Introduction
The infection with the SARS-CoV-2 virus caused a pandemic lasting more than 3 years and its worldwide impact was reflected in all fields, leaving long-lasting consequences. AAP (American Academy of Pediatrics) epidemiological data showed that children represent 18.3% of all cases of COVID-19 infection in a study of global statistics [1]. The clinical expression of COVID-19 infection ranges from asymptomatic disease with mild respiratory tract symptoms to severe pneumonia with acute respiratory distress syndrome and multiorgan dysfunction [2]. Compared to adult patients with COVID-19 infection, children have a milder clinical course, fewer radiological changes, and shorter convalescence time [3]. However, bronchopulmonary complications can occur even in cases of asymptomatic infection or mild form of the disease [4].
According to the latest studies presented in the specialized literature, approximately 25% of children who suffered the infection of COVID-19 experience sequelae with various manifestations [5]. Contemporary diagnostic imaging methods of high sensitivity, such as lung CT, allow to establish the degree of lung damage, the volume, and the sequelae arising from enduring the COVID-19 infection. The long-term consequences of the COVID-19 infection are still researched. Pneumonia in the infection of COVID-19 can lead to the long-term development of pulmonary fibrosis and bronchiectasis [6]. Thus, it is important to monitor patients with COVID-19 over time to assess the progression to irreversible fibrotic lung disease and its impact on respiratory symptoms, quality of life, and mortality [7].
Clinical case
We present the clinical case of a 5-month-old boy admitted to the Pneumology Clinic of the Mother and Child Institute in Chisinau.
At the age of 4 months, the child suffered the severe evolution of the COVID-19 infection. He was hospitalized in the specialized section for COVID-19 infections within the Mother and Child Institute. The child presented to the emergency room with a fever of 38.5°C, signs of respiratory catarrh, rare dry cough, tachypnea with 58-60 breaths per minute, SpO2 – 94%, dyspnea, intercostal draft, acrocyanosis, refusal to eat, sleepiness. From the history of the disease, the child is considered sick for 2 days, with fever up to 38.9°C, difficult breathing, agitation. The reason for referral was the persistent febrile syndrome, which did not respond to the administration of antipyretics. From the epidemiological anamnesis, it is known that the child's mother showed signs of respiratory infection during the last 3-4 days. The objective examination of the child showed a serious general condition, he was apathetic with signs of respiratory failure.
During laboratory examinations, grade I anemia is attested (hemoglobin - 98 g/l, erythrocytes 3.2x106/µL, hematocrit - 26%); leukopenia (leukocytes – 4.4x109/L); lymphopenia (lymphocytes – 27%); accelerated ESR – 11mm/h; elevated liver transaminases (ALT – 82.8 U/l AST – 83.1 U/l); C-reactive protein – negative.
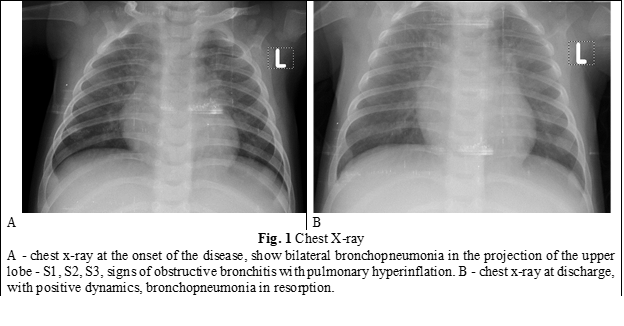
X-ray of the chest confirmed the bronchopulmonary damage with the following conclusion – Bilateral bronchopneumonia in the projection of the upper lobe - S1, S2, S3, signs of obstructive bronchitis with pulmonary hyperinflation (fig. 1 A). Taking into consideration the specialized care and treatment, clinical-imaging evolution with positive dynamics was attested with the reduction of pulmonary infiltration and the involution of clinical signs (fig. 1 B). The patient was discharged home after 6 days with recovery recommendations.
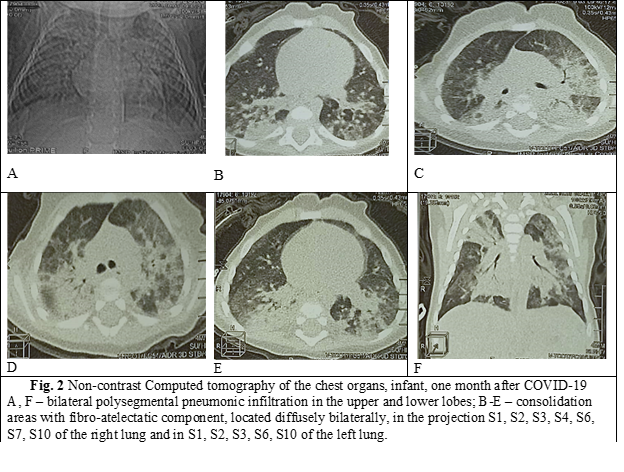
More than a month after suffering COVID-19 infection, the patient goes to the Pneumology clinic with complaints of semi-productive cough, difficult breathing, and loss of appetite. These symptoms surfaced about a week ago. Despite the background of symptomatic treatment, the child's general condition worsens due to toxic-infectious signs, respiratory failure. At admission, the child is agitated, has tachypnea with 53-57 breaths per minute, SpO2 90-92%, mixed dyspnea, subcostal draft, acrocyanosis, food refusal. Taking into consideration the serious general condition, the complaints and the anamnestic of the disease, the child was admitted to the intensive care unit for specialized treatment. Later, after stabilization of the general condition and clinical signs, a computed tomography of the chest without contrast was performed (fig. 2). The tomographic sections, performed in the pulmonary and mediastinal mode, highlight: consolidation areas by hyperattenuation type, with atelectatic component, located diffusely bilaterally, in the projection S1, S2, S3, S4, S6, S7, S10 of the right lung and in S1, S2, S3, S6, S10 of the left lung, with irregular border, inhomogeneous and with partial visualization of the air bronchogram. Deformation of the anatomical architecture of the lung parenchyma is present. Diffuse bilateral peribronchial thickening is observed, more pronounced at the level of the main and segmental bronchi, associated with narrowing of the lumen of the main and segmental bronchi. Trachea, main and segmental bronchi are permeable. The lung fields are transparent. The costo-diaphragmatic sinuses are free. The pleura shows thin sheets, without fluid collections and pathological thickenings. Heart and major vessels have normal CT appearance. The arterial ligament is calcified. The thymus is placed in the region of the anterior mediastinum, the dimensions correspond for the age, with usual configuration, clearly outlined, homogeneous, with the native density +65UH. Volume formations in both lung fields and in the projection of the mediastinum are not determined. Enlarged mediastinal lymph nodes are not determined. Diaphragm with clear outline, without pathological changes. Tomographic images are suggestive for bilateral polysegmental pneumonic infiltration with severe fibro-atelectatic component, signs of chronic bronchitis.
Discussion
COVID-19 infection affects people of any age or gender. Among the pediatric population, serious forms of the disease are less common, fewer complications and a shorter recovery period [8]. According to data from specialized literature, children up to 6 months of age have a major risk of developing a severe form of the infection [9]. Young age can be an unfavorable predictor in the development of post-COVID19 schools. These circumstances are also present in the clinical case of this infant with COVID-19 infection. Computed tomography data suggest fibro-atelectatic changes in both lungs, predominantly in the apical and basal segments. Once triggered, pulmonary fibrosis leaves worrisome sequelae in children, as lung architectural distortions and irreversible lung dysfunction develop [10]. Taking into account that the occurrence of sequelae is unpredictable, the infection of COVID-19 in the pediatric population requires continuous monitoring by multidisciplinary teams with the involvement of pediatric pulmonologists and imaging techniques, especially by pulmonary CT.
Conclusions
Infants showed an increased vulnerability to the appearance of bronchopulmonary changes after COVID-19. The case is suggestive from a clinical point of view, emphasizing the connection between the form, the evolution of the disease, and the consequences arising from suffering from COVID-19 infection. Fibrotic pulmonary evolutionary changes are suggestive of SARS-CoV-2 virus infection.
Authors’ contribution
CC conceived and designed the study. RS performed the analysis and drafted the manuscript. SȘ designed the significant revision of manuscript and provided significant intellectual input. All authors revised and approved the final version of the manuscript.
Patient consent
Obtained.
Competing interests
None declared.
Ethics approval
This study was approved by the Research Ethics Committee of Nicolae Testemițanu State University of Medicine and Pharmacy (Minutes no. 1 from 14.04.2023).
Authors’ ORCID IDs
Corina Conica – https://orcid.org/0000-0002-8002-2829
Rodica Selevestru – https://orcid.org/0000-0002-8923-3075
Svetlana Șciuca – https://orcid.org/0000-0003-1091-9419
References
Centers for Disease Control and Prevention. COVID-19 weekly cases and deaths per 100,000 population by age, race/ethnicity, and sex [Internet]. Atlanta: CDC; 2022-. [cited 2023 Aug 20]. Available from: https://covid.cdc.gov/covid-data-tracker/#demographicsovertime
Deville JG, Song E, Ouellette CP. COVID-19: Clinical manifestations and diagnosis in children. [Internet]. UpToDate; ©2023- [cited 2023 Jul 2]. Available from: https://www.uptodate.com/contents/covid-19-clinical-manifestations-and-diagnosis-in-children
Selevestru R, Conica C, Rotaru-Cojocari D, Bozadji V, Farmache N, Şciuca S. Lung damage in hospitalized children with COVID-19. Mold J Health Sci. 2022;(3 Suppl):396.
Bottino I, Patria MF, Milani GP, et al. Can asymptomatic or non-severe SARS-CoV-2 infection cause medium-term pulmonary sequelae in children? Front Pediatr. 2021 May 13;9:621019. doi: 10.3389/fped.2021.621019.
Osmanov IM, Spiridonova E, Bobkova P, et al; Sechenov StopCOVID Research Team. Risk factors for the post-COVID-19 condition in previously hospitalized children using the ISARIC Global follow-up protocol: a prospective cohort study. Eur Respir J. 2022;59(2):2101341. doi: 10.1183/13993003.01341-2021.
Zhang C, Huang L, Tang X, Zhang Y,Zhou X. Pulmonary sequelae of pediatric patients after discharge for COVID‐19: an observational study. Pediatr Pulmonol. 2021;56(5):1266-1269. doi: 10.1002/ppul.25239.
Lago VC, Prudente RA, Luzia DA, Franco ET, et al. Persistent interstitial lung abnormalities in post-COVID-19 patients: a case series. J Venom Anim Toxins Incl Trop Dis. 2021 Apr 14;27:e20200157. doi: 10.1590/1678-9199-JVATITD-2020-0157.
Șciuca S, Selevestru R, Conica C, Băluțel T, Rotaru-Cojocari D. Particularities of respiratory manifestations of COVID-19 infection of children. One Health Risk Manag. 2022;3(3):33-38. https://doi.org/10.38045/ohrm.2022.3.05.
Shi Q, Wang Z, Liu J, et al. COVID-19 evidence and recommendations working group. Risk factors for poor prognosis in children and adolescents with COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2021 Nov;41:101155. doi: 10.1016/j.eclinm.2021.101155.
Ademola S, Simon A, Oyeronke T, et al. Pulmonary fibrosis in COVID-19 survivors: predictive factors and risk reduction strategies. Pulm Med. 2020;5:1-10. doi: 10.1155/2020/6175964.