Introduction
The treatment of degenerative spinal instability in patients with severe osteoporosis remains controversial because of frequent instrument failure and the high rate of symptomatic pseudarthrosis. Pedicle screw loosening is correlated with an increase in back pain, leading to high disability and poor quality of life for patients. Cortical bone trajectory (CBT) screw fixation is considered a potential option for patients with osteoporosis undergoing lumbar fusion. The novel method of CBT screw fixation was introduced in 2009 by Santoni et al. [1]. The proposed trajectory offered the benefit of maximized thread contact with the zone of higher bone density in the pars interarticularis region, which is mostly spared by the osteoporotic disease process. The aims of this track were to improve the anchoring of the screws in osteoporotic vertebrae and to prevent instrumentation failure. However, the efficacy of CBT fixation in osteoporosis patients has not yet been proven.
Materials and methods
Detailed anamnesis of disease development and postoperative course, thorough clinical and neurological examination, patient self-reported outcome measures (pain VAS, ODI, SF-12), preoperative and postoperative bone-window CT of the spine with three-dimensional reconstructions for interbody fusion status assessment, vertebral bone mineral density assessment by DEXA (dual X-ray absorptiometry) scan, vertebral bone density measurement in Hounsfield units by computer tomography, and the review of published literature were analysed.
Results
We report the clinical case of a patient who underwent spinal stabilization surgery that failed due to poor vertebral bone quality, although preoperative tests showed adequate bone density. Considering the unusual postoperative course and the failure of the applied treatment, it was decided to analyse the patient's clinical and imaging data repeatedly with the application of new alternative bone density assessment methods. The literature reporting similar complications was also reviewed.
Clinical case
A 67-year-old woman was admitted to the neurosurgery ward of the Timofei Mosneaga Republican Clinical Hospital of Moldova with complaints of severe low back pain (VAS = 9/10) with irradiation in both lower limbs, predominantly in the left leg, without evident motor deficit. The patient has been suffering from low back pain for about 2 years. She has tried multiple treatment regimens, including complex physiotherapeutic and rehabilitation treatment, with only modest pain relief. The functional status was assessed using the Oswestry Disability Index, which corresponded to a state of crippled patient (ODI = 67%).
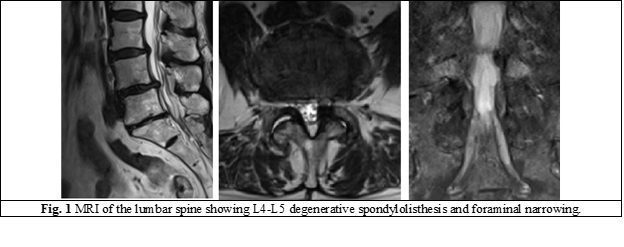
The patient underwent a lumbar spine MRI scan, which revealed the presence of a low-grade degenerative spondylolisthesis at the L4-L5 level, as well as bilateral foraminal stenosis, particularly narrow on the left side (Fig. 1).
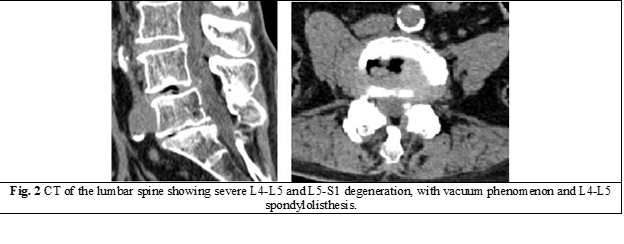
Computed tomography demonstrated the presence of L4-L5 severe degeneration, with intradiscal vacuum phenomenon, facet joint deformity and hypertrophy, and left side foraminal narrowing due to a bony spur (Fig. 2).
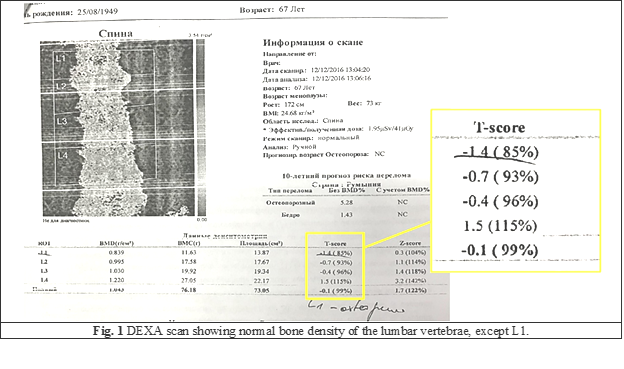
The patient's vertebral bone density was assessed using dual x-ray absorptiometry (DEXA) scan, which demonstrated normal density of the lumbar vertebras. DEXA T-score was greater than -1 in all lumbar vertebrae except L1, which had a score of -1.4, corresponding to osteopenia (Fig. 3).
Treatment
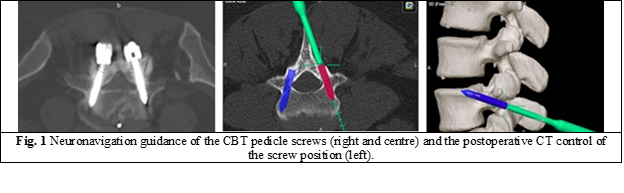
Considering the association of symptomatic foraminal stenosis with degenerative spondylolisthesis and normal bone density of the lumbar vertebrae, indications for interbody arthrodesis were established. It was decided to apply the minimally invasive technique of midline lumbar interbody fusion (MIDLIF) with neuronavigation-guided CBT screws. This procedure involves the insertion of CBT pedicle screws and intervertebral cages through a limited medial exposure, similar to the laminectomy approach.
The procedure was done under general anaesthesia, with the patient being placed in the prone position. The level to be fused was identified using fluoroscopy. After a dose of antibiotics 30 minutes before the operation, a 5 cm posterior midline skin incision was made. The subperiosteal muscle dissection was limited to the lateral side of the pars interarticularis and facet joints. The neuronavigation-guided drill was used to create a pilot hole for the CBT screw at the junction of the superior articular process and pars interarticularis, following a medial-to-lateral path in the axial plane and a caudo-cephalad path in the sagittal plane. After the trajectory was created and tapped, CBT pedicle screws were placed bilaterally along the tracks (Fig. 4). A thorough posterior decompression, including bilateral facetectomy and total discectomy, was carried out. The endplate cartilage was removed, and the intervertebral cage was placed. The cages and the disc space were filled with autogenous bone obtained from the decompression to provide interbody fusion. The self-retaining retractor was removed, and the wound was closed in a standard way. A sterile wound dressing was applied.
Outcome and follow-up
The patient was allowed to walk the first day after surgery. Significant postoperative relief of radiating pain in the lower limbs was obtained. Moderate pain (VAS = 3-4 p.) and discomfort remained in the postoperative wound area, which was well controlled by non-steroidal analgesics. The patient was discharged from the hospital two weeks after surgery. She was encouraged to avoid sitting for long periods and heavy lifting during the first 3 months after surgery.
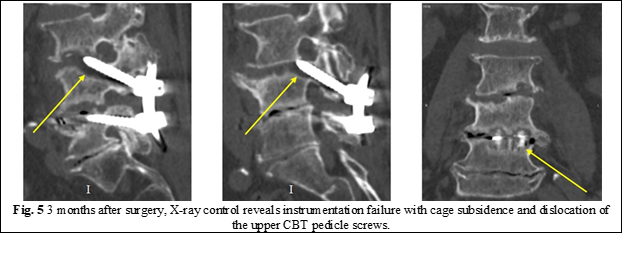
At 3 months postoperatively, the patient presented with severe pain (VAS = 8p.) in the lumbar region, without radiation to the lower limbs. A follow-up radiograph was performed, which showed signs of mechanical failure of the screw fixation system, with dislocation of the proximal pedicle screws in the cranial direction and subsidence of the interbody cages (Fig. 5).
The patient was advised to wear a lumbar brace and take special medication (vitamin D and calcium) to accelerate the process of interbody fusion. The CT scan control was scheduled for 6 months after surgery.
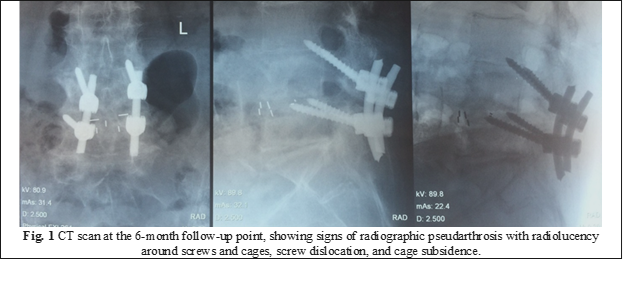
At the 6-month follow-up point, the patient presented with persistent axial low-back pain (VAS = 6p.), radiating in the lower limbs (VAS = 4p.). The ODI score was 42%, corresponding to a severely disabled patient. A computer tomography scan showed clear signs of radiographic pseudarthrosis, with loosening and migration of the cranial screws, subsidence of interbody cages, and a significant radiolucent halo around implants (Fig. 6).
The patient was offered the option of revision surgery with removal of the CBT screws and fixation of the spine with traditional pedicle screws augmented with vertebroplasty cement. The patient decided to decline the proposed treatment for her own reasons. She was allowed to continue conservative treatment under the supervision of her family doctor.
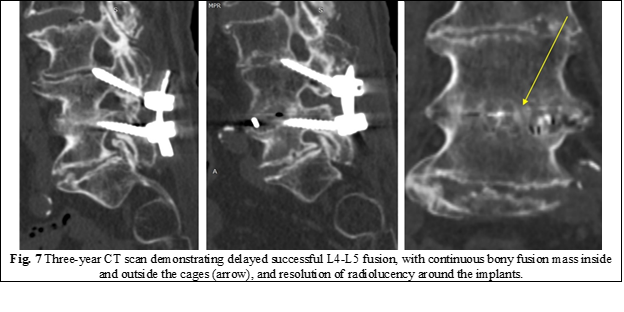
She was unable to follow up after that. Being a participant in a scientific trial, she was called for a final examination at the 3-year follow-up point. She presented only with mild low back pain (VAS = 2p.) without radiating pain. Her ODI score improved to 18%, which correlated with a state of only mild disability. A lumbar spine CT scan confirmed the presence of solid interbody fusion (BSF-3) and the absence of radiolucency around the implants (Fig. 7).
Discussion
Insufficient grip strength leading to mechanical hardware failure is a well-known drawback of traditional pedicle screws, especially in osteoporotic patients. CBT pedicle screws have been proposed as a solution to reduce the rate of screw loosening due to the purchase of higher-density bone in the pars interarticularis area.
The DEXA scan has been the gold standard for assessing bone mineral density (BMD) prior to spinal instrumentation surgery. However, DEXA scans can result in falsely elevated BMD measurements in patients with severe degenerative changes, compression fractures, and calcification of the aorta.
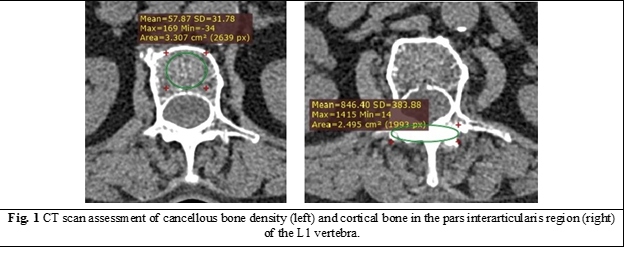
In our case, the DEXA scan showed a normal BMD of the lumbar vertebrae. To explain the failure of arthrodesis, preoperative computed tomography data were reviewed, and the method of bone quality assessment described by Zaidi et al. was applied [2]. This method involves measuring the density of cancellous bone tissue at the level of the L1 lumbar vertebra, with a threshold value of 110 HU being highly (> 90%) specific for osteoporosis. A free trial version of RadiAnt DICOM Viewer software was used to measure vertebral bone density. A density of 57 HU was found in the cancellous bone of the L1 vertebra (Fig. 8), which correlates with the presence of severe osteoporosis and explains the pseudarthrosis formation.
Our observations corroborate with those of other studies [3-5] that state that a DEXA scan alone is insufficient for an accurate diagnosis of vertebral osteoporosis when important degenerative changes or vascular calcifications are found in preoperative lumbar radiological examinations.
Pseudarthrosis remains one of the most challenging problems facing the spinal surgeon. It is usually defined as failure of bony union between two vertebrae within one year after surgery, indicated by the absence of continuous trabecular osseous bridging between vertebrae, peri-implant radiolucency on CT, and motion on flexion-extension radiographs. The patient with symptomatic pseudarthrosis usually presents with worsening axial back pain. After the diagnosis of pseudarthrosis, depending on the clinical situation, there are many different treatment options. The primary principles include stabilization of the existing posterior fixation by replacing the loose pedicle screws, followed by additional bone grafting.
However, there is no unanimous consensus on when a patient with pseudarthrosis should undergo revision surgery. Tokuhashi et al. declared that it is not reasonable to define a failure to achieve osseous union within one year after posterior spinal surgery as pseudarthrosis and that the condition should instead be called delayed union [6]. They reported that the postoperative pedicle screw radiolucent zone disappeared over time in approximately two-thirds of patients treated with posterior lumbar arthrodesis, and its presence did not necessarily indicate permanent pseudarthrosis [7]. Another study published by Kanemura et al. (2014) stated that the interbody arthrodesis site in patients with early pseudarthrosis may begin to change to a successful fusion one or two years after surgery, with two-thirds of such patients exhibiting successful fusion five years after surgery. They concluded that a final determination of nonunion or delayed union after posterior lumbar interbody arthrodesis should be made three years after surgery [8].
Conclusions
A DEXA scan can result in falsely elevated BMD values in patients with spinal degeneration, severe spine deformities, or vascular calcifications. A CT scan could be successfully used to assess bone quality before instrumented spine surgery.
The measurement of bone density in Hounsfield units is rapid, simple, and reproducible. A cut-off value of 110 HU measured in the L1 vertebra is considered highly specific for osteoporosis. These patients are at risk for screw loosening, subsidence, and pseudarthrosis. Careful surgical treatment planning is essential for this type of patient.
Even if the majority of trials suggest that CBT-screw fixation is a reasonable and superior alternative to traditional pedicle screws for osteoporotic populations, the risk of hardware failure in these patients remains very high, imposing the need to consider safer alternatives such as cement-augmented pedicle screws.
A final assessment of the pseudarthrosis should be performed at least three years after surgery.
Abbreviations
BMD – bone mineral density, CBT – cortical bone trajectory, CT – computer tomography, DEXA – dual X-ray absorptiometry, MIDLIF – Midline Lumbar Interbody Fusion, MRI – Magnetic Resonance Imaging, HU – Hounsfield unit.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
None declared.
Author’s ORCID iD
Serghei Borodin – https://orcid.org/0000-0003-2082-1976
References
Santoni BG, Hynes RA, McGilvray KC, Rodriguez-Canessa G, Lyons AS, Henson MA, et al. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009;9(5):366-73. doi: 10.1016/j.spinee.2008.07.008.
Zaidi Q, Danisa OA, Cheng W. Measurement techniques and utility of hounsfield unit values for assessment of bone quality prior to spinal instrumentation: a review of current literature. Spine. 2019;44(4):e239-e244. doi: 10.1097/brs.0000000000002813.
Hendrickson NR, Pickhardt PJ, Del Rio AM, Rosas HG, Anderson PA. Bone mineral density T-scores derived from CT attenuation numbers (Hounsfield Units): clinical utility and correlation with dual-energy X-ray absorptiometry. Iowa Orthop J. 2018;38:25-31.
Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N. Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med. 2013;158(8):588-95. doi: 10.7326/0003-4819-158-8-201304160-00003.
Zou D, Li W, Deng C, Du G, Xu N. The use of CT Hounsfield unit values to identify the undiagnosed spinal osteoporosis in patients with lumbar degenerative diseases. Eur Spine J. 2019;28(8):1758-66. doi: 10.1007/s00586-018-5776-9.
Tokuhashi Y, Ajiro Y, Umezawa N. Follow-up of patients with delayed union after posterior fusion with pedicle screw fixation. Spine. 2008;33(7):786-91. doi: 10.1097/BRS.0b013e31816956f7.
Tokuhashi Y, Matsuzaki H, Oda H, Uei H. Clinical course and significance of the clear zone around the pedicle screws in the lumbar degenerative disease. Spine. 2008;33(8):903-8. doi: 10.1097/BRS.0b013e31816b1eff.
Kanemura T, Matsumoto A, Ishikawa Y, Yamaguchi H, Satake K, Ito Z, et al. Radiographic changes in patients with pseudarthrosis after posterior lumbar interbody arthrodesis using carbon interbody cages: a prospective five-year study. J Bone Joint Surg Am. 2014;96(10):e82. doi: 10.2106/jbjs.l.01527.

