Introduction
Being part of the five most frequently encountered syndromes in surgical practice, cholestatic jaundice syndrome in the specialized literature is exposed in both benign and malignant pathologies. According to existing data in the literature, the presence of cholestatic jaundice in the complications of gallstones is reported in 10-20% of cases, with choledocholithiasis as the main cause but also being characteristic of acute biliary pancreatitis, acute cholecystitis, cholangitis [1-2]. Although significant progress has been made in recent years in the diagnosis and treatment of mechanical jaundice syndrome in gallstones, there are still many problems and challenges [3-5]. Considered a medical-surgical emergency, cholestatic jaundice syndrome requires a surgical approach as early as possible, but in some cases, biliary decompression, carried out both by laborious surgical interventions and by endoscopic methods, induces a worsening of the patient's condition with the installation of some severe evolutionary complications, caused by existing homeostatic disturbances [6].
In the current concepts of publications on the subject, cholestatic jaundice installed in gallstones is considered a multifactorial pathogenetic process. It is known that obstructive cholestasis induces serious functional disorders of homeostasis, causing the suppression of the metabolic activity of the liver, inhibiting the immune system and hemostasis mechanisms, reducing over time the excretory function of the kidneys, and limiting the barrier function of the digestive tract [7]. These data are an argument that the severity of the pathological condition is determined by a common link, consisting of the endogenous intoxication syndrome (EI) characteristic of the complications of gallstones and the occurrence in these conditions of systemic oxidative stress (OS). The level of “peptides with average mass” (PAM) is considered a universal biomarker of EI [8]. PAM are components with high biological activity and a polyfunctional spectrum of action that are formed upon the intensification of non-enzymatic proteolysis, including blood protein proteolysis. An essential feature of PAM is the increased biological capacity of the compounds in this group, the action of which further aggravates the existing metabolic disorders, inducing their continuous formation with the appearance of a “vicious circle”. The severity of endotoxemia reflects the imbalance between the formation of endotoxins and the body's capacities for their transformation and biological elimination [8, 9]. In turn, OS develops because of the imbalance between the hyperproduction of active forms of oxygen and the insufficiency of the body's antioxidant capacity, which usually increases suddenly in various toxic states [10]. Based on existing studies aimed at the pathogenesis of the disturbances produced by cholestatic jaundice, the importance of the influence of free radicals that ultimately induce hepatocyte damage is proven [10-12].
However, the analysis of the literature reveals few studies with reference to the role of endogenous intoxication in the occurrence of systemic oxidative stress in cholestatic jaundice associated with gallstone complications. Additionaly, the available literature data do not contain information that aims at the deviations of oxidative stress depending on the degree of hepatic endogenous intoxication present in different complications of gallstones.
Material and methods
The clinical research was carried out within the Nicolae Anestiadi Department of Surgery of Nicolae Testemițanu State University of Medicine and Pharmacy. The study included the investigation of 105 patients with complicated gallstones and associated cholestatic jaundice, and the control group consisted of 35 patients with uncomplicated gallstones. Depending on the evolutionary complications present, the patients from the core investigation batch were divided into 3 homogeneous groups: group 1 – chronic gallstones and cholestatic cholemia (n = 35), group 2 – acute lithiasic cholecystitis, cholangitis, and cholestatic cholemia (n = 35), group 3 – acute biliary pancreatitis and cholestatic cholemia (n = 35). The age of the patients varied between 51 and 72 years. The female/male ratio was estimated to be 3/1. The criteria for including patients in the basic group were the presence of gallstones in the complication phase, associated with cholestatic jaundice, confirmed by diagnostic parameters:
clinical – history of gallstones or biliary colic at onset, presence of skin jaundice;
paraclinical – laboratory characteristic tests – elevated values of serum bilirubin, specifically the direct fraction, elevated values of alkaline phosphatase, elevated values of leukocytes, fibrinogen, serum urea, amylase, as well as marked values of ALAT; and imaging confirmation of gallstones and the diameter of the main bile duct > of 0.8 cm.
Cases that met the stated criteria were included in the study. Blood samples were collected during hospitalization until the start of treatment and after biliary decompression. Endogenous intoxication, ascertained by the values of peptides with average mass (PAM), was determined according to the procedure by Gabrielian N.I. et al. (1984) [13]. The comparative evaluation of systemic OS in groups was performed by assessing the correlation in the blood serum between the intensity of peroxidic oxidation of lipids (POL) and the antioxidant potential (AP). The intensity of POL was determined by the values of the final product of lipoperoxidation – malonic dialdehyde (MDA), assessed according to the procedure modified by Gudumac V. et al. (2010) [14]. The antioxidant potential was expressed by superoxide dismutase (SOD) and catalase (CAT) values. SOD activity was estimated according to the procedures modified by Gudumac V., Tagadiuc O. et al. (2010) [15]. CAT activity was determined according to the method modified by Baciu E. and Nastas I. (1996) [16].
The data of each case were recorded in a standardized form and processed using the operative methods of statistical evaluation of the computer program Windows 2010 (GraphPad Software, Inc.) and Excel (Microsoft®, USA) 2010, Medcalc. The obtained results were compared and reported in relation to the values of the parameters of the control batch; also, the deviations of the values in the batches were compared. The statistical analysis was performed applying the Mean (M), Mean Error (m), Dispersion, Standard Deviation, Asymmetry (Skew), Coefficient of variation (%), and T-Student statistic test. The discrepancy with the margin of error <5% was considered statistically significant (p < 0.05). For paired group comparisons, the ANOVA test and the Tukey HSD test were used.
Results
The analysis of the examination results confirms the homogeneity of the groups depending on age and concomitant pathologies, with an insignificant difference in group II [p c/1 < 0.05 (t = 2.55); p c/2 > 0.05 (t = 1.10); p c/3 < 0.01 (t = 2.84)]. The homogeneity of the groups is also with insignificant deviations between groups I and II [p 1/2 > 0.05 (t = 1.64); p 1/3 < 0.01 (t = 4.55); p 2/3 < 0.01 (t = 3.31)]. An earlier hospitalization of patients was highlighted in groups II and III, caused by the presence in these patients of the painful, progressive inflammatory component, an important factor that contributes to the reduction of the duration of jaundice until hospitalization with data of medium-grade jaundice [p 1/2 < 0.001 (t = 3.5); p 1/3 < 0.001 (t = 9.6); p 2/3 < 0.001 (t = 8.6)]. Survey data and results of laboratory parameters in the study groups and the control group at hospitalization are presented in Table 1.
Table 1. Survey data and results of laboratory parameters at hospitalization. | |||||||
Control group (n=35) | Group 1 (n=35) | Group 2 (n=35) | Group 3 (n=35) | p1/2 | p1/3 | p2/3 | |
Age | 59.1±1.12 | 64.2±1.65* | 61.4±1.75 ****
| 53.1±1.79** | p>0.05 t=1.64 | p<0.01 t=4.55 | p<0.01 t=3.31 |
Duration of jaundice | 0 | 4.44±0.38 | 3.19±0.19 | 1.48±0.06 | p<0.001 (t=3.5) | p<0.001 (t=9.6) | p<0.001 (t=8.6) |
Temperature (°C) | 37±0.5 | 37±0.5**** | 38±0.5**** | 37±0.5**** | p>0.05 (t=1.41) | p>0.05 (t=0) | p>0.05 (t=1.41) |
Alkaline phosphatase (U/I) | 149.8±12.4 | 881.14±78.3*** | 541.4±34.6*** | 760.0±83.0*** | p<0.001 (t=3.9) | p>0.05 (t=1.06) | p<0.05 (t=2.4) |
Total bilirubin (mmol/l) | 12.1±0.79 | 119.31±8.7*** | 78.55±5.3*** | 80.28±4.9*** | p<0.01 (t=4.0) | p<0.01 (t=3.9) | p>0.05 (t=0.2) |
Direct bilirubin (mmol/l) | 4.2±0.06 | 88.2±6.7*** | 56.2±4.2*** | 54.8±3.4*** | p<0.01 (t=4.0) | p<0.01 (t=4.4) | p>0.05 (t=0.3) |
ALAT (U/l) | 19.57±0.97 | 128.7±8.2*** | 207.1±12.1*** | 289.62±9.4*** | p<0.001 (t=5.3) | p<0.001 (t=12.9) | p<0.001 (t=5.4) |
Blood amylase (U/l) | 34.57±1.4 | 37.9±1.9**** | 43.1±2.3**** | 164.9±9.7*** | p>0.05 (t=7.4) | p<0.001 (t=12.8) | p<0.001 (t=12.2) |
Fibrinogen (U/L) | 2.69±0.06 | 3.52±0.1*** | 4.21±0.1*** | 4.43±0.17*** | p<0.01 (t=4.87) | p<0.01 (t=4.61) | p>0.05 (t=1.1) |
Blood leukocytes (n) | 6.23±0.23 | 7.51±0.31** | 12.12±0.52*** | 10.24±0.43*** | p<0.01 (t=7.61) | p<0.01 (t=5.15) | p<0.01 (t=2.78) |
Neutrophil (n) | 3.86±0.22 | 7.5±0.39*** | 13.1±0.43*** | 9.9±0.56*** | p<0.01 (t=12.5) | p<0.001 (t=3.74) | p<0.01 (t=5.31) |
Urea (U/l) | 6.23±0.21 | 6.56±0.24**** | 7.0±0.21* | 7.92±0.47** | p>0.05 (t=1.37) | p<0.05 (t=2.57) | p>0.05 (t=1.78) |
Creatinine (U/l) | 68.8±1.19 | 81.0±3.5** | 86.58±3.2** | 82.17±2.8** | p>0.05 (t=1.17) | p>0.05 (t=0.26) | p>0.05 (t=1.03) |
Note: p<0.05*; p<0.01**; p<0.001***; p>0.05**** - compared to the values of the control group; Group1 - chronic gallstones and cholestatic cholemia; Group 2 - acute lithiasic cholecystitis, cholangitis and cholestatic cholemia; Group 3 - acute biliary pancreatitis and cholestatic cholemia; p1/2 - compared to the values of the group 1 to 2; p1/3 - compared to the values of the group 1 to 3; p2/3 - compared to the values of the group 2 to 3; ALAT – alanine aminotransferase; t - test used to compare the means of two independent samples. | |||||||
Examination of the levels of biochemical markers of cholestasis reported a statistically significant difference in all study groups compared to the control group, confirming the existing homeostatic disturbances: alkaline phosphatase [p < 0.001 (t = 8.2); (t = 3.9); (t = 7.27)], direct bilirubin [p < 0.001 (t = 12.5); (t = 12.3); (t = 14.9)]. The comparative examination of parameters in groups shows an insignificant difference of alkaline phosphatase in groups 1 and 3 [p > 0.05 (t = 1.06)] and direct bilirubin in groups 2 and 3 [p > 0.05 (t = 0.3)]. However, according to the examinations, the severity of the liver disease is correlated with the markers of the inflammation syndrome - elevated values of fibrinogen, blood leukocytosis, neutrophils with a significant statistical difference (p < 0.001), more evident in groups 2 and 3 (Fig.1).
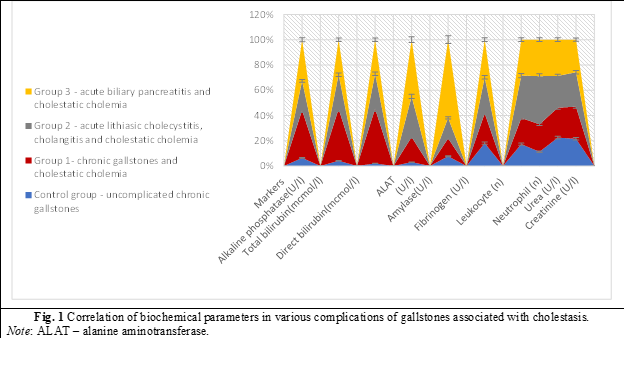
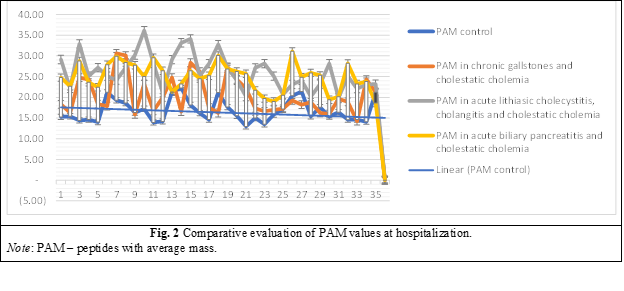
Also, the degree of endotoxemia assessed at hospitalization by PAM values was consistent with the inflammation present in groups 2 and 3, reporting a statistically significant difference compared to the control group [p c/2 < 0.001(t = 11.1); p c/3 < 0.001(t = 11.07)], regardless of the fact that the values of cholestasis markers in these groups were lower (Fig. 2).
Using the ANOVA test for the comparison of groups also confirmed a statistically significant difference with a p < 0.00001 for an F = 15.06988. The Tukey HSD test for pairwise group comparisons showed a negative Q with no statistical difference only in the comparison of group II and III, both with a marked inflammatory syndrome (Table 2).
Table 2. Pairwise Comparison of Endotoxemia (Tukey HSD Test). | ||
Pairwise Comparison | HSD.05 = 8.5102 HSD.01 = 10.3447 | Q.05 = 3.6554 Q.01 = 4.4434 |
C – Gr 1 | 21.31 | Q = 9.39 (p = .00000) |
C – Gr. 2 | 9.60 | Q = 4.23 (p = .01595) |
C – Gr.3 | 12.89 | Q = 5.68 (p = .00044) |
Gr.1 – Gr.2 | 11.71 | Q = 5.16 (p = .00178) |
Gr.1 – Gr.3 | 8.43 | Q = 3.71 (p = .04488) |
Gr.2 – Gr.3 | 3.29 | Q = 1.45(p = .73573) |
Note: HSD – honestly significant difference; Q negative – blue color; C – control group; Gr.1 – chronic gallstones and cholestatic cholemia; Gr. 2 – acute lithiasic cholecystitis, cholangitis, and cholestatic cholemia; Gr.3 – acute biliary pancreatitis and cholestatic cholemia. | ||
MDA as the final product of lipid peroxidation, evaluated at hospitalization, shows double marked values in all groups, compared to the control group [p < 0.001 (t = 10.7); (t = 10.9); (t = 16.5)] (Fig. 3).
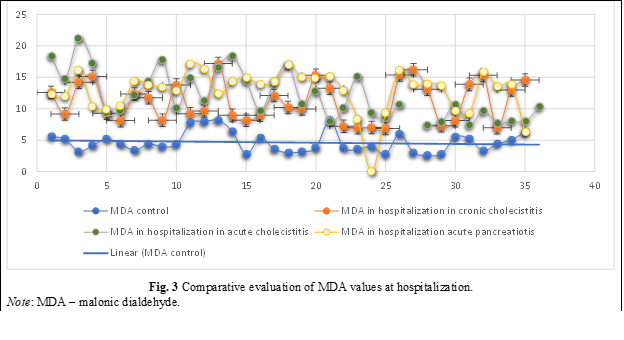
The ANOVA and Tukey HSD comparison test in paired groups reported that in the presence of a marked lipoperoxidation, regardless of the complication associated with gallstones, a negative Q is found without statistical difference in all study groups, with minimal value disproportions (Table 3).
Table 3. Pairwise comparison of MAD in subgroups at hospitalization (Tukey HSD test). | ||
Pairwise comparison | HSD.05 = 13.0262 HSD.01 = 15.8343 | Q.05 = 3.6554 Q.01 = 4.4434 |
Gr.1 – Gr.2 | 5.03 | Q = 1.41 (p = .75078) |
Gr.1 – Gr.3 | 6.84 | Q = 1.92 (p = .52697) |
Gr.2 – Gr.3 | 1.81 | Q = 0.51 (p = .98400) |
Note: HSD – honestly significant difference; Q negative – blue color; Gr.1 – chronic gallstones and cholestatic cholemia; Gr. 2 – acute lithiasic cholecystitis, cholangitis, and cholestatic cholemia; Gr.3 – acute biliary pancreatitis and cholestatic cholemia. | ||
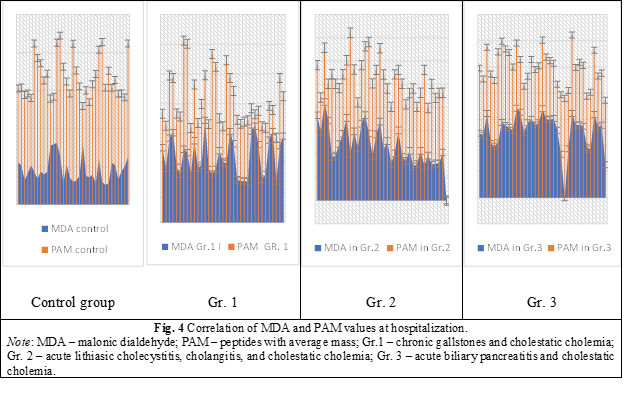
The assessment in the study of the correlation of lipid peroxidation with the degree of endogenous intoxication reported a direct dependence of the increase in PAM parameters with the elevation of DAM (Fig. 4).
Antioxidant activity, assessed at hospitalization by superoxide dismutase and catalase values, shows a statistically significant decrease in both SOD values [p < 0.001 (t = 6.4); (t = 4.1); (t = 5.7)] as well as CAT [p < 0.001 (t = 6.7); (t = 5.6); (t = 7.2)] in all groups, by 30-40% compared to the control group.
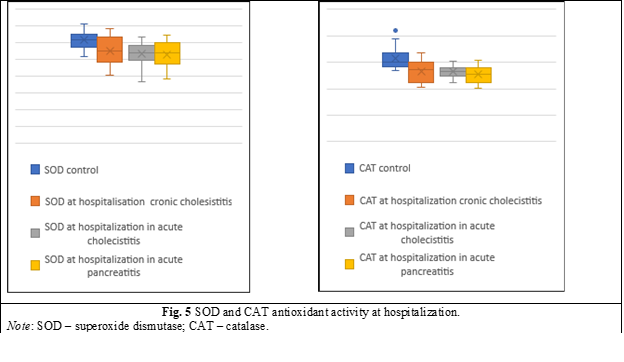
However, the ANOVA comparison test in paired groups and the Tukey HSD Test showed a negative Q with a statistically insignificant difference (p > 0.05), confirming that in all complications, the antioxidant system is compromised without major value differences (Table 4).
Table 4. Pairwise Comparison of SOD and CAT in groups at hospitalization (Tukey HSD Test). | |||||
Pairwise Comparison of SOD | HSD.05 = 239.0962 HSD.01 = 90.6385 | Q.05 = 3.6554 Q.01 = 4.4434 | Pairwise Comparison of CAT | HSD.05 = 12.1089 HSD.01 = 14.7192 | Q.05 = 3.6554 Q.01 = 4.4434 |
Gr.1 – Gr.2 | 13.94 | Q = 0.21 (p = .99878) | Gr.1 – Gr.2 | 0.47 | Q = 0.14 (p = .99963) |
Gr.1 – Gr.3 | 16.40 | Q = 0.25 (p = .99802) | Gr.1 – Gr.3 | 0.47 | Q = 0.14 (p = .99963) |
Gr.2 – Gr.3 | 2.46 | Q = 0.04 (p = .99999) | Gr.2 – Gr.3 | 0.01 | Q = 0.01 (p = .00001) |
Note: SOD – superoxide dismutase; CAT – catalase; HSD – honestly significant difference; Q negative – blue color; Gr.1 – chronic gallstones and cholestatic cholemia; Gr. 2 – acute lithiasic cholecystitis, cholangitis and cholestatic cholemia; Gr. 3 – acute biliary pancreatitis and cholestatic cholemia. | |||||
The correlation of endogenous liver intoxication with the reaction of the pro- and antioxidant system characteristic for various complications of gallstones associated with cholestatic jaundice is presented in numerical values in Table 5.
Table 5. Evaluation of the degree of endotoxemia and systemic oxidative stress in groups at hospitalization. | |||||||
Markers | Control group (n = 35) | Group 1 (n = 35) | Group 2 (n = 35) | Group 3 (n = 35) | p1/2 | p1/3 | p2/3 |
MDA | 4.62±0.27 | 11.12±0.53*** | 12.11 ± 0.64*** | 13.16±0.44*** | p>0,05 (t=1.19) | p<0,01 (t=2.96) | p>0,05 (t=1.35) |
SOD | 1230.74±16.39 | 1096.97±27.4*** | 1060.91±21.05*** | 1057.44±25.2*** | p>0,05 (t=1.04) | p>0,05 (t=1.06) | p>0,05 (t=0.11) |
CAT | 15.79±0.33 | 13.17±0.33*** | 13.27±0.14*** | 12.62±0.25*** | p>0,05 (t=0.29) | p>0,05 (t=1.3) | p>0,05 (t=1.41) |
PAM | 16.77±0.45 | 20.4±0.75*** p<0.001 (t=4.1) | 26.16±0.71** p<0.001 (t=11.1) | 24.81±0.57** p<0.001 (t=11.07) | p<0,01 (t=5.5) | p<0,01 (t=4.68) | p>0,05 (t=1.48) |
Note: *: p<0.05*; p<0.01**; p<0.001***; p>0.05**** – compared to the values of the control group; Gr.1 – chronic gallstones and cholestatic cholemia; Gr. 2 – acute lithiasic cholecystitis, cholangitis, and cholestatic cholemia; Gr. 3 – acute biliary pancreatitis and cholestatic cholemia; MDA – malonic dialdehyde; SOD – superoxide dismutase; CAT – catalase; PAM – peptides with average mass; p1/2 – compared to the values of the group 1 to 2; p1/3 – compared to the values of the group 1 to 3; p2/3 – compared to the values of the group 2 to 3; ALAT – alanine aminotransferase; t - test used to compare the means of two independent samples. | |||||||
Discussions
The liver has a wide variety of metabolic functions, due to which liver dysfunction is associated with various clinical-pathological sequelae. Dysregulation of liver metabolism activates mechanisms that cause the accumulation of toxic products and the installation of variable endogenous intoxication in different pathologies [17]. The concept of “endogenous intoxication” for a long time did not have a biochemical substrate for research, which is why it could not be measured quantitatively. Currently, several homeostasis indicators and parameters are considered markers of endogenous intoxication: bilirubin, transaminases, proteases and their inhibitors, fibrinogen, haptoglobin, ceruloplasmin, C-reactive protein, creatinine, urea, total protein levels and parameters, proteinograms, ESR, cellular, humoral characteristics, etc. However, the values of these indicators are important only in complex with other criteria, which can vary depending on the etiology of toxemia. It is impossible to adequately assess the degree of intoxication based on one of them, and defining all of them is very laborious and difficult from an economic point of view [8, 18]. Recent studies have demonstrated that, as a universal biochemical marker of EI, necessary to objectify the toxicity of a certain environment, regardless of etiopathogenetic characteristics, the level of “average molecules” can be considered. There is an opinion that the level of PAM primarily reflects the degree of altered protein metabolism and correlates with clinical and laboratory prognostic criteria for metabolic disorders [19]. Characteristic for the mechanical jaundice syndrome, PAM is considered the main group of endotoxins that determine the development of endogenous intoxication. Possessing diverse biological activity and contributing to the inhibition of enzyme systems, the disturbance of ionic membrane permeability, and the fixation and suppression of vitally necessary protein synthesis processes, PAM induce the development of endogenous intoxication, which, in the end, can evolve into hepatocellular insufficiency with alterations in the functions of various systems and organs [9, 19].
According to the results of our own research, the PAM level in cholestatic cholemia, present in the complications of gallstones, was increased in all groups, being more evident in the groups with the presence of acute inflammation (group 2) with an increase of 26.7%, and the enzymatic component supporting inflammation (group 3) with a 22.5% increase. Regardless of the presence of higher bilirubin parameters in group 1, the PAM values reported a less significant increase - only by 5.78%. These results are consistent with existing literature data, which show a percentage of increase – 29.5-39.7%, but without a specification characteristic of different groups of complications [8, 19]. As a rule, in the available literary sources, we found only the fact of increasing the PAM level in the blood (plasma, erythrocytes) of patients with mechanical jaundice, without differentiation in different clinical groups.
Several studies report that the development of endogenous intoxication in liver diseases of different genesis is largely due to a change in the ratio between lipid peroxidation products and the enzymes that cause their deactivation [20]. The presence of an increased number of free radicals can be considered as one of the triggering pathogenetic factors in the progression of pathological changes in the liver in patients with cholestatic jaundice [12, 21].
The present study confirms massive lipoperoxidation in all benign complications of gallstones associated with cholestatic jaundice, showing an increase in MDA values as the end product of peroxidation in all groups, being more evident in the groups with the presence of the enzymatic component supporting inflammation (group 3) – a 2.84-fold increase compared to the values of the control group and in the presence of acute inflammation (group 2) – a 2.6-fold increase. MDA values in group I reported a 2.4-fold increase over control group values. Also, the study confirmed the direct dependence of the PAM and MDA ratio, which is higher in patients with cholestatic jaundice and associated infectious complications, being an indication for biliary decompression as early as possible in these patients.
In various pathological conditions, including cholestatic jaundice, the acceleration of the formation of free radicals induces an imbalance between the prooxidant factors and the protective antioxidant systems, in which the prooxidant factors constitute a specific aggravating factor. The antioxidant system (AS) has the function of limiting the excess of free radicals in the body, acting preventively and creating positions to stop the progression of the harmful effects of free radicals [11, 22]. AS acts by maintaining the regulation mechanisms of the pro- and antioxidant balance, favoring conditions for the body to fight effectively in various pathological situations, limiting injuries and their extension [10, 11, 22]. The balance between the prooxidant action of free radicals and the level of antioxidants is essential to life and characterizes the resistance capacity of an organism [23].
According to our own results, in gallstone cholestatic jaundice, regardless of the type of condition, the antioxidant system is mobilized from the first hours of the appearance of the complication and the association of jaundice, but prooxidant activity and endotoxemia are prevalent, contributing to the inhibition of the antioxidant system. Antioxidant activity, assessed at hospitalization by superoxide dismutase and catalase values, shows a statistically significant decrease in all groups: group 1 – CAT < 16.7%, SOD < 10.9%; group 2 – CAT < 15.9%, SOD < 13.7%; group 3 – CAT < 20.1%, SOD < 14.1%, compared to the control batch. The publications on the subject do not present a valuable exposition of the deviations of the investigated parameters in different complications of gallstones associated with cholestatic jaundice but mention the early inhibition of antioxidant activity in the mechanical jaundice syndrome [12, 24].
Conclusions
The syndromic evaluation of liver activity in the complications of gallstones associated with cholestatic jaundice reveals the elevation of the values of the parameter characteristic for cholestasis and liver mesenchymal inflammation syndromes, which have an impact on the evolution of liver synthesis function and liver cytolytic disorders. In established cholestatic jaundice, there is an obvious activation of lipoperoxidation processes, which contributes to the increase of endogenous intoxication and early suppression of antioxidant activity. There is a direct linear relationship in the increase of prooxidant activity and the level of endogenous intoxication, in all complications of gallstones associated with cholestatic jaundice, but being more elevated in infectious complications, serving as an indication for an early solution.
Competing interests
None declared.
Patient consent
Obtained.
Ethics approval
The study was initiated before the creation of the Research Ethics Committee at Nicolae Testemițanu State University of Medicine and Pharmacy, so the study was approved by the scientific council and the patient's informed consent was obtained.
Authors' contributions
All the authors have contributed equally to the results presentation in the paper.
Authors’ ORCID IDs
Liuba Streltov – https://orcid.org/0000-0002-8560-1264
Valentin Gudumac – https://orcid.org/0000-0001-9773-1878
Gheorghe Rojnoveanu – https://orcid.org/0000-0001-7075-4113
References
Shabanzadeh DM. Incidence of gallstone disease and complications. Curr Opin Gastroenterol. 2018;34(2):81-89. doi: 10.1097/MOG.0000000000000418.
Pain JA, Cahill CJ, Bailey ME. Perioperative complications in obstructive jaundice: therapeutic considerations. Br J Surg. 1985;72(12):942-945. doi: 10.1002/bjs.1800721203.
Duca S. Tratamentul miniinvaziv al litiazei CBP [Mini-invasive treatment of CBP lithiasis]. In: Chirurgia laparoscopica [Laparoscopic surgery]. Bucuresti: Paralela 45; 2001. p. 209-247. Romanian.
Hotineanu V, Ferdohleb A, Hotineanu A. Strategia chirurgicala in rezolvarea icterului obstructiv benign [The surgical strategy in resolving benign obstructive jaundice]. Chirurgia. 2005;100(3):241-250. Romanian.
Taylor A, Stapley S, Hamilton W. Jaundice in primary care: a cohort study of adults aged >45 years using electronic medical records. Fam Pract. 2012;29(4):416-420. doi: 10.1093/fampra/cmr118.
Pavlidis ET, Pavlidis TE. Pathophysiological consequences of obstructive jaundice and perioperative management. Hepatobiliary Pancreat Dis Int. 2018;17(1):17-21. doi: 10.1016/j.hbpd.2018.01.008.
Czabanka M, Peter C, Martin E, et al. Microcirculatory endothelial dysfunction during endotoxemia-insights into pathophysiology, pathologic mechanisms and clinical relevance. Curr Vasc Pharmacol. 2007;5(4):266-275. doi: 10.2174/157016107782023389.
Malakhova MIa. Endogennaia intoksikatsiia kak otrazhenie kompensatornoi perestroiki obmennykh protsessov v organizme [Endogenous intoxication as a reflection of compensatory restructuring of metabolic processes in the body]. [Efferent therapy]. 2000;6(4):3-14. Russian.
Buniatian ND, Vlasov AP, Nachkina EI, Kochkarova RR, Shibitov VA, Kargaeva TN, Nazarov AL, Naumova EA. Funktsional’no-sistemnye reaktsii organizma pri endotoksikoze i ikh korrektsiia [Functional-systemic reactions of the body in endotoxicosis and their correction]. Pharmacy. 2011;(6):43-46. Russian.
Vladimirov YA, Proskurnina EV. Free radicals and cell chemiluminescence. Biochemistry (Moscow). 2009;74(13):1545-1566. doi: 10.1134/s0006297909130082.
Simon HU, Haj-Yehia A, Levi-Schaffer F. Role of reactive oxygen species (ROS) in apoptosis induction. Apoptosis. 2000;5(5):415-418. doi: 10.1023/a:1009616228304.
Silina EV, Stupin VA, Abramov IS, Bolevich SV, Deshpande G, et al. Oxidative stress and free radical processes in tumor and non-tumor obstructive jaundice: influence of disease duration, severity and surgical treatment on outcomes. Pathophysiology. 2022;29(1):32-51. doi: 10.3390/pathophysiology29010005.
Gabrielian NI, Lipatova VI. Opyt ispol’zovaniia pokazatelia srednikh molekul v krovi dlia diagnostiki nefrologicheskikh zabolevanii u detei [Experience in the use of the median molecule index of blood to diagnose kidney diseases in children]. Lab Delo. 1984;(3):138-40. Russian.
Gudumac V, Tagadiuc O, Rîvneac V, SardarI V, Pantea V. Investigații biochimice de laborator: elaborare metodică. Vol. 2: Micrometode. [Laboratory biochemical investigations: methodical guidelines. Vol. 2: Micromethods]. Chişinău: Elena VI; 2010. 104 p. Romanian.
Tagadiuc O, Gudumac V, Pantea V, inventors. Procedeu de dozare a activității superoxiddismutazei [Superoxide dismutase activity assay procedure]. Republic of Moldova patent no. 4891. 2010 July 15. Romanian.
Baciu E, Nastas I, inventors. Procedeu de determinare a activității catalazei [Method for determination of catalase activity]. Republic of Moldova patent no. 3122. 1996 Nov 9. Romanian.
Vagholkar K. Obstructive jaundice: understanding the pathophysiology. Int J Surg Med. 2020;6(4):26-31.
Afanas’eva AN. Sravnitel’naia otsenka urovnia endogennoi intoksikatsii u lits raznykh vozrastnykh grupp [Comparative assessment of the level of endogenous intoxication in persons of different age groups]. Clin Lab Diagn. 2004;(6):11-12. Russian.
Kariakina EV, Belova SV. Molekuly srednei massy kak inegral’nyi pokazatel’ metabolicheskikh narushenii [Molecules of average mass as an integral indicator of metabolic disorders]. Clin Lab Diagn. 2004;(3):3-8. Russian.
Jakus V, Lopuchova M. Role of free radicals, oxidative stress and antioxidant systems in liver diseases. Bratisl Lek Listy. 1999;100(10):548-559.
Guiotto A, Ruzza P, Babizhayev MA, Calderan A. Malondialdehyde scavenging and aldose-derived Schiff bases transglycation properties of synthetic histidyl-hydrazide carnosine analogs. Bioorg Med Chem. 2007;15(18):6158-6163. doi: 10.1016/j.bmc.2007.06.029.
Chen J, Wu F, Long Y, Yu W. Glutathione supplementation attenuates oxidative stress and improves vascular hyporesponsiveness in experimental obstructive jaundice. Oxidative Med Cell Longev. 2015;2015:486148. doi: 10.1155/2015/486148.
Busch CJ, Binder CJ. Malondialdehyde epitopes as mediators of sterile inflammation. Biochim Biophys Acta Mol Cell Biol Lipids. 2017;1862(4):398-340. doi: 10.1016/j.bbalip.2016.06.016.
Bolevich SB, Stupin VA, Gakhramanov TV, Khokonov MA, Silina EV, Menshova NI, Bogdanova LS. Free radical processes at patients with pathologies of biliary ducts and methods of their correction. Khirurgiia (Moscow). 2010;7:65-70.