Introduction
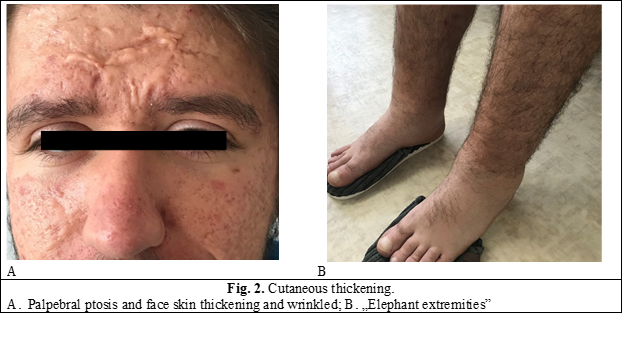
Primary hypertrophic osteoarthropathy or pachydermoperiostosis (PDP) is a rare genetic disease with both autosomal dominant and autosomal recessive transmission. It is mainly found in males, who have more pronounced clinical manifestations; the male/female ratio is 9:1 [1]. This pathology affects the skin and bones and is characterized by the association of cutaneous manifestations (pachydermia or thickening of the skin) with rheumatological manifestations (periostosis and digital clubbing). Onset of the disease usually occurs at puberty, with thickening and wrinkling of the face (pachydermia), causing thickening of the facial features, ptosis of the eyelids and cutis verticis gyrata on the scalp. Another characteristic feature is the enlargement of the fingertips (digital clubbing), which can appear from childhood or in adolescence, sometimes remaining the only clinical manifestation. Structural changes can also occur in the osteo-articular system, manifesting by the swelling of the periarticular tissues and the bone proliferation of the tubular bones at the level of the periosteum (periostosis). The lower part of the legs can take on a cylindrical shape known as “elephant foot” [2]. Joint involvement can be characterized by arthritis, hydrarthrosis arthralgias, and hemarthrosis. Other clinical manifestations include seborrhea, acne, hyperhidrosis of the palms and soles, eczema, feeling of warmth in the hands and feet. PDP can be complicated with neurological manifestations and can be associated with structural cardiac manifestations. These changes usually progress 5-20 years, and then remain permanently stable. From a clinical point of view, PDP is divided into 3 subclasses: I – the complete form, which presents the phenotype in general, II - an incomplete form, with isolated bone involvement and limited skin changes, and III - a truncated form, with minimal or absent pachydermia and periostosis [3].
Case presentation:
A 20-year-old man was admitted to rheumatology department presents with the following complaints: pain accompanied by swelling in the hands and feet, pain in his both ankles, and knees with The onset of the disease was insidious, at the age of 14, when pain in the joints of both knees and ankles and low fever appeared, after several episodes of streptococcal pharyngitis. He received anti-inflammatory treatment in the rheumatology department of the pediatric hospital, being diagnosed with juvenile idiopathic arthritis. Treatment with NSAIDs and antibacterial medicines reduced pain intensity and joint swelling. Few months later, he noticed the appearance of pustular acne on his face and upper body. At the age of 15, he noticed a sudden increase in his height (+20cm) and in the size of hands and feet (from size 40 to 45), with swelling of soft tissues. He periodically had cold symptoms accompanied by arthralgia, during which he administered various types of NSAIDs. Considering the frequent colds, in 2018 he underwent a tonsillectomy, followed by the administration of benzathine penicillin for a duration of 6 months. In 2019, a pituitary tumor was ruled out after a brain MRI examination. In addition, thyroid scintigraphy in 2019 did not confirm any thyroid disease to explain the clinical symptoms.
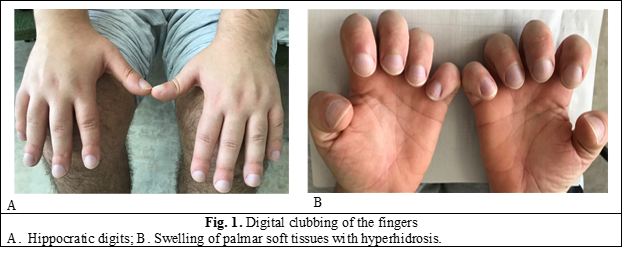
During the physical examination, we noticed the presence of Hippocratic fingers on the hands and feet; diffuse swelling of the palmar and plantar soft tissues accompanied by hyperhidrosis (fig.1). At the level of the face, palpebral ptosis and thickening of the tegument are determined (fig 2A). At calf level - cylindrical deformity known as „elephant extremities” (fig. 2B).
Laboratory investigations show normal values of hematological parameters, as well as ESR, C-reactive protein, electrolytes, transaminases, bilirubin, total protein, albumin, coagulogram, uric acid, LDH, CPK, lipid profile, normal levels of thyroid indices (TSH, FT4). ECG, chest X-ray without pathological changes.
Genetic testing with next-generation sequencing (with lllumina NextSeq and Illumina Trusight One Expanded set) identified heterozygous variants NM_005630.3:c. 1658delT p.(lie553Thrfs*7) of the SLCO2A1 gene (Laboratorio di Genetica, Azienda Ospedale – Universita di Padova). Inactive variants of the SLCO2A1 gene are associated with autosomal recessive primary hypertrophic osteoarthropathy syndrome (MIM#614441).
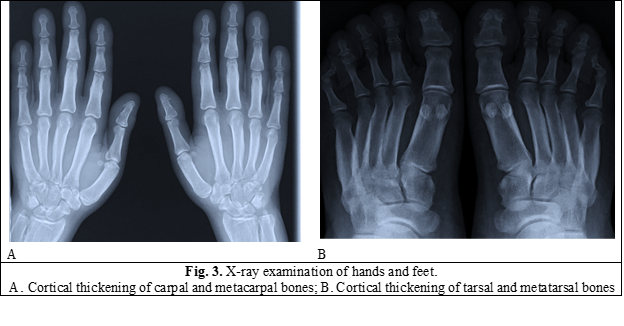
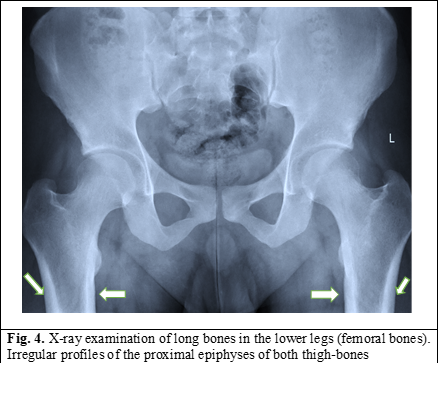
Radiographic examination of hands, feet, and long bones of lower legs show cortical thickening of the metacarpals and proximal phalanges of both hands (fig. 3), significant and irregular thickening of the periosteum - cortex of the femoral bones (fig. 4).
Based on the clinical and paraclinical results, we established the diagnosis: Primary hypertrophic osteoarthropathy (or Pachydermoperiostosis). Treatment with NSAIDs during the periods of arthralgias and joint swelling temporarily relieved the symptoms.
Discussions
Hypertrophic osteoarthropathy (OAH) is a clinical syndrome, manifested by the increase in size of the extremities as a result of bone and periarticular proliferation, Hippocratic fingers and toes, and painful swellings in the joints. This can be primary (PDP) and secondary. Secondary or pulmonary OAH is associated with a lung pathology, often lung cancer. It is important to make a differential diagnosis between these two pathologies, in order to determine the subsequent treatment process [1].
Referring to the presented clinical case, the age of onset of this pathology is specific – in adolescence. The patient presents the full form of the disease, with both dermatological and rheumatological clinical manifestations. The consecutiveness of the appearance of clinical manifestations is observed, starting with the increase in the size of the extremities, Hippocratic fingers, arthralgias, and osalgias and continuing with the skin manifestations, which developed during puberty, thus making it difficult to establish the diagnosis. It is important that for about 1.5 years the patient has shown stagnation in growth, already suspecting a slowing down of the disease, which is known to occur after 5-20 years after the initiation of structural changes. According to the investigations carried out, no structural manifestations or increases in the size of the internal organs were determined. In addition, the laboratory analyzes and the hormonal profile are within the limits of the norms, which helps to establish the diagnosis of PDP. Due to such a varied clinical picture, it was initially difficult to determine the diagnosis and differential diagnosis was performed with several pathologies. Among them were acromegaly, secondary OAH, SAPHO disease.
To differentiate PHP from secondary OAH, it is necessary to examine the chest to rule out a lung mass. In the reported case, the presence of a formation in the lungs was not determined.
Authors had to differentiate it from the SAPHO disease. It is known that the manifestations in SAPHO appear late, mainly between 30-50 years, in the case of the patient it is known that it started in adolescence. Cutaneous manifestations differ in the presence of acneiform and pustular eruptions but thickening of the skin with changes in facial features, palpebral ptosis, and cutis verticis gyrata are not attested. In addition, the musculoskeletal manifestations in SAPHO disease have a more central spread, affecting the chondro-sternal, sacroiliac, coxofemural and knee joints. Nevertheless, peripheral joint damage and Hippocratic fingers are specific for PDP, these manifestations are present in the studied patient from this clinical case.
Acromegaly has similarities with PDP. The presence of Hippocratic toes and periostosis, plus the absence of prognathism, enlargement of the sella turcica, or abnormal circulating concentrations of growth hormone products would be helpful in establishing this diagnosis. According to the results of the laboratory data, the presented patient does not show any changes specific to this pathology.
Thyroid acropachy is characterized by periosteal proliferation located mainly in the small tubular bones of the hands and feet, being a rare manifestation of Graves' disease and independent of the state of thyroid function. Clubbing usually coexists with exophthalmos and pretibial myxedema. Myxedema resembles the elephant's feet described in HOA. The presence of digital clubbing for several years in the absence of a recognized internal disease is in favor the diagnosis of PDP.
It is necessary to differentiate this pathology from others, such as cranio-osteoarthropathy, chronic recurrent multifocal osteomyelitis, Camurati-Engelman disease, and syphilitic periostosis, in order to determine the correct treatment tactics. PDP is a self-limiting pathology with no effect on life expectancy. Symptoms stabilize or even resolve in the third or fourth decade, with an average interval of 10 years after the onset of symptoms. In the case of persistent joint and bone pain syndrome, the administration of analgesic medications and COX2-inhibiting NSAIDs have been shown to be effective in reducing arthritis. A regression of inflammatory markers (ESR, CRP) was determined when Etoricoxib was administered [4]. Rheumatologic symptoms may also be improved by treatment with bisphosphonates such as pamidronic acid or risedronate. Bisphosphonates inhibit osteoclastic resorption and therefore reduce bone remodeling and improve polyarthritis [4]. In the hospital, anti-inflammatory medication was administered, and at discharge, the arthralgia and swelling of the soft tissues decreased. The patient needs to be reevaluated periodically (every 3-6 months) after being discharged with recommendations of using COX2 inhibitors.
Conclusions
The diagnosis of pachydermoperiostosis is based on the clinical manifestations presented by the patient and requires more detailed laboratory evaluation to differentiate it from other similar pathologies. To confirm the diagnosis, it is necessary to find the presence of cutaneous (thickening and wrinkling of the face (pachydermia), thickening of facial features and ptosis of the eyelids and scalp producing cutis verticis gyrata) and rheumatological manifestations (Hippocratic fingers, swelling of periarticular tissues and bone proliferation of tubular bones at the level of periosteum (periostosis) manifesting as „elephant's foot”). It is imperative to know the diagnostic criteria in order to administer a specific treatment for this pathology. For PDP, symptomatic treatment with analgesics and COX2-inhibiting NSAIDs are indicated. In addition, some studies mention the importance of bisphosphonates in reducing the progression of hyperostosis.
Authors’ contribution
All listed authors have provided a significant contribution to the collecting of material and writing this article. All authors revised and approved the final version of the manuscript.
Informed consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
None declared.
Authors’ ORCID IDs
Marinela Homițchi – https://orcid.org/0000-0002-1357-2388
Serghei Popa – https://orcid.org/0000-0001-9348-4187
Lucia Dutca – https://orcid.org/0000-0002-1815-2294
Svetlana Agachi – https://orcid.org/0000-0002-2569-7188
References
Martinez-Lavin M. Miscellaneous non-inflammatory musculoskeletal conditions. Pachydermoperiostosis. Best Pract Res Clin Rheumatol. 2011 Oct;25(5):727-34. doi: 10.1016/j.berh.2011.10.019.
Yap FY, Skalski MR, Patel DB, Schein AJ, White EA, Tomasian A, Masih S, Matcuk GR Jr. Hypertrophic osteoarthropathy: clinical and imaging features. Radiographics. 2017 Jan-Feb;37(1):157-195. doi: 10.1148/rg.2017160052.
Castori M, Sinibaldi L, Mingarelli R, Lachman R, Rimoin D, Dallapiccola B. Pachydermoperiostosis: an update. Clin Genet. 2005;68(6):477-486. doi: 10.1111/j.1399-0004.2005.00533.x.
Zhang H, Yang B. Successful treatment of pachydermoperiostosis patients with etoricoxib, aescin, and arthroscopic synovectomy: two case reports. Medicine (Baltimore). 2017 Nov;96(47):e8865. doi: 10.1097/MD.0000000000008865.

