Introduction
Indirect pulp capping (IPC) is defined as a biological treatment method, which consists of the application of a bioactive material over a thin layer of remaining dentine after the excavation of carious tissues, without exposing the pulp. This treatment method aims primarily to protect the odontoblasts of the dental pulp and to promote the formation of reactive dentine at the pulp-dentinal junction [1]. It is also the most conservative method within the concept of vital pulp therapy (VPT), a series of treatment methods that aims to preserve and maintain pulp tissue in a healthy state that has been compromised but not destroyed by caries, trauma, or restorative procedures [2]. In our case report we used the technique of indirect pulp capping, a method that involves placing a bioactive dental material – Biodentine, onto a thin layer of affected dentine, without exposure of the pulp.
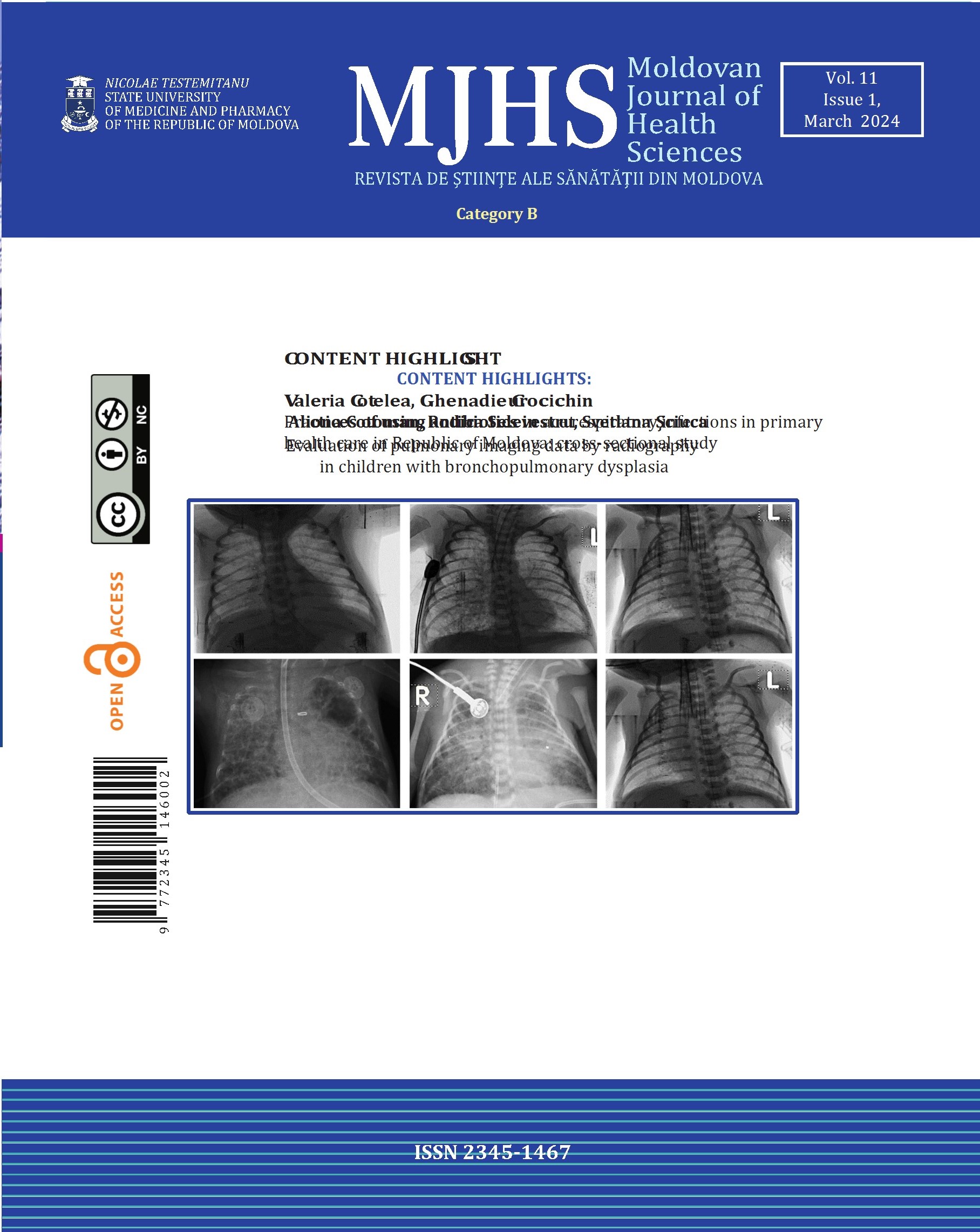
Biodentine (Septodont, France) is a calcium silicate hydraulic cement created as a dentine replacement material and specifically designed for vital dental pulp therapy. It has been commercially available since 2009 and it is based on tricalcium silicate. Its aqueous component includes reaction accelerators; thus, it classifies into type 4 hydraulic cements, according to the Camilleri classification [3]. Biodentine’s form of presentation consists of a powder in a capsule and a liquid in an ampoule, as shown in figure 1. The manufacturer recommends adding 5 drops of liquid from the ampoule to the powder in the capsule prior to mixing. Then, the capsule is inserted in the amalgamator and mixed at 4500 rpm for 30 seconds in order to obtain a homogeneous texture, which is immediately inserted into the prepared cavity [3].
Biodentine’s chemical composition is based on tricalcium silicate which represents 80% of the powder. Zirconium oxide is included as a radiopacifier, is an inert material and does not participate in the hydration reaction unlike bismuth oxide in MTA, and does not cause color changes in dental tissues. Calcium carbonate represents 15% of the powder, and is a reaction modifier, which allows the early release of calcium ions in solution in larger quantities than unmodified tricalcium silicate. A water-soluble polymer and calcium chloride are incorporated into the liquid component. Calcium chloride reduces setting time. The water-soluble polymer in the liquid has a double role: first, it allows a reduced water-to-powder ratio and results in increased material strength; secondly, it increases the viscosity of the material and improves its handling. The end product of tricalcium silicate hydration is calcium silicate hydrate and calcium hydroxide. The initial setting time declared by the manufacturer is 12 minutes [4].
The antimicrobial potential of Biodentine has been evaluated in numerous studies and compared to other pulp capping materials. Freshly mixed Biodentine was tested against Streptococcus mutans, Enterococcus faecalis, Escherichia coli and Candida albicans, and showed a greater antibacterial effect (p < 0.05) than mineral trioxide aggregate (ProRoot® MTA, Dentsply) and a glass ionomer cement [5]. The hydroxyl ions released during the hydration of Biodentine create an alkaline pH in the environment that has antimicrobial effects. The alkaline pH is also produced by other pulp capping materials such as mineral trioxide aggregate or calcium hydroxide, so the antibacterial mechanism of these materials is similar [6].
In case of injury to the pulp-dentine complex, the pulp’s response can vary from an increase in the synthetic activity of the odontoblast in cases of mild/moderate damage, to the differentiation of odontoblast cells from pulp stem cells in the event of pulp exposure, which leads to the secretion of tertiary dentine. In both cases, the tertiary dentine will serve as protection for the pulp, and the rate of its deposition will largely depend on the severity of the traumatic or carious lesion, the degree of pulpal inflammation, the pulp capping material used and its sealing ability. The regeneration of the pulp-dentine complex is a well-orchestrated process that following the use of Biodentine, consists of the following steps:
Resolution of the inflammation: following the application of Biodentine to the exposed/unexposed pulp, there is a recruitment of inflammatory THP-1 cells, including their adhesion to activated endothelial cells, as well as their migration and activation in macrophage-like cells. This leads to a decrease in the expression of cyclooxygenase-1 and cyclooxygenase-2 - two enzymes involved in the initial phase of inflammation. It also significantly decreases the secretion of two mediators of inflammation: prostaglandin E2 and thromboxane B2.
Neoangiogenesis: stimulation of the expression and secretion of the following factors involved in neoangiogenesis: vascular-endothelial growth factor from pulp stem cells, fibroblast growth factor 2, platelet-derived growth factor, and transforming growth factor β1.
Stimulation of pulpal fibroblasts proliferation: This results from increased secretion of fibroblast growth factor 2 and transforming growth factor β1.
Proliferation and migration of dental pulp stem cells: is orchestrated by growth factors such as transforming growth factor β1, known to stimulate odontoblastic differentiation and the secretion of fibroblast growth factor 2, which induces stem cell proliferation.
Differentiation of stem cells into odontoblast-like cells that will synthesize reparative dentine, with its subsequent mineralization: mesenchymal progenitor cells migrate to the wound area and differentiate into a phenotype with mineralizing capabilities, also known as secondary odontoblasts. These cells deposit hard tissue at the covering site and create a biological closure of the defect, termed a "dentine bridge". The newly formed mineralized tissue is classified as tertiary dentine and is called reparative or reactive dentine [4].
Materials and methods
This article reports a clinical case study of a 22-year-old male who requested dental care with the chief complaint of sensitivity to sweet stimuli in the upper right molar region. The patient underwent clinical and radiological examination. Inspection, probing, percussion, and tests to assess pulp vitality, including cold and electrical sensitivity tests, were performed.
Results
Clinical examination revealed a deep carious cavity in tooth 17. Dental probing was not painful; the dentine had a soft consistency; axial percussion was negative. For cold testing, a cotton pellet soaked in Endo-Frost spray was used, and the response indicated a vital pulp. Additionally, electrical pulp testing was performed with a DigiTest device, recording a value of 16 µA. On the orthopantomography, an extended radiolucency was detected in tooth 17 without communication with the pulp chamber. No pathological periapical findings were found. The final diagnosis was a deep chronic carious lesion, class I cavity by Black.
According to the enhanced treatment protocol proposed by Bjørndal in 2018 [7], a single visit indirect pulp capping of tooth 17 was performed, following these subsequent steps:
Loco-regional anesthesia with Septanest 1:100.000;
Isolation of the working field with rubber dam;
Selective carious cavity preparation – a thin layer of affected dentine was kept;
Cavity disinfection with sodium hypochlorite 5.25% for 10 sec.;
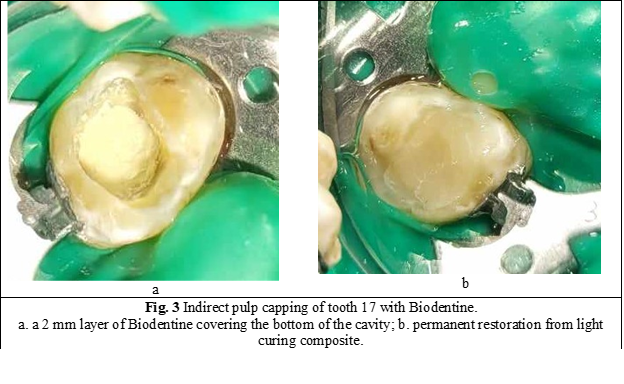
Application of a thin layer of Biodentine on the bottom of the cavity;
Bonding with VI-th generation adhesive system;
Application of a permanent restoration with light curing composite.

Discussions
This clinical case study describes the procedure of indirect pulp capping, which involves the application of a thin layer of bioactive dental material over a thin layer of affected dentine. It is considered that a layer of 0.5 – 1 mm of dentine has an increased number of large dentinal tubules that communicate with the dental pulp, allowing the diffusion of active components of dental materials into the pulp [8]. At the same time, since the pulp was not exposed, it has a very high chance of regeneration if proper treatment is applied.
According to Bjørndal, cases with deep carious lesions require a modified treatment algorithm that includes the removal only of the infected carious tissue, the use of optical magnification, disinfection, and hemostasis with 5.25% sodium hypochlorite, and the use of a hydraulic calcium silicate cement as pulp capping agent [7]. Exactly this algorithm was applied in our clinical case study.
Researchers have shown high rates (95-100%) of clinical success of Biodentine when applied as an indirect or direct pulp-capping agent [9]. This is due to the advantages of the material: appropriate setting time of approximately 12 minutes, easy manipulation, no staining of hard dental tissues, good adhesion to dentine, no dissolution over time, high sealing capacity, high pH, antimicrobial activity, and stimulation of pulp-dentine regeneration process.
The patient was examined at 3 and 6 months after the applied treatment. He no longer presented sensitivity to any irritants. Vitality pulp tests (electrical and cold) confirmed the healthy status of the pulp. On the orthopantomography, a thin layer of newly created tertiary dentine was depicted, and no periapical pathological modifications were found. Our findings correlate with different studies that have shown high success rates of calcium silicate cements in VPT, including Biodentine [9, 10].
Factors contributing to the success of indirect pulp capping could include: establishing the correct pulpal health status before selecting the treatment; proper patient selection – age under 35 and good general health condition; selection of appropriate dental materials for pulp capping and permanent filling; absolute isolation of the tooth with rubber dam from the oral cavity – an environment with a high bacterial load; use of optical magnification and proper disinfection of the prepared cavity, etc.
Conclusions
The indirect pulp capping with Biodentine was considered a success because the main complaint - the sensitivity from sweet stimuli disappeared after the treatment was applied. Also, at the follow-up visits at 3 and 6 months, the cold vitality tests indicated a vital pulp, the electrical pulp testing recorded decreasing values (14 µA and 11 µA respectively), and no pathological periapical radiological modifications were found. In conclusion, we can say that Biodentine exhibited very good handling properties, confirming its status as a promising pulp-capping agent for teeth affected by deep caries.
Competing interests
None declared.
Patient consent
Obtained.
Ethics approval
No approval was required for this study.
Authors’ contribution
Both authors contributed equally to the writing of manuscript. The authors read and approved the final version of the manuscript.
Authors’ ORCID IDs
Diana Trifan – https://orcid.org/0009-0003-7911-1482
Diana Uncuța – https://orcid.org/0000-0001-8172-2854
References
Trifan D, Uncuța D. Caria dentară profundă și particularități de preparare. Materiale curative și tehnici de menținere a vitalității pulpare [Deep dental caries and preparation peculiarities. Curative materials and techniques for maintaining pulp vitality]. Chișinău; 2023. 40 p. Romanian.
Ghoddusi J, Forghani M, Parisay I. New approaches in vital pulp therapy in permanent teeth. Iran Endod J. 2014;9(1):15-22.
Camilleri J. Classification of hydraulic cements used in dentistry. Front Dent Med. 2020;1(9):1-6. doi: 10.3389/fdmed.2020.00009.
About I, editor. BiodentineTM: properties and clinical applications. Berlin: Springer; 2021. 221 p.
Arafa A, Kenawi L, Issa N. Assessment of reparative hard tissue formation after direct pulp capping with Biodentine versus mineral trioxide aggregate. Endod Pract Today. 2019;13(3):227-236.
Bjørndal L, Mjor IA. Pulp-dentine biology in restorative dentistry part 4: dental caries—characteristics of lesions and pulpal reactions. Quintessence Int. 2001;32(9):717-736.
Bjørndal L, Simon S, Tomson PL, Duncan HF. Management of deep caries and the exposed pulp. Int Endod J. 2019;52:949-973. doi: 10.1111/iej.13128.
Peskersoy C, Lukarcanin J, Turkun M. Efficacy of different calcium silicate materials as pulp-capping agents: Randomized clinical trial. J Dent Sci. 2021;16(2):723-731. doi: 10.1016/j.jds.2020.08.016.
Brizuela C, Ormeño A, Cabrera C, et al. Direct pulp capping with calcium hydroxide, mineral trioxide aggregate, and Biodentine in permanent young teeth with caries: a randomized clinical trial. J Endod. 2017;43(11):1776-1780. doi: 10.1016/j.joen.2017.06.031.
Katge FA, Patil DP. Comparative analysis of 2 calcium silicate-based cements (Biodentine and Mineral Trioxide Aggregate) as direct pulp-capping agent in young permanent molars: a split mouth study. J Endod. 2017;43(4):507-513. doi: 10.1016/j.joen.2016.11.026.