Introduction
Implant-prosthetic rehabilitation has become the preferred method for treating patients with various forms of edentulism. In the lateral areas of the upper jaw, a deficiency in the height of the alveolar ridge is often encountered, resulting from the pneumatization of the maxillary sinus and the atrophy of the alveolar process following tooth loss. The low subantral bone height creates challenges for the insertion of endosseous dental implants. Currently, the most used methods for solving this issue are transcrestal or lateral sinus lifting operations.
The lateral sinus lift technique involves creating a bony window on the lateral wall of the maxillary sinus, elevating the Schneiderian membrane, and grafting the subantral space with a variety of materials, including autogenous bone, allografts, xenografts, alloplastic materials, or mixtures thereof [1-3]. Despite the fact that this procedure alters the anatomy of the maxillary sinuses by lifting the sinus membrane, it has been demonstrated not to have any adverse impact on sinus function.
Non-pathological sinus augmentation poses little risk of ostium obstruction or sinus dysfunction due to the cranial position of the ostium. However, when bone augmentation of the maxillary sinus is performed in the presence of a pathological condition that significantly reduces the lumen of the sinus, the risk of obstruction after a sinus lift can be increased. This scenario can result in the stagnation of mucus secretion inside the sinus, leading to a sinus infection [4-6].
A small mucosal cyst in the maxillary sinus (MSMC) does not pose a contraindication to the sinus lift procedure, as the risk of complications during or after surgery, such as membrane perforation or ostial obstruction, is minimal [7-9].
Nevertheless, the presence of a large MSMC (occupying at least one-third of the sinus volume) can create difficulties during the elevation of the sinus membrane and may damage the ostium following the augmentation procedure [5, 10].
Obstruction of the ostium can lead to mucus accumulation inside the maxillary sinus and loss of sinus ventilation [4-6]. The severe complications that can occur are caused by the spread of the infection to other paranasal sinuses, the orbit, and even the cranial cavity [11, 12].
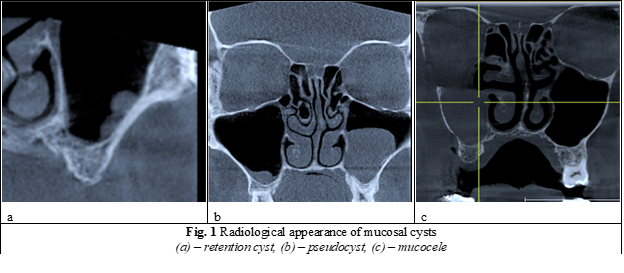
The formation of retention cysts (secretory type) (Fig. 1a) is believed by Gerlings P. and Lindsay J. to be caused by blockage of the excretory duct of the seromucous glands due to sinus infection, allergy, odontogenic infection, or traumatic extraction [13, 14].
Mucosal pseudocysts of the non-secretory type (Fig. 1b), as described by Harar R., are formed by the accumulation of exudate in the conjunctival layer of the maxillary sinus mucosa, between the periosteum and the epithelial layer. The occurrence of pseudocysts is a topic of debate. Some authors argue that in 50% of cases, the etiology is odontogenic due to the penetration of oral microflora in the cystic fluid (bacteriologically determined in the cystic fluid), as well as the fact that most cysts originate from the mucosa of the sinus floor at the level of the apical odontogenic foci of the affected teeth [15]. Bacterial toxins destroy the walls of the capillaries, leading to protein loss in the tissues. This results in an increase in the osmotic pressure and blockage of the reabsorption of tissue fluids. As a consequence, fluid accumulates in many areas of the subepithelial space, which ultimately coalesce to form the pseudocyst [14].
Mucocele (Fig. 1c) is a lesion that is most found in the frontal sinus, less often in the ethmoid cells, and sporadically in the maxillary sinus. Kuczkowski J. performed the most extensive characterization of mucoceles and described them as cyst-like formations [3]. The mucocele is lined with epithelium, contains mucoid fluid, and has an expansive, destructive growth that is associated with obstruction of the natural ostium of the respective sinus. The mucocele causes compressive resorption of the bone through intraluminal fluid pressure, resulting in invagination into adjacent cavities such as the cranial box, orbit, or under the skin surface. Clinical symptoms of mucocele include headache, diplopia, decreased vision, and nasal obstruction. Histologically, the mucocele exhibits sac-shaped hernias of the sinus mucosa [16].
Mucocele in the maxillary sinus is a relatively uncommon condition, with most cases reported in Japan, where they are referred to as postoperative cysts [17]. Among the 22 cases of antral mucocele reported by Kuczkowski J. [3], all 22 were caused by the Caldwell-Luc radical cure. Similarly, all 71 cases reported by Kaneshiro et al. in Japan were secondary, occurring after radical cure of the sinus [18].
In the pre-implantation preparation of patients with maxillary sinus pathology, specialists are often faced with uncertainty when deciding whether to perform sinus lifting surgery in the presence of a mucosal cyst. Some specialists believe that sinus lifting cannot be performed in the presence of sinus pathology and should be delayed until a later stage of healing, while others believe that it can be done in conjunction with sinus drainage. As a result, there is considerable controversy regarding treatment tactics, stages, and optimal timing for achieving rehabilitation in these patients, highlighting the relevance of the problem at hand.
Materials and methods
The study included twenty patients who sought implant-prosthetic rehabilitation for partial edentulism in the lateral area of the upper jaw and the presence of a mucosal cyst in the maxillary sinus at the Department of OMF Surgery and Oral Implantology "Arsenie Guţan" and the dental clinic "OmniDent" between 20.06.2016 and 01.01 2019. All patients underwent a sinus lift operation despite the presence of the MSMC. Depending on the method of managing the mucosal cyst, patients were divided into three study groups.
The study was approved by the Ethics Committee (EC) of the Nicolae Testemițanu State University of Medicine and Pharmacy, decision No. 77 (17.06.2016). The chair of the EC was Nacu Viorel.
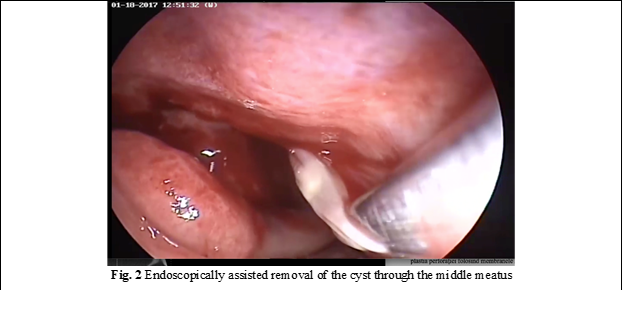
The first study group consisted of seven patients, aged between 31 and 64 years (with an average age of 43 years). In this group, the mucosal cyst was completely removed, and a lateral sinus lifting operation was performed simultaneously. The cyst removal was carried out using two methods: endoscopic removal and removal through a small perforation of the mucosa in the lateral wall of the maxillary sinus.
The endoscopic method involved the following steps: First, the uncinate process was identified through anterior rhinoscopy of the respective nostril using a straight rigid optic (0°), and subsequently resected. Next, angled optics (40°) were used to identify the natural ostium of the maxillary sinus, which was slightly enlarged with the aid of Blacksley forceps. The cyst was then completely removed from the maxillary sinus through the natural ostium using antral forceps. Following cyst removal, sinus lifting was performed using the classical method, as illustrated in Fig. 2.
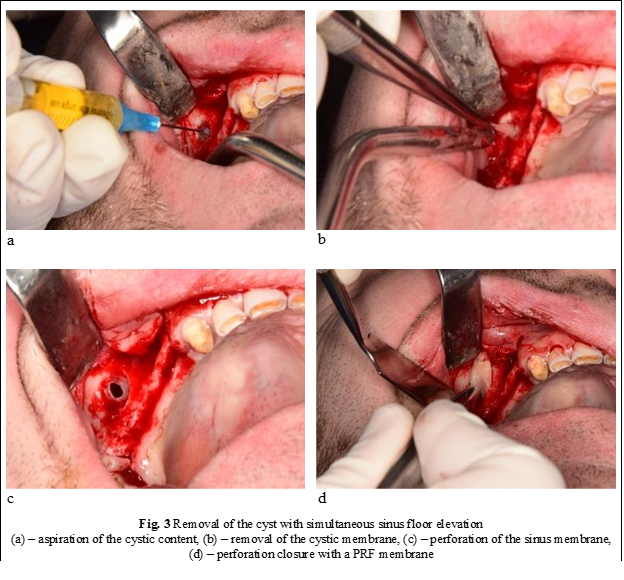
The second method used to completely remove the cyst involved the following steps, as illustrated in Fig. 3: First, a trapezoidal incision was made in the edentulous area of the oral mucosa. The muco-periosteal flap was then detached, and an osteotomy of the side wall of the maxillary sinus was performed using drill no. 5 from the "Dentium" kit, taking care not to damage the sinus mucosa. Next, the maxillary sinus was punctured using a needle and syringe through Schneider's membrane, and the cystic contents were aspirated. With the help of a thin forceps and suction, the cystic membrane was carefully pulled through the microperforation created by the needle, exposed in the oral cavity, and removed. After cyst removal, the sinus mucosa was elevated, and the perforation was closed using either PRF membranes or artificial membranes. Finally, the subantral space was augmented, with or without the insertion of implants (Table 1).
Table 1. Patients’ data included in the study. | |||||||
Nr. | Sex | Age, year | Sinus left/ right | Group | Preoperative mucosal thickness, mm | Postoperative mucosal thickness, mm | Sinus lifting Immediate/delayed |
1 | m | 52 | r | 2 | 28.83 | 19.77 | delayed |
2 | w | 50 | l | 2 | 37.99 | 12.35 | immediate |
3 | w | 64 | r | 1 | 36.20 | 0 | delayed |
4 | m | 64 | r | 3 | 25.94 | 28.47 | immediate |
5 | m | 57 | l | 2 | 16.44 | 16 | immediate |
6 | w | 67 | r | 2 | 22 | 4.87 | immediate |
7 | m | 38 | r | 2 | 24 | 3.23 | immediate |
8 | w | 39 | l | 1 | 28 | 0 | immediate |
9 | m | 34 | r | 3 | 12.68 | 12.68 | immediate |
10 | m | 18 | r | 1 | 17.13 | 0 | delayed |
11 | w | 61 | r | 3 | 14.22 | 13.05 | immediate |
12 | m | 49 | r | 2 | 23.44 | 3.55 | immediate |
13 | m | 46 | l | 3 | 20.28 | 20.28 | immediate |
14 | m | 47 | l | 3 | 18.34 | 0 | immediate |
15 | w | 57 | r | 1 | 32.56 | 0 | immediate |
16 | m | 55 | l | 2 | 17.14 | 8.1 | immediate |
17 | w | 31 | l | 1 | 29.33 | 0 | immediate |
18 | m | 55 | r | 1 | 15.29 | 0 | immediate |
19 | m | 46 | l | 2 | 37.77 | 9.6 | immediate |
20 | m | 40 | l | 3 | 15.64 | 14.66 | immediate |
Total | m – 13 w – 7 | min – 18 max – 64 average – 48.33 | r – 11 l – 9 | 1 2 3 | min – 12.68 max – 37.99 average – 23.81 | min – 0 max – 28.47 average – 8.33 | i – 17 d – 3 |
Note: Descriptive statistics; m – man; w – woman; l – left; r – right; i – immediate; d – delayed | |||||||
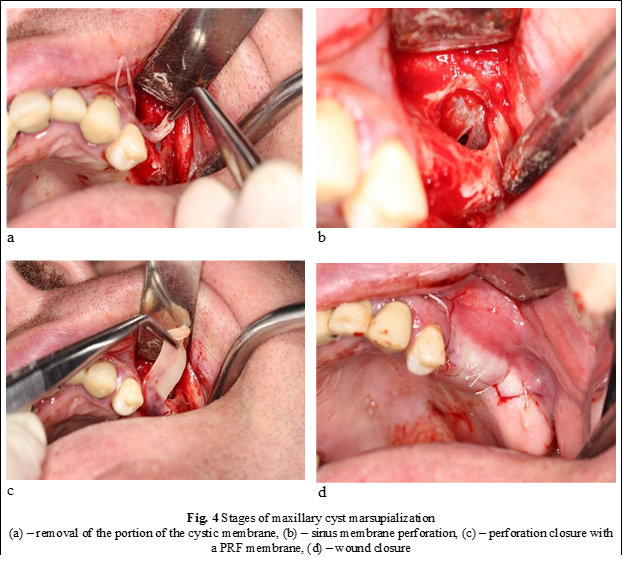
Group 2 included five patients aged between 18 and 67 years (with an average age of 45 years) who underwent marsupialization of a mucosal cyst. The intervention method was similar to the previous one in terms of surgical steps. The only difference was that the cyst membrane was sectioned with scissors without being entirely removed (Fig. 4).
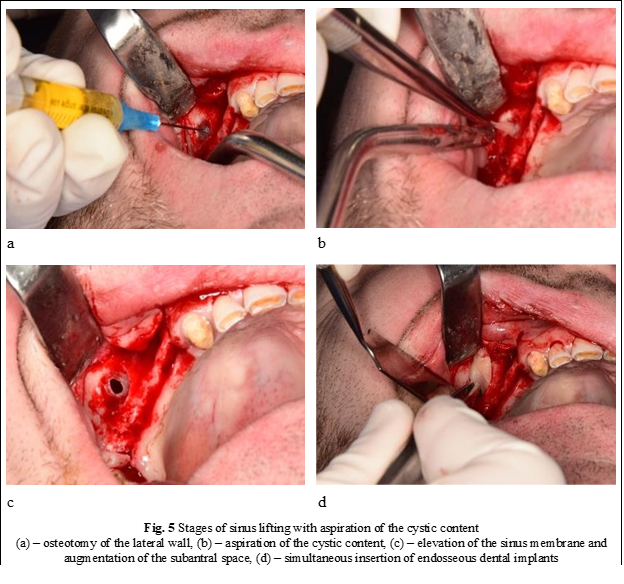
Group 3 comprised six patients aged between 34 and 61 years (mean age: 53 years). In these patients, only the cyst content was aspirated, without removal or marsupialization of the cyst (Fig. 5).
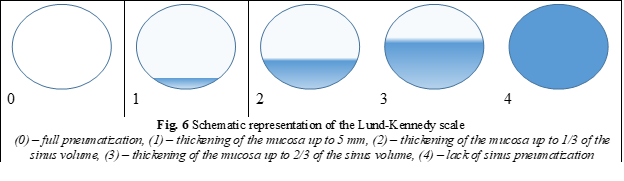
A computed tomography was performed on all patients both before and after the operation, with a minimum interval of 6 months between the two scans. The Lund-Kennedy scale was assessed before and after the operation (Fig. 6).
Results
Of the patients in our study, the majority were men (13 out of 20, or 65%). The average age of the patients was 48 years. We assessed each patient's Lund-Kennedy scale both before sinus floor elevation and 6 months after the operation.
Based on the tables presented, it is apparent that the first group of patients, in which the cyst was completely removed, had no recurrences. In the second group, where marsupialization of the cyst was performed, the cyst visibly decreased in volume during the postoperative period. However, in the third group, where only the cyst content was aspirated, the cyst returned to its original size after a short period of time. While these results suggest that complete removal of the cyst is the most effective method for treating mucosal cysts when the sole goal is to remove the cyst, it remains unclear which method is optimal when a sinus lifting operation is also necessary. Specifically, it is unclear whether the method used in Group 1 remains the most effective in this context.
Discussions
Lin Y., et al. [9] described a two-stage protocol with delayed sinus lift, in which sinus grafting was performed approximately 3 months after pseudocyst removal. Eleven patients were treated using this approach. During the first operation, a small lateral access was made to remove the pseudocyst. Three months later, sinus augmentation was performed, and dental implants were inserted 6 months after the sinus grafting procedure. The authors reported no instances of sinus membrane perforation during sinus membrane elevation, no implant loss, and no cystic recurrence after a mean follow-up of 29 months. One of the disadvantages mentioned was that patients had to undergo two separate surgeries. Furthermore, the procedures and elevation of the sinus floor were performed through the same access route as in the first surgical intervention. This required dissection between the sinus membrane and the oral mucoperiosteum, which increased the technical difficulty of the sinus lifting operation.
Table 2. Obtained results | |||||
| Cyst management | ||||
Removal | Marsupialization | Aspiration | |||
Age, years | minimum | 18 | 31 | 34 | |
maximum | 64 | 61 | 64 | ||
average | 47 | 45 | 53 | ||
standard deviation | 18 | 10 | 10 | ||
25th percentile | 47 | 39 | 46 | ||
median | 49 | 43 | 55 | ||
75th percentile | 58 | 51 | 61 | ||
Sex | m | total | 5 | 5 | 4 |
column N % | 100.0 | 62.5 | 57.1 | ||
lower 95,0% | - | 29.5 | 23.5 | ||
upper 95,0% | - | 88.1 | 86.1 | ||
w | total | 0 | 3 | 3 | |
column N % | 0.0 | 37.5 | 42.9 | ||
lower 95,0% | - | 11.9 | 13.9 | ||
upper 95,0% | - | 70.5 | 76.5 | ||
Lund-Kennedy before surgery | 2 | total | 3 | 3 | 4 |
column N % | 60.0 | 37.5 | 57.1 | ||
lower 95,0% | 20.9 | 11.9 | 23.5 | ||
upper 95,0% | 90.6 | 70.5 | 86.1 | ||
3 | total | 1 | 3 | 1 | |
column N % | 20.0 | 37.5 | 14.3 | ||
lower 95,0% | 2.3 | 11.9 | 1.6 | ||
upper 95,0% | 62.9 | 70.5 | 50.1 | ||
4 | total | 1 | 2 | 2 | |
column N % | 20.0 | 25.0 | 28.6 | ||
lower 95,0% | 2.3 | 5.6 | 6.5 | ||
upper 95,0% | 62.9 | 59.2 | 64.8 | ||
Lund-Kennedy after surgery | 0 | total | 3 | 3 | 3 |
column N % | 60.0 | 37.5 | 42.9 | ||
lower 95,0% | 20.9 | 11.9 | 13.9 | ||
upper 95,0% | 90.6 | 70.5 | 76.5 | ||
1 | total | 1 | 2 | 0 | |
column N % | 20.0 | 25.0 | 0.0 | ||
lower 95,0% | 2.3 | 5.6 | . | ||
upper 95,0% | 62.9 | 59.2 | . | ||
2 | total | 0 | 3 | 4 | |
column N % | 0.0 | 37.5 | 57.1 | ||
lower 95,0% | - | 11.9 | 23.5 | ||
upper 95,0% | - | 70.5 | 86.1 | ||
4 | total | 1 | 0 | 0 | |
column N % | 20.0 | 0.0 | 0.0 | ||
lower 95,0% | 2.3 | - | - | ||
upper 95,0% | 62.9 | - | - | ||
Note: Descriptive statistics; lower 95% and upper 95% represent a 95% confidence interval | |||||
We believe that this method should only be considered when other approaches have failed. In fact, we have used this technique in only two cases (one from group 1 and one from group 2) when attempts to remove or marsupialize the cyst resulted in large perforations, making it difficult to predict the outcome of the sinus lift. Therefore, we decided to postpone the sinus lift for 3 months. The procedure was successfully performed without any perforations or risks of pushing the augmentation material into the sinus.
The one-step protocol was first introduced by Pikos et al. In this approach, a conventional bone "window" is created, and then the pseudocyst is removed by intentionally perforating the sinus membrane. Sinus grafting is performed after the sinus membrane is closed with resorbable collagen membranes. Although the authors reported positive results, it is important to note that these outcomes are based on individual cases. Furthermore, intentional perforation of the sinus membrane is contrary to the biological principles of the sinus augmentation technique [1]. While it is possible to close the perforation with collagen membranes, complications such as contamination of the graft material and its dispersion in the maxillary sinus may occur [1, 11].
We used the given method to treat the first group of patients. Although this method allows to remove the cyst entirely, we found that it resulted in an unpredictable-sized perforation instead. After the removal of the cyst and the elevation of the sinus floor, we had to perform the closure of the perforation. In our study, we performed PRF membrane closure. However, in one case, we couldn't continue the intervention due to a massive perforation. Considering that mucosal cysts of the maxillary sinus do not require specific treatment (surgical or medicinal), are not considered tumors, and do not typically lead to complications, it may not be necessary to remove the cyst in its entirety, which could result in intraoperative complications.
In our search for new treatment methods, we decided to apply the marsupialization technique, which we commonly used for managing massive odontogenic cysts, to treat these patients. This technique involves ensuring the drainage of the cyst over an extended period, which reduces the intracystic pressure and causes the cyst to shrink in volume. However, in contrast to jaw cysts, where the cystic membrane attaches to the bone walls, this is not possible with sinus cysts. As a result, the mucosal cyst tends to recur, first shrinking in volume and then growing again.
The authors used the given method to treat eight patients and observed the following advantages:
- the method enables directed perforation in most cases;
- it reduces pressure on the augmentation material during the healing period.
However, the biggest disadvantage of the method is that intentional perforation can enlarge the perforation if the membrane is thin. In one case, we had to postpone the sinus lift due to a large perforation.
Maiorana C., et al. proposed an alternative technique for treating sinus cysts [19]. Their method involved creating access to the maxillary sinus through osteotomy and aspirating the cystic fluid using a fine needle inserted through the sinus membrane. This step reduced both the pseudocystic volume and the tension on the sinus membrane. With these factors minimized, the sinus lift technique could be completed with minimal risk of ostium obstruction and sinus membrane perforation.
We used the given method to treat seven patients and found that unlike the first two groups, all cases resulted in good outcomes without complications. The method has several advantages, including its simplicity and ease of performance, non-perforation of the mucosa, and reduction of intracystic pressure, which facilitates detachment of the mucosa. However, the main disadvantage is that aspiration of only the liquid does not allow for complete enucleation of the pseudocyst.
Felisati G. proposed a protocol that combines the intraoral approach with the transnasal endoscopic sinus approach in a single surgical session [5]. This approach allows for transnasal treatment of pseudocysts and rhinosinusitis (if present), which is a relative contraindication to the sinus lift technique. Specifically, the elevation of the floor of the maxillary sinuses is performed through an intraoral approach immediately after the endoscopic surgery.
This protocol is an ideal solution for sinus grafting in patients with pseudocysts and nasopharyngeal conditions, such as multiple sinus cysts, nasal septum deviation, agger nasi cell hypertrophy, and concha bullosa, that can affect sinus ventilation. However, when treating only a pseudocyst that can be removed through a simple intraoral approach, the protocol has certain limitations. These include the need for two distinct surgical teams (ENT surgeons and OMF surgeons), treatment under general anesthesia, and a significant increase in price, operative time, and postoperative morbidity.
It is important to note that there is no universal method for managing mucosal cysts of the maxillary sinus in candidates for sinus lifting, and each case must be approached individually. Unfortunately, this problem has been insufficiently addressed in the specialized literature, and further studies are needed with larger patient groups to better understand and address this issue.
Conclusions
- The mucosal cyst does not present a contraindication to sinus lifting but requires additional surgical procedures.
- All methods have their advantages and disadvantages; there is no optimal method.
- The sinus lifting method with the removal of the cystic membrane through a small perforation is effective. However, sometimes it creates large perforations, which require additional plastic surgery, increase the cost of the intervention, and increase the risks of postoperative complications, although the cyst does not recur.
- The sinus lifting method with marsupialization of the cyst does not create large perforations. However, the cyst may recur but in a smaller size. This results in less pressure on the augmentation during the healing period. Nevertheless, it is important to close the perforation and monitor the patient's progress over time.
- We consider the sinus lifting method with aspiration of the cyst content to be the most effective because it does not create perforations, it is easy, and the postoperative period has low risks.
Competing interests
None declared.
Authors’ contributions
Conception and design of study – DS, AM; Data collection – AM, ID; Analysis and/or interpretation of data – AM, AMo; Drafting the manuscript – AM, DS, ID; Revising the manuscript critically for important intellectual content – AM, DS, AMo; Approval of the final version of the manuscript – all authors.
Authors’ ORCID IDs
Alexandr Mighic – https://orcid.org/0009-0007-8267-2108
Dumitru Sîrbu – https://orcid.org/0000-0003-4023-4031
Andrei Mostovei – https://orcid.org/0009-0000-1926-9403
Ion Dabija – https://orcid.org/0000-0002-7389-3394
References
Monje A, Pikos MA, Chan HL, Suarez F, Gargallo-Albiol J, Hernández-Alfaro F, Galindo-Moreno P, Wang HL. On the feasibility of utilizing allogeneic bone blocks for atrophic maxillary augmentation. Biomed Res Int. 2014;2014:814578. doi: 10.1155/2014/814578. Epub 2014 Sep 11. PMID: 25535616; PMCID: PMC4177739.
Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res. 2006 Oct;17 Suppl 2:136-59. doi: 10.1111/j.1600-0501.2006.01357.x.
Kuczkowski J, Narozny W, Stankiewicz C, Izycka-Swieszewska E, Skrzypczak W, Kowalska E, Plichta L. Sluzowiaki zatok przynosowych [Mucoceles of the paranasal sinuses]. Otolaryngol Pol. 2007;61(5):680-6. Polish. doi: 10.1016/S0030-6657(07)70506-1.
Chan HL, Wang HL. Sinus pathology and anatomy in relation to complications in lateral window sinus augmentation. Implant Dent. 2011 Dec;20(6):406-12. doi: 10.1097/ID.0b013e3182341f79.
Felisati G, Borloni R, Chiapasco M, Lozza P, Casentini P, Pipolo C. Maxillary sinus elevation in conjunction with transnasal endoscopic treatment of rhino-sinusal pathoses: preliminary results on 10 consecutively treated patients. Acta Otorhinolaryngol Ital. 2010 Dec;30(6):289-93.
Schuknecht HF, Lindsay JR. Benign cysts of the paranasal sinuses. Arch Otolaryngol. 1949;49(6):609-630. doi: 10.1001/archotol.1949.03760120036004.
Celebi N, Gonen ZB, Kilic E, Etoz O, Alkan A. Maxillary sinus floor augmentation in patients with maxillary sinus pseudocyst: case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011 Dec;112(6):e97-102. doi: 10.1016/j.tripleo.2011.06.001.
Cortes AR, Correa L, Arita ES. Evaluation of a maxillary sinus floor augmentation in the presence of a large antral pseudocyst. J Craniofac Surg. 2012;23:e535-e537. doi: 10.1097/SCS.0b013e31825aaff8.
Lin Y, Hu X, Metzmacher AR, Luo H, Heberer S, Nelson K. Maxillary sinus augmentation following removal of a maxillary sinus pseudocyst after a shortened healing period. J Oral Maxillofac Surg. 2010 Nov;68(11):2856-60. doi: 10.1016/j.joms.2010.05.091.
van den Bergh JP, ten Bruggenkate CM, Disch FJ, Tuinzing DB. Anatomical aspects of sinus floor elevations. Clin Oral Implants Res. 2000 Jun;11(3):256-65. doi: 10.1034/j.1600-0501.2000.011003256.x.
Alkan A, Celebi N, Baş B. Acute maxillary sinusitis associated with internal sinus lifting: report of a case. Eur J Dent. 2008 Jan;2(1):69-72.
MacDonald-Jankowski DS. Mucosal antral cysts observed within a London inner-city population. Clin Radiol. 1994 Mar;49(3):195-8. doi: 10.1016/s0009-9260(05)81776-3.
Gerlings PG, Hammelburg E. Keel-, neus- en oorheelkunde [Throat, nose and ear surgery]. Haarlem: Erven Bohn; 1969. p. 157. Dutch.
Lindsay JR. Nonsecreting cysts of the maxillary sinus mucosa. Laryngoscope. 1942;52(2):84-100. https://doi.org/10.1288/00005537-194202000-00002.
Harar RP, Chadha NK, Rogers G. Are maxillary mucosal cysts a manifestation of inflammatory sinus disease? J Laryngol Otol. 2007 Aug;121(8):751-4. doi: 10.1017/S0022215107005634.
Gardner DG. Pseudocysts and retention cysts of the maxillary sinus. Oral Surg Oral Med Oral Pathol. 1984;58(5):561-567. https://doi.org/10.1016/0030-4220(84)90080-X.
Li J, Wang HL. Common implant-related advanced bone grafting complications: classification, etiology, and management. Implant Dent. 2008 Dec;17(4):389-401. doi: 10.1097/ID.0b013e31818c4992.
Kaneshiro, S., Nakajima, T., Yoshikawa, Y., Iwasaki, H., & Tokiwa, N. (1981). The postoperative maxillary cyst: report of 71 cases. Journal of Oral Surgery (American Dental Association : 1965), 39(3), 191–198.
Maiorana C, Beretta M, Benigni M, Cicciù M, Stoffella E, Grossi GB. Sinus lift procedure in presence of mucosal cyst: a clinical prospective study. J Implant Adv Clin Dent. 2012;4(5):53-60.

