure, especially when they soak up and become saturated with blood and other liquids [1, 5]. Most often, textilomas were found in the abdominal cavity, a fact explained by the complexity of its anatomy and its large volume [1, 2]. The incidence of abdominal textilomas is not known, and most publications are limited to reports of single cases or small series, due to possible legal and/or reputational implications for the hospital and surgeons involved [2]. However, according to the most reliable data, the incidence of abdominal textiloma is estimated to range from 1 in 1,000 to 1 in 1,500 for intra-abdominal operations [10, 11].
Any foreign object elicits a reaction in the human body [9]. The manifestations of this reaction, as well as the natural evolution of foreign textile items unintentionally left in the human body after surgery, are variable and depend on the item's location, composition, grade of bacterial contamination, and the individual host's response. Patients with textiloma can have two main types of foreign body reactions [3, 4, 7]. The most common is an aseptic fibrous inflammatory reaction and adhesion that encapsulates the textile item in the omentum and surrounding organs. These patients usually remain asymptomatic and are discovered incidentally, as happened in cases No.3 and 8 in our series, or have very limited and non-specific symptoms, dominated by general malaise, vague pain, and sometimes a palpable abdominal mass (cases No.1, 2, 5, and 11). The second known reaction is of the exudative-inflammatory type, which leads to the formation of an abscess or purulent fistula. This reaction usually manifests acutely, in the early postoperative period or much earlier than the fibrinous reaction [12], in the form of persistent inflammation and local septic complications (cases No.4, 9, 12, and 13). The most threatening evolution of textiloma is associated with the gradual erosion of the bowel wall due to a combination of mechanical pressure and localized inflammation. The final part of this process is the bowel wall destruction, with partial or complete migration of the gauze sponge into the intestinal lumen. In our series, colonic fistula development was documented in two cases (No.5 and 6). However, in patient No.7, the textiloma completely migrated into the jejunal lumen, causing acute intestinal obstruction.
In any case, clinical signs are often nonspecific, and the possibility that a foreign body was left behind is rarely considered when assessing the postoperative course, particularly in the early stages. Therefore, imaging studies play a decisive role in making a timely diagnosis. Conventional radiography is the standard method for the initial diagnosis of acute abdominal abnormalities, including the detection of remaining sponges [13]. The exam is especially effective if the gauze sponge has a radiopaque marker, which is in line with universal surgical recommendations [1, 14]. Unfortunately, the use of radiopaque markers on surgical sponges is inconsistent in the Republic of Moldova. In our series of thirteen patients, all of whom had their primary surgeries in different hospitals across the country, none of the surgical sponges had a radiopaque marker. This made it difficult to visualize them during imaging studies. In some cases, a plain abdominal X-ray may reveal a faint soft tissue density with mottled lucencies due to trapped air or abscess formation. While this finding may raise suspicion, it cannot confirm the diagnosis of textiloma with certainty [4].
On abdominal ultrasound, textilomas typically appear as well-defined masses that can be either cystic or solid. Ultrasound features typically include a wavy internal echogenic source with a hypoechoic rim and a dense posterior shadow [4, 13, 15]. Posterior acoustic shadowing is the most characteristic sonographic feature of textilomas and may result from the retained sponge or from areas of calcification or air within the mass [13, 15]. However, ultrasonography has some limitations, such as operator dependence, difficulty identifying foreign bodies at greater depths or located posteriorly to a gas-containing hollow viscus, and the possibility of presenting false-positive results in cases where scars and calcifications of other etiologies are present [13]. Of the 13 patients in our series, only 2 ultrasound scans were completely uninformative. In the remaining patients, a “volume mass’ was visualized or an “abdominal abscess” was suspected. However, in no case did the examiner definitively identify the lesion as a “retained foreign body.” This could be because radiologists may not receive adequate training or have enough experience in recognizing surgical sponges, and therefore may lack complete information about what these objects might look like. As a result, the abdominal ultrasound data in our study were inconclusive and only indicative and could not be used to justify a diagnosis or further therapeutic measures. Additionally, ultrasound scanning was not able to provide information on the anatomical relationships of the textiloma.
In cases of abdominal textiloma, a CT scan may be indicated in the presence of indeterminate or non-specific clinical manifestations, or in the presence of predisposing findings from previous examinations. On CT, the most characteristic feature of a textiloma is a heterogeneous, low-density cystic lesion with a typical spongiform pattern resulting from trapped gas bubbles, surrounded by a thin, high-density capsule that exhibits marked enhancement after contrast administration [4, 12, 16]. In chronic cases, the gas bubbles within the retained gauze piece are gradually absorbed, and the textiloma acquires the visual characteristics of a round or oval soft-tissue-density mass with a thick capsule, strong wall enhancement, and calcifications [15]. The latter is often defined as a so-called “calcified reticulate rind” sign, which is probably formed by gradual deposition of calcification along the fiber network of the surgical gauze [17]. In our study, we observed both acute and chronic CT appearances of textiloma, with these features closely related to the disease duration. The acute form was typically detected after an average of two months, while the chronic form was found after an average of 78 months. Importantly, in all cases, regardless of the clinical manifestations and duration of the disease, CT scanning was the decisive imaging method, allowing for the identification of a mass related to a foreign body and the establishment of an accurate diagnosis of textiloma, including its anatomical location, the presence of possible complications, and the need for repeated surgical intervention.
Once a textiloma is diagnosed, surgical removal should be performed even if the patient is asymptomatic to prevent potential complications that could lead to a high mortality rate [2, 4, 8]. In our series, most patients were symptomatic, and all cases of textiloma were surgically removed through open laparotomy. While most surgeries were technically simple and involved only the retrieval of the foreign body, two patients required more complex reconstructive procedures. Furthermore, the postoperative course was challenging for three patients, requiring prolonged hospitalization. However, all of these repeated surgeries could have been easily avoided with timely detection and removal of the retained sponges.
Undoubtedly, prevention is the best treatment modality for textile foreign bodies forgotten in the abdominal cavity. Many systems and safeguards are applied in the operating room to ensure that no material is left behind unintentionally after closure [1, 2]. The most common recommendations include creating a well-organized operating room with minimal distractions, ensuring optimal communication among the surgical team and support staff, and strictly adhering to patient safety measures, which are maintained by carefully, consistently, and informally following all the rules of the “Surgical Safety Checklist” developed by the World Health Organization in 2009 [14]. Counting items at the time of surgery is the most widely used method for the screening of textile surgical objects, with established protocols in place. In fact, the process by which counts are performed is not standardized and is often modified according to individual hospital policies. At the end of 2022, the Ministry of Health of Moldova approved the National Guidelines for “Safety of Surgical Patient in the Operating Room”, which, among other things, provides clear recommendations on standard rules for counting gauze sponges and other surgical objects during surgery [18]. It provides four separate counts during each operative procedure: (1) before surgery begins; (2) before closure of any hollow organ; (3) before closure of a laparotomic wound; and (4) during suturing or closure of the skin. In addition, the movement of all surgical objects and instruments should be closely monitored throughout the operation, and the surgeon should carefully explore the abdominal cavity for foreign bodies, regardless of the final count results. In accordance with international standards, the Guidelines strongly recommend the use of only surgical textile materials with an incorporated radiopaque marker in open body cavities [14, 18]. Of course, the latter measure does not prevent inadvertently leaving gauze sponges in the abdominal cavity, but in cases of inconsistency in their count before closure, intraoperative radiography of the entire surgical field makes it easy to identify the lost object.
Conclusions
Our study showed that despite increased attention to patient safety, textiloma is still encountered in daily surgical practice. The possibility of an abdominal textiloma should be considered in the differential diagnosis of any postoperative patient who presents with pain, infection, or a palpable mass.
The CT scan is a practical and highly sensitive diagnostic tool for detecting abdominal textilomas with characteristic imaging features in both chronic encapsulated and acute inflammatory manifestations.
Prevention of abdominal textiloma can be achieved with increased vigilance and strict adherence to preventive measures and strategies in the operating room, aimed at a careful count of sponges and instruments as well as thorough cavity exploration.
Competing interests
None declared.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Authors’ contributions
Concept and design of study – SG, IrC; acquiring of data – OG, DZ, IuC, ID; analysis and/or interpretation of data – SG, IrC, OG, DZ, IuC, ID; drafting the manuscript – SG, IrC; revising the manuscript critically for important intellectual content – SG, IrC. All authors have read and approved the final version of the manuscript.
Author’s ORCID ID
Serghei Guțu – https://orcid.org/0000-0001-9583-0485
Irina Cuţitari – https://orcid.org/0000-0001-6108-6889
Olga Gurschi – https://orcid.org/0009-0001-9956-0619
Diana Zagadailov – https://orcid.org/0009-0006-6981-7002
Iuvenalii Coșulinschii – https://orcid.org/0009-0002-4267-5471
Igor Donțu – https://orcid.org/0009-0008-3938-1169
References
Wan W, Le T, Riskin L, Macario A. Improving safety in the operating room: a systematic literature review of retained surgical sponges. Curr Opin Anaesthesiol. 2009 Apr;22(2):207-14. doi: 10.1097/ACO.0b013e328324f82d.
Stawicki SP, Evans DC, Cipolla J, Seamon MJ, Lukaszczyk JJ, Prosciak MP, Torigian DA, Doraiswamy VA, Yazzie NP, Gunter OLJr, Steinberg SM. Retained surgical foreign bodies: a comprehensive review of risks and preventive strategies. Scand J Surg. 2009;98(1):8-17. doi: 10.1177/145749690909800103.
Rajput A, Loud PA, Gibbs JF, Kraybill WG. Diagnostic challenges in patients with tumors: case 1. Gossypiboma (foreign body) manifesting 30 years after laparotomy. J Clin Oncol. 2003 Oct 1;21(19):3700-1. doi: 10.1200/JCO.2003.02.092.
Tandon A, Bhargava SK, Gupta A, Bhatt S. Spontaneous transmural migration of retained surgical textile into both small and large bowel: a rare cause of intestinal obstruction. Br J Radiol. 2009 Apr;82(976):e72-5. doi: 10.1259/bjr/32683906.
Gibbs VC, Coakley FD, Reines HD. Preventable errors in the operating room: retained foreign bodies after surgery. Part I. Curr Probl Surg. 2007 May;44(5):281-337. doi: 10.1067/j.cpsurg.2007.03.002.
Cima RR, Kollengode A, Garnatz J, Storsveen A, Weisbrod C, Deschamps C. Incidence and characteristics of potential and actual retained foreign object events in surgical patients. J Am Coll Surg. 2008 Jul;207(1):80-7. doi: 10.1016/j.jamcollsurg.2007.12.047.
Andronic D, Lupaşcu C, Târcoveanu E, Georgescu S. Corpi străini textili restanţi postoperator [Foreign textile bodies retained after surgery]. Chirurgia. 2010;105(6):767-77. Romanian.
Garg M, Aggarwa MG. A review of medicolegal consequences of gossypiboma. J Indian Acad Forensic Med. 2010;32(4):358-361.
Kumar GVS, Ramani S, Mahajan A, Jain N, Sequeira R, Thakur M. Imaging of retained surgical items: a pictorial review including new innovations. Indian J Radiol Imaging. 2017 Jul-Sep;27(3):354-361. doi: 10.4103/ijri.IJRI_31_17.
Gawande AA, Studdert DM, Orav EJ, Brennan TA, Zinner MJ. Risk factors for retained instruments and sponges after surgery. N Engl J Med. 2003 Jan 16;348(3):229-35. doi: 10.1056/NEJMsa021721.
Lincourt AE, Harrell A, Cristiano J, Sechrist C, Kercher K, Heniford BT. Retained foreign bodies after surgery. J Surg Res. 2007 Apr;138(2):170-4. doi: 10.1016/j.jss.2006.08.001.
Cheng TC, Chou AS, Jeng CM, Chang PY, Lee CC. Computed tomography findings of gossypiboma. J Chin Med Assoc. 2007 Dec;70(12):565-9. doi: 10.1016/S1726-4901(08)70063-7.
Chagas Neto FA, Agnollitto PM, Mauad FM, Barreto ARF, Muglia VF, Elias JJr. Imaging findings ao abdominal gossypibomas. Radiol Bras. 2012 Jan/Feb;45(1):53-58. doi: 10.1590/S0100-39842012000100012.
World Health Organization. WHO Guidelines for Safe Surgery 2009: Safe surgery saves lives [Internet]. Geneva: WHO; 2009 [cited 2023 Feb 28]. Available from: https://www.who.int/teams/integrated-health-services/patient-safety/research/safe-surgery.
Manzella A, Filho PB, Albuquerque E, Farias F, Kaercher J. Imaging of gossypibomas: pictorial review. Am J Roentgenol. 2009 Dec;193(6 Suppl):S94-101. doi: 10.2214/AJR.07.7132.
Mathew RP, Thomas B, Basti RS, Suresh HB. Gossypibomas, a surgeon's nightmare-patient demographics, risk factors, imaging and how we can prevent it. Br J Radiol. 2017 Feb;90(1070):20160761. doi: 10.1259/bjr.20160761.
Ministry of Health of the Republic of Moldova; Gutu E, Casian D, Guzun V, et al. Siguranţa chirurgicală a pacientului în sala de operație: Ghid naţional [Safety of surgical patient in the operating room: National guide] [ Internet]. Chișinău: The Ministry; 2022. Romanian [cited 2023 Feb 28]. Available from: https://ms.gov.md/wp-content/uploads/2023/01/Ghid-national-Siguran%C5%A….

