Introduction
Chronic pancreatitis (CP) is a widespread disease that affects patients of working age, which makes this problem not only medical, but also medical and social [1, 2]. This pathology attracts the attention of many researchers, but today there are still many unresolved issues of the pathogenesis, diagnosis and treatment of CP [3, 4].
Until now, there is no specific treatment for CP, and the goal of conservative influence is the treatment of exacerbation of the disease, chronic pain syndrome, exocrine / endocrine insufficiency of the pancreas, correction of metabolic disorders and complications [2].
For effective treatment of chronic pancreatitis, it is necessary to influence the main pathogenesis in order to inhibit the development of fibrous and other structural changes in the pancreas.
Purpose of the study: To determine the main pathogenetic links of clinical and morphological forms of CP, markers of disease progression, to develop a diagnostic algorithm and principles of treatment of patients.
Materials and methods
Prospectively, we recruited 210 patients with CP who underwent a comprehensive examination Control groups without pancreatic diseases (n = 120) and a comparison group (n = 25) were established to determine the effectiveness of the proposed treatment. Patients in all groups were comparable in terms of gender and age. To determine the effectiveness of treatment, the main indicators were studied immediately after treatment and at 6-12 months. Among the examined patients, there were 169 men and 41 women, with patients ages ranging from 26 to 72 years, and an average age of (47.3±0.7) years. The ratio of women to men was 1:4.1. According to the 1998 Marseille-Rome classification, patients were divided into 4 groups: group I consisted of 26 patients (12.4%) with obstructive CP, group II - 56 patients (26.7%) with calcification, group III - 78 patients (34.1%) with the fibro-parenchymal form, and group IV - 50 patients (23.8%) with CP complicated by pseudocyst.
Methods of research included clinical, instrumental (esophagogastroduodenoscopy (EGD), endoscopic retrograde cholangiopancreatography (ERCP), radiography, enhanced computed tomography (CT), ultrasound), and functional methods (gastric sounding to study its secretory activity and duodenal sounding with the determination of enzymes and bicarbonates) [2]. To study the role of immune factors and oxidative stress in the progression of fibrosis and stone formation in the pancreas, the following methods were used: biochemical analysis of blood serum and the contents of the pancreatic duct to determine enzymatic activity of the pancreas (amylase, lipase, phospholipase A) [4]. Levels of glycated hemoglobin (HbA1c) and hyaluronic acid (HA) were determined [4], as well as indicators of lipid peroxidation (LP) and antioxidant protection (AP) [5, 6], hexosamines (Ha) content [4], protein-bound hydroxyproline (PBH) [7], and the content of medium-weight molecules (AWM) [8].
Levels of interleukins TNF-α, TGF-β1, REG-1α, lactoferrin, and fecal elastase-1 were determined in the blood by enzyme immunoassay. The immune status and nonspecific resistance of the organism were assessed [9, 10]. Morphological methods were used to study biopsies of the pancreas obtained from 60 patients (aspiration biopsy under ultrasound control and during planned operations on the pancreas). Staining was conducted with hematoxylin and eosin and according to Mallory-Slinchenko, and pancreatic histostructure was assessed according to Stolte (1987). Immunohistochemical typing of apoptotic nucleases and morphometry were performed [11, 12]. Microbiological methods were used to determine the microbial contamination of the stomach and pancreatic duct [13].
To study the main morphological and biological changes in the pancreas during the development of CP, we conducted experimental studies on 24 laboratory white Wistar male rats weighing 180–230 g. We used our experimental model of CP, which developed as a result of blocking NO synthase [14]. Rats (n = 12) were intraperitoneally administered NG-nitro-L-arginine (L-NNA), Sigma-Aldrich (USA), at a dose of 40 mg/kg for 6 (n = 6) and 12 (n = 6) days. The control group (n = 12) consisted of rats intraperitoneally administered with 0.9% NaCl solution. Rats were removed from the experiment on days 6 and 12.
To study the effect of the drug „Glutargin” („Health”, Kyiv, Ukraine) on the state of the LP-AP system and collagen metabolism, an experimental study was conducted on 21 laboratory white Wistar male rats weighing 180-230 g. Group I rats (n = 7) were injected with L-NNA at a dose of 40 mg/kg for 12 days, and the rats in group II (n = 7) were injected with L-NNA at the same dose and glutargin at 20 mg/kg (intraperitoneally, 20 min. before the introduction of L-NNA) for 12 days. The control group (n = 7) consisted of rats that received 0.9% NaCl solution intraperitoneally. Rats were removed from the experiment on the 45th day.
The withdrawal of animals from the experiment was carried out by introducing a lethal dose of ketamine hydrochloride. After the animals were withdrawn from the experiment, blood was taken to determine the concentration of PBH, malonic dialdehyde (MDA), glucose, nitrites/nitrates, and the activity of α-amylase, lipase, and trypsin in the blood serum. A histological study of the tissue of the pancreas of rats was also conducted.
The studies were carried out in compliance with the main provisions of the Declaration of Helsinki of the World Medical Association (1964-2013) and the European Convention for the Protection of Vertebrate Animals used for Research and other Scientific Purposes [15].
Descriptive and inductive statistics were used to analyze the obtained results. In the case of quantitative data and under the condition of their normal distribution, the mean and standard error of the mean were used. To determine the significance of differences, Student's t-test was used. In the absence of a normal distribution, the median, minimum, maximum, upper, and lower quartiles were used, and the significance of differences was determined by the Mann-Whitney U test. To describe qualitative data, the frequency of feature detection (%) was used. In this case, the χ-test was used to determine the significance of differences between groups. Differences were considered significant at p < 0.05. Correlation and factor analysis were performed. All calculations were carried out in SPSS 9.0 for Windows (or Statistica 6) [16, 17]. The work was performed at the Institute of Gastroenterology of the National Academy of Medical Sciences of Ukraine.
The study has been approved on September 10, 2008, by the „Research ethics committee of Institute of Gastroenterology of National Academy of Medical Sciences of Ukraine” (minutes No. 5). Informed consent was obtained from each subject at the beginning of the study.
Results
In the experiment involving the use of L-NNA in the pancreatic tissue of rats, morphological changes characteristic of inflammation with atrophy and fibrosis of the pancreatic parenchyma were observed, along with an activation of the exocrine function of the gland. The introduction of glutargin contributed to a decrease in the level of lipid peroxidation products, an improvement in the state of the antioxidant defense system, and the normalization of collagen metabolism (PBH).
In all patients, risk factors for the development of clinical and morphological forms of chronic pancreatitis and quality of life (QOL) were studied. An assessment of the possibilities of methods for diagnosing clinical and morphological forms of CP was carried out, and morphological features of the pancreas were determined. The role of immune factors and oxidative stress in the progression of clinical and morphological forms of CP was examined, and the diagnostic capabilities of markers of inflammation, fibrosis, stone formation, and apoptosis in clinical and morphological forms of CP were studied. A treatment and diagnostic algorithm for CP has been developed, taking into account the factors of disease progression.
As a result of the work, it was found that the activity of fibrotic processes (TGF-β1) is higher in patients with a long history of the disease (groups II and III, (29.06±0.55) ng/ml and (27.62±0.56) ng/ml, respectively, compared with I (23.50±0.64) ng/ml and IV (21.16±0.67) ng/ml, (p<0.001), against the background of a decrease in the level of apoptosis receptor protein – CD95 (II (15.08±0.83)% and III (15.78±0.43)% compared with control (17.24±0.57)%, (p<0.001). The level of pro-inflammatory cytokines (TNF-ά) is increased in all patients, but significantly higher in patients with impaired pancreatic secretion outflow - group I (197.33±2.21) pg/ml, and the presence of pancreatic pseudocyst - group IV (194.44±2.62) pg/ml compared with II (174.34±12.16) pg/ml, (p<0.001) and III (178.78±1.88) pg/ml, (p<0.05), and compared with the control (22.0±0.81) pg/ml, (p<0.001).
For a detailed characterization of immune disorders, the coefficient of diagnostic value was taken into account, allowing, given the average values of the parameters in the group and their dispersions, to select indicators that are significantly different from the norm. Consequently, a formula for immune system disorders (FID) was obtained, which includes the 3 most informative indicators (Table 1). According to FID, the most pronounced changes were found in patients of group III in both cellular and humoral immunity. In patients with chronic pancreatitis complicated by a pseudocyst, dysfunction of cellular immunity is characteristic, while in patients with calcifying chronic pancreatitis – humoral dysfunction is notable.
Table 1. Formula for immune system disorders in examined patients. | ||
Groups of patients | FID | |
cellular immunity | humoral immunity | |
І group | CD3 2- , СD4 2- СD8 1+ | CIC 2+, IgG2+, IgА1+ |
ІІ group | СD4 2- , CD3 2- , СD8 1+ | CIC 2+, IgG3+, IgА2+ |
ІІІ group | СD4 2- , CD3 2- , СD4/СD8 2- | CD19 3+, CIC3+, IgG2+ |
ІV group | СD4 2- , CD3 2- , СD4/СD8 2- | CD19 3+, CIC2+, IgG1+ |
Note: the results were analyzed using Oneway ANOVA; FID – formula for immune system disorders; CD – cluster of differentiation (CD3 – T lymphocytes, CD4 – T helper cells, CD8 – cytotoxic T cells, CD19 – B lymphocytes); CIC – circulating immune complexes; Ig – immunoglobulin; (+) – hyperfunction; (-) – immune deficiency; 1 (2, 3) – the degree of immune disorders. | ||
In patients with various clinical and morphological forms of CP, unidirectional changes in the level of stone formation markers were established. There was a significant increase in the level of lithostatin (REG-1α) by 8.7 times, reaching (1498.71±63.80) pg/ml compared to the control group’s (185.0±23.0) pg/ml (p<0.001). Additionally, the level of lactoferrin increased by 18.7 times, reaching (12227.57±542.29) ng/ml compared to the control group’s (653.57±11.89) ng/ml (p<0.001).
An intergroup analysis showed that in patients of groups I and II, the level of lithostatin ((1183.22±70.69) pg/ml and (983.86±8.83) pg/ml, respectively) was significantly lower compared to patients in groups III and IV ((1779.91±109.86) pg/ml and (2256.94±57.79) pg/ml, respectively) (p<0.001). The increase in the level of lactoferrin was significantly higher in patients of groups I and II ((17669.44±841.39) ng/ml and (17461.892±261.18) ng/ml, respectively) compared with patients in groups III and IV ((7305.72±40.74) ng/ml and (7218.88±51.45) ng/ml, respectively) (p<0.001). Thus, the level of a specific protein of „pancreatic stones” - pancreatic stone protein (PSP, or lithostatin), which suppresses the growth of calcium carbonate crystals, is significantly lower in patients of groups I and II (obstructive and calcifying CP). In contrast, the level of lactoferrin, which is the basis of „pancreatic stones”, is significantly higher in patients of these groups compared with patients of groups III and IV. The coefficients of the values of these indicators relative to the control and their ratio were calculated (the control values of the studied indicators were taken as 1.0) and it was found that the probability of stone formation is high - at a value of 0.5-1.0 of the calcification coefficient (REG-1α / lactoferrin), low - at 1.5 and above.
The possibilities of modern methods for diagnosing clinical and morphological forms of CP were determined, and the highest sensitivity in diagnosing structural changes in the pancreas was found with the CT method (group I - 98.6%, II - 95.1%, III - 89.1%, IV - 98.2%). Complete agreement among CT, ultrasound, and ERCP diagnoses occurred in 64.7% of cases, partial mismatch - in 28.5%, and complete discrepancy - in 6.8%. Ultrasound demonstrated the highest sensitivity and specificity in cases of calcific CP (93.8% and 85.6%) and CP complicated by pseudocyst (92.3% and 88.5%). For diagnosing other forms of CP, it is necessary to additionally use CT and, if necessary, ERCP. In the assessment of fibrotic changes in the pancreas in CP, a significant correspondence was found between the ultrasound parameters and the data from morphological studies of the pancreas, including the areas of fibrosis in the parenchyma of the gland (r = 0.91; p = 0.03) and the density of the parenchyma (r = 0.94; p = 0.05).
As a result of the study of the histostructure of the pancreas, it was found that the morphological picture of fibrotic changes in the pancreas does not depend on the form of the disease and is characterized by a mild (I) degree of fibrosis in 6.6% of patients, moderate (II) in 20.0%, severe (III) in 16.7%, and complete fibrosis (IV) in 56.7%. Immunohistochemical studies have revealed various mechanisms of apoptosis in the exocrine and endocrine parts of the pancreas. The proapoptotic protease DNase I is expressed in the cytoplasm of acinar cells, and endonuclease-G is expressed in some of the islet cells and in the epithelium of the ducts. It has been established that an early marker of apoptosis is the translocation of DNase I from the cytoplasm to the nucleus of the acinar cell.
The vast majority of patients with CP are characterized by endotoxemia (AWM level is increased in 67.8% to (706.67±26.84) mg/l compared with the control (445.60±18.20) mg/l, p<0.001), activation of fibrotic processes (PBH increased in 81.6% to (175.76±3.59) µmol/l compared with the control (136.04±4.3) µmol/l, p<0.001), HA level increased in 75.0% to (1.71±0.24) g/l compared with the control (0.76±0.12) g/l, p<0.02), and the level of Ha was increased in 50,9% to (6.81±0.16) mmol/l compared with the control (5.04±0.19) mmol/l (p<0.001)), and no significant intergroup differences in these indicators were found.
Activation of lipid peroxidation processes was detected in 90.0% of cases (MDA up to (3.32±0.09) nmol/ml versus (2.07±0.13) nmol/ml in control, p<0.05), isolated double bonds (IDB) up to (1.42±0.04) relative units/ml versus (0.99±0.04) relative units/ml in control, p<0,05), diene conjugates (DC) up to (0.87±0.03) relative units/ml versus (0.67±0.03) relative units/ml in control, (p<0.05). Moreover, in 97.4% of patients with CP, there was an imbalance between the accumulation of primary lipid peroxidation products and a significantly accelerated decay of the products of their transformation into dialdehyde products (MDA). That is, in patients with CP, there is an intensification of lipid peroxidation processes, which contributes to the formation of secondary LP products that inactivate cationic pumps, channels, and ionic conductivities, membrane proteins, and enzymes.
On the basis of the data obtained, markers of CP progression were determined, including: the value of the calcification coefficient (REG 1α/lactoferrin) between 0.5-1.0, translocation of DNase I from the cytoplasm to the nucleus of the acinar cell, activation of collagen formation (with a decrease below 0.5), an increase in the level of fibrosis activators (TGF-β1, TNF-a), and intensification of LP processes (MDA).
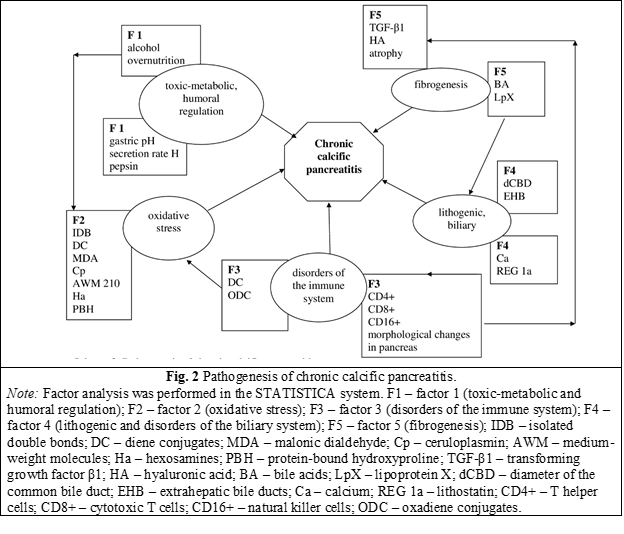
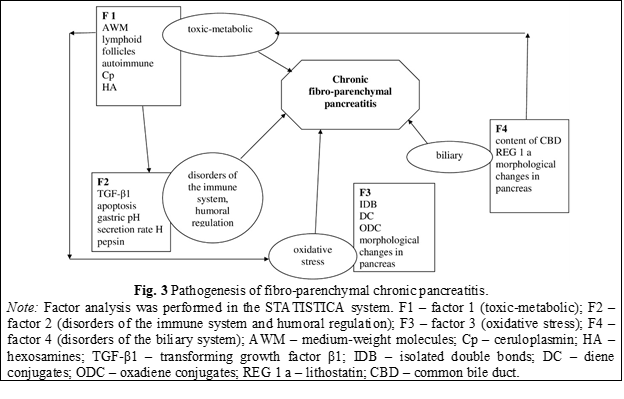
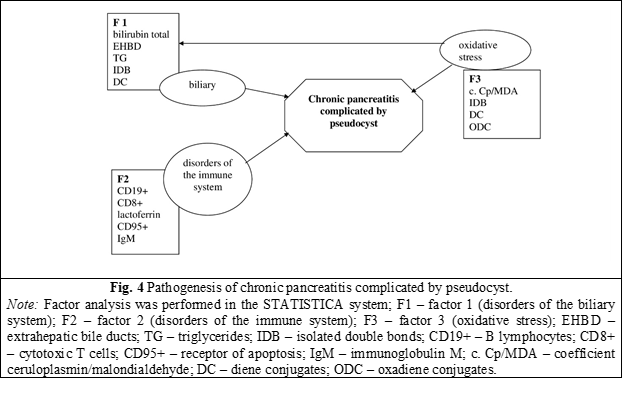
As a result of factorial and correlation analysis of the obtained data, and in order to develop a diagnostic algorithm, the main pathogenetic links of various forms of CP were formulated (Figs. 1-4). The analysis allowed us to explore the relationships between variables and interpret the „nature” of the factors that make the main contribution to explaining the variability of the sample variables.
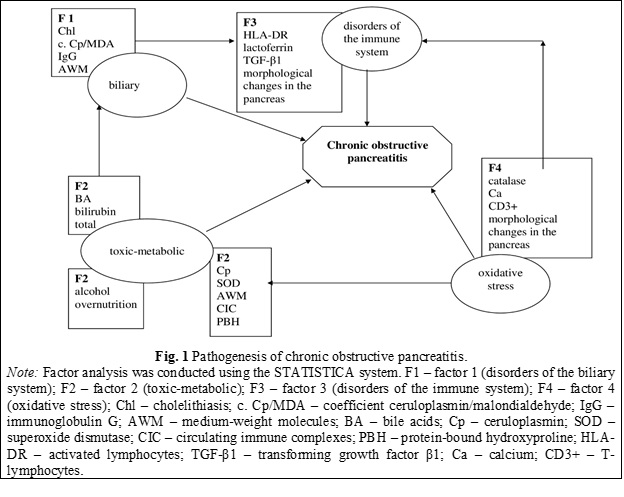
In patients of group I (obstructive pancreatitis), four factors explain about 59% of the total variance (Fig. 1). The first factor (13.4% of sample variability) correlated mainly with indicators that reflect disorders of the biliary system (presence of cholelithiasis (Chl) r = 0.72; p = 0.001), LP-AP processes (ceruloplasmin/malondialdehyde (Cp/MDA) r = 0.72; p = 0.05), endogenous intoxication (AWM r = 0.66; p = 0.05) and activation of humoral immunity (IgG r = 0, 78; p = 0.001). Therefore, with cholelithiasis (Chl), bile reflux into the pancreatic duct is determined, which, along with an imbalance in the LP-AP system, leads to inflammation and damage to the pancreatic tissue. The volume of duodeno-pancreatic reflux affects the degree of oxidative damage. Prolonged exposure to refluxate leads to fibrosis of the pancreas. There is „a vicious circle”, that is, the mutual influence of immune factors, LP indicators, disorders of the biliary tract, endogenous intoxication in the development and course of CP.
The second most important factor (16.0% of sample variability) is toxic-metabolic, correlated with indicators that reflect the toxic effect of overnutrition (r = 0.69; p = 0.001), harmful substances and toxins (alcohol r = 0.82; p = 0.05, CIC r = 0.77; p = 0.05, AWM r = 0.73; p = 0.05, bile acids (BA) r = 0.78; p = 0.01, bilirubin r = 0.76; p = 0.001), and shows their direct effect on acinar cells, cell metabolism, which leads to fatty degeneration, cell necrosis and the development of fibrosis (PBH r = 0.81; p = 0.05). Periductal fibrosis develops and, accordingly, dilatation of the ducts. Fibrosis of the pancreatic tissue with scarring in the periductal areas leads to obstruction of the ducts. Complete and prolonged obstruction leads to atrophy and fibrosis. Structural changes in the pancreas, which were detected by ERCP, CT, or ultrasound, correlate with the level of endogenous intoxication (AWM r = 0.78; p = 0.01), metabolic changes (LpX r = 0.76; p = 0.03, Ca r = 0.73; p = 0.028), and AP disorders (superoxide dismutase (SOD) r = 0.77; p = 0.04).
The third factor (15.0% sample variability) reflects disorders of the immune system; it is correlated with the level of activated lymphocytes (HLA-DR r = 0.68; p = 0.001), lactoferrin (r = 0.86; p = 0.05), profibrotic cytokines (TGF-β1 r = 0.81; p = 0.001), which, in turn, leads to the activation of stellate cells with their subsequent production of an extracellular matrix with a predominance of collagen. This leads to the replacement of the functional parenchyma of the gland with fibrous tissue (fibrosis index r = 0.79; p = 0.03).
The fourth factor (14.3% of sample variability) reflects oxidative stress and correlates with the level of catalase (r = 0.70; p = 0.05), lipid peroxidation products (MDA r = 0.79; p = 0.003), (Ca r = 0.73; p = 0.028), the level of lymphocytes (CD3 r = 0.88; p = 0.001). Various xenobiotics during their metabolism cause oxidative stress in the pancreatic tissue, which leads to cell and organ damage (fibrosis index r = 0.56; p = 0.007).
In the development of clinical and morphological forms of CP, the same factors are important: toxic-metabolic, biliary, immune, oxidative stress, but there are differences. In patients of group II (calcifying pancreatitis), the largest number of factors was found - 5 (Fig. 2), which confirms the data obtained on the basis of a comprehensive clinical, laboratory, and instrumental study that the calcific form of CP is the most unfavorable for the course and prognosis. Five factors explain about 58.4% of the total variance.
The first toxic-metabolic factor (11.1% of sample variability) was additionally correlated with indicators of humoral mechanisms of regulation of pancreas activity (pH r = 0.81; p = 0.001; H+ secretion rate r = 0.73; p = 0.05; pepsin r = 0.87; p = 0.001). In combination with the second factor (oxidative stress, 12.0% of sample variability, correlated with Cp indicators r = 0.79; p = 0.05, Ha r = 0.75; p = 0.001, IDB r = 0.68; p = 0.05, DC r = 0.69; p = 0.003), third (disorders of the immune system, 13.6% sample variability, correlated with CD19 r = 0.74; p = 0.001, CD4 r = 0.74; p = 0.001, CD16 r = 0.65; p = 0.001), and disorders of the biliary system (fourth factor, 8.9% of the sample variability, correlated with the expansion of the choledochus r = 0.68; p = 0.001, choledochal calculi r = 0.63; p = 0.05); these changes lead to the activation of stone formation (REG-1α r = 0.78; p = 0.05; Ca r = 0.83; p = 0.001). Against the background of an increase in the phenomena of cholestasis and metabolic disorders, the processes of fibrosis of the pancreas intensify (fifth factor, 9.1% of sample variability, correlated with BA values r = 0.80; p = 0.001, LpX r = 0.85; p = 0 .01, TGF-β1 r = 0.75, p = 0.01, HA r = 0.71, p = 0.001).
In patients of group III (fibro-parenchymal form of CP), similarly to the first group, 4 factors were identified that explain 50.8% of the variance (Fig. 3): the toxic-metabolic factor is determined in the first place (14.5% of the sample variability, correlated with AWM r = 0.77, p = 0.05, Cp r = 0.70, p = 0.05, HA r = 0.62, p = 0.05, lymphoid follicles r = 0.67, p = 0.01), on the second - disorders of the immune system and humoral regulation of the activity of the pancreas (13.9% of sample variability, correlated with TGF-β1 r = 0.65; p = 0.001, apoptosis r = 0.83; p = 0.05, gastric pH r = 0.88, p = 0.05, H+ secretion rate r = 0.78, p = 0.01, pepsin r = 0.88, p = 0.05) induced by oxidative stress (the third factor is 11.9% of the sample variability, correlated with IDB indicators r = 0.65, p = 0.05, DC r = 0.86, p = 0.05, oxadiene conjugates (ODC) r = 0.65, p = 0.05). All these changes, along with disorders of the biliary system (fourth factor - 10.5% of the sample variability, correlated with indicators of the content of the choledochus r = 0.83; p = 0.05, REG-1 α r = 0.67; p = 0.05, fibrosis index r = 0.74; p = 0.05), lead to damage to the pancreas. The high probability of stone formation is evidenced by REG-1α, which is a component of the fourth factor.
The smallest number of factors was found in patients of group IV - 3 factors (Fig. 4): biliary (13.3% of sample variability, correlated with bilirubin index r = 0.75; p = 0.05, dilatation of extrahepatic bile ducts r = 0.77; p = 0.05, triglycerides (TG) r = 0.76; p = 0.05, IDB r = 0.82; p = 0.05), disorders of the immune system (13.2% sample variability, correlated with CD19 r = 0.74, p = 0.05, CD8 r = 0.76, p = 0.05, lactoferrin r = 0.70, p = 0.05, CD95 r = 0.65, p = 0.05, IgM r = 0.66; p = 0.05), oxidative stress (10.7% of sample variability, correlated with Cp/MDA r = 0.63; p = 0.05, IDB r = 0.83; p = 0.001, DC r = 0.95, p = 0.001, ODC r = 0.81, p = 0.05). These three factors account for 37.1% of the variance. This coincides with the data on a short history of the disease in patients of this group and the development of pseudocysts after acute pancreatitis.
Based on the conducted studies and factor analysis data, the diagnostic algorithm for patients with CP was improved (Fig. 5).
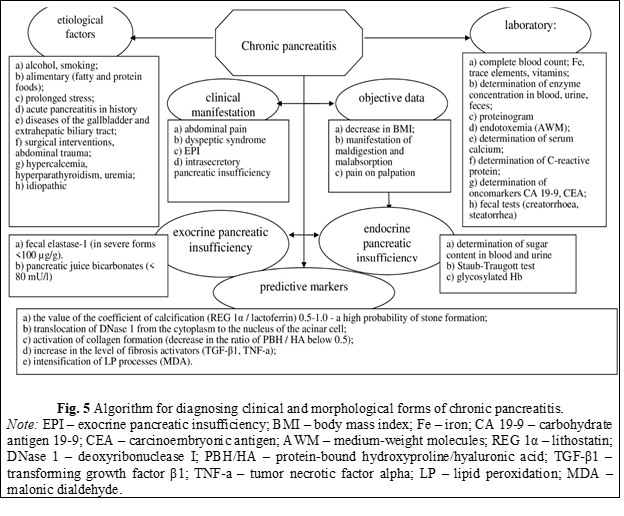
The developed diagnostic algorithm, with the maximum information content of the data obtained, made it possible to evaluate the pathophysiological features of functional and organic disorders of the pancreas in patients with CP, choose a pathogenetically justified method of treatment, and reduce the length of stay in the hospital.
A group of patients with persistent and intermittent pain syndrome due to obstruction at various levels of the pancreatic ductal system was identified, with the development of complications that could not be eliminated by conservative methods and were subject to surgical treatment. With obstructive CP, the treatment of patients is aimed at eliminating the cause of the obstruction, which is achieved only by surgical methods. Patients with CP complicated by pseudocyst formation also need treatment in the surgical department. They underwent gastro/duodenocystostomy or percutaneous puncture of the pseudocyst at the first stage of treatment, and then surgery was performed. Surgical treatment of patients with CP was aimed at improving the outflow of pancreatic juice from the main pancreatic duct or resection of the affected area of the gland.
The tactics of conservative treatment for patients with CP was the use of basic complex therapy to relieve exacerbation of the disease, chronic pain syndrome, exocrine/endocrine insufficiency of the pancreas, and correction of metabolic disorders and complications. Analgesics, non-steroidal anti-inflammatory drugs, enzyme preparations, antacids, and proton pump blockers were used.
In addition to the basic therapy, treatment is proposed aimed at stopping the pain syndrome, normalizing immune system disorders, eliminating oxidative stress, and inhibiting fibrotic processes. To stop the pain syndrome, a vortex pulsed magnetic field (VPMF) was applied with an effect on the projection of the pancreas and biologically active points for 5-15 minutes in a course of 10-15 sessions [18]. Glutargin (a salt of arginine and glutamic acid) was used to normalize the state of the LP-AP system, glutathione, and ultimately as an antifibrotic agent [19]. For immunocorrection and increasing the adaptive potential of the body, reducing the level of pro-inflammatory cytokines and profibrotic cytokines, patients with CP were prescribed autocytokine therapy in addition to the main treatment [20, 21].
As a result of complex treatment, good results were obtained in 73.5% of patients. The severity of pain, as measured by the visual analogue scale (VAS), decreased. There was a significant decrease in the levels of lactoferrin, REG 1α, TGF-1β, and normalization of the Tx/Tc ratios. There was also a significant decrease in the marker of collagen formation (PBH) and lipid peroxidation products (MDA).
Discussion
The development of CP is considered the result of exposure to various pathological stimuli. There is no single etiology that inevitably leads to CP, and it is considered a complex disease with several concomitant factors [3, 22, 23]. The diagnosis of CP requires the integration of clinical, laboratory, and imaging features [24, 25].
In our study, we demonstrated that the development and course of clinical and morphological forms of CP are determined by the ratio of regulatory factors of the immune system, apoptosis, and oxidative stress. The obtained interrelations of immune factors, oxidative stress, and structural changes in the pancreas made it possible to develop markers for the progression of CP: the value of the calcification coefficient (REG 1α / lactoferrin) 0.5-1.0; translocation of DNase I from the cytoplasm to the nucleus of the acinar cell; activation of collagen formation (decrease in the ratio of PBH / HA below 0.5); the growth of the level of fibrosis activators (TGF-β1, TNF-a), intensification of LP processes (MDA). In our study, it was shown that an early marker of apoptosis is the translocation of DNase I from the cytoplasm to the nucleus of an acinar cell.
Today, the treatment of patients with CP remains one of the most difficult areas of pancreatology [25, 26]. A search is being made for treatment methods that can influence the main links in the pathogenesis of the disease to inhibit the development of fibrosis and other structural changes in the pancreas [27].
In the ACG guideline on CP (2020), it is noted that the most frequent symptom of CP and a factor in patients' low quality of life is abdominal pain, which is often refractory to the treatment used [26]. There is a constant search for treatment methods that can reduce the severity of the pain syndrome and slow down the progression of CP.
One of the mechanisms of the pain syndrome is damage to nerve endings [28, 29]. In the hope of treating refractory pain in CP, various experimental treatment methods, such as spinal cord nerve stimulation, transmagnetic brain stimulation, or direct radiation therapy to the pancreas, have been performed, and they have shown their effectiveness in treating pain [26, 30].
We used VPMF to treat pain and showed that in patients with CP and refractory pain, VPMF has an analgesic effect, improves the patient's general condition and quality of life [18].
In the development and progression of CP, an important pathogenetic chain is the uncontrollable strengthening of LP processes. In the case of prolonged action, oxidative stress entails the destruction and death of cells, which further leads to the progression of fibrous changes, exocrine and intrasecretory pancreatic insufficiency [3, 31, 32]. Therefore, antioxidants are used to correct LP [33, 34].
In our work, we used glutargin in the complex treatment of patients with CP. The composition of glutargin includes L-arginine and glutamic acid; it is able to activate the synthesis of enzymes of antioxidase protection (glutathione, glutathione peroxidase); therefore, it is an antioxidant. In addition, L-arginine enhances the activating effect of glutamic acid, which, in turn, together with metabolites, changes the activity of phosphorylase A2 and promotes the removal of toxic products of peroxidized fatty acid residues of phospholipids [19].
Cytokines play an important role in the pathogenesis of CP, as in any inflammatory process. During pancreatic injury, atrophic acinar cells activate several key participants in inflammation, such as macrophages and granulocytes, which release a number of pro-inflammatory cytokines. Proinflammatory cytokines additionally activate pancreatic stellate cells, contributing to the development of CP [35-37].
Cytokines have promising potential as therapeutic agents. However, the clinical use of cytokines is limited since they have high pleiotropy, and their systemic administration can lead to severe side effects [38].
We used autologous cytokines (autocytokines) in addition to the main treatment of patients with CP. Autocytokines act according to the network principle and their immunocorrective effect is directed to the cells involved in inflammation, regeneration, and development of the immune response [20]. The main principles of the method are the use of a composition of cytokines secreted by mononuclear cells of the patient's peripheral blood, it allows to avoid the development of toxic and allergic side effects [20].
Conclusions
The obtained results contribute to a further understanding of the complex pathogenesis of pancreatitis, improving the diagnosis and treatment of patients with CP. The use of disease progression markers has enhanced the diagnosis of clinical and morphological forms of pancreatitis and the stratification of treatment. The proposed treatment for patients with chronic pancreatitis contributed to a decrease in the severity of pain, normalization of the cytokine profile, and limitation of oxidative stress, improving the general condition and quality of life of patients.
Competing interests
None declared.
Patient consent
Obtained.
Ethics approval
The study was approved on 10 September 2008 (minutes No. 5) by the Research ethics committee of the Institute of Gastroenterology of the National Academy of Medical Sciences of Ukraine.
Acknowledgments
The author thanks Gaidar Y.A., MD. (Laboratory of Pathomorphology, Institute of Gastroenterology, National Academy of Medical Sciences of Ukraine), Rudenko A.I., Ph.D. (Laboratory of Pathophysiology, Institute of Gastroenterology, National Academy of Medical Sciences of Ukraine), Kudryavtseva V.E., Ph.D. (Laboratory of Immunology and Microbiology, Institute of Gastroenterology, National Academy of Medical Sciences of Ukraine) for their participation in the research and assistance in obtaining data.
The materials of this article were previously published in Ukrainian [39].
Author’s ORCID ID
Olena Krylova - https://orcid.org/0000-0002-3033-4912
References
Desai N, Kaura T, Singh M, Willingham FF, Rana S, Chawla S. Epidemiology and characteristics of chronic pancreatitis - Do the East and West meet? Gastro Hep Advances. 2022;1(6);942-949. https://doi.org/10.1016/j.gastha.2022.07.013.
Shimizu K, Ito T, Irisawa A, Ohtsuka T, Ohara H, Kanno A, et al. Evidence-based clinical practice guidelines for chronic pancreatitis 2021. J Gastroenterol. 2022 Oct;57(10):709-724. doi: 10.1007/s00535-022-01911-6.
Aghdassi AA. Pathogenesis of chronic pancreatitis. In: Pancreapedia: Exocrine Pancreas Knowledge Base, 2016. doi: 10.3998/panc.2016.16.
Kamyshnikov VS. [Handbook of clinical and biochemical studies and laboratory diagnostics]. 3rd ed. Moscow: MEDpress-Inform; 2009. 896 p. Russian.
Metel'skaia VA, Gumanova NG. [Screening as a method for determining the serum level of nitric oxide metabolites]. Klin Lab Diagn. 2005;(6):15-18. Russian.
Ovsyannikova LM, Alekhina SM, Drobinskaya OV. [Biochemical and biophysical methods for assessing oxidative homeostasis disorders in persons exposed to radiation due to the Chernobyl accident: methodical recommendations]. Moscow; 1999. 18 p. Russian.
Osadchuk TK, Motin IuK, Osadchuk MA. [Study of hydroxyproline in gastric juice and its diagnostic value]. Lab Delo. 1982;(4):16-18. Russian.
Nikolaychuk VV, Moin VM, Kirkovsky VV. [A method for determining “average molecules”]. Lab Delo. 1991;(10):13-16. Russian.
Sochner AM, Belchenko IE, Burshtein AM. [Lymphocytotoxic test as a method for identifying T-lymphocyte subpopulations with monoclonal antibodies]. Lab Delo. 1989;(3):29-32. Russian.
Khaitov RM, Pinegin BV. [Evaluation of the immune status in normal and pathological conditions]. Immunologiia. 2001;(4):4-6. Russian.
Stolte M. Chronische Pankreatitis [Chronic pancreatitis]. Verh Dtsch Ges Pathol. 1987;71:175-85. German.
Wang GS, Rosenberg L, Scott TW. Tubular complex as a source for islet neogenesis on the pancreas of diabet-prone BB rats. Lab Invest. 2005;85(5):675-688. doi: 10.1038/labinvest.3700259.
Marukhno TV, editor. [Bacteriology and virology: Standard production and practical publication]. Kiev: Mediinform; 2007. Ukrainian.
Krylova OO, Rudenko AI, Gaidar IuA, inventors. Method for modeling pancreatitis in experiment. Ukraine patent № 61631 G 09B 23/00. 2011.
Rozemond H. Laboratory animal protection: the European Convention and the Dutch Act. Vet Q. 1986;8(4):346-9. doi: 10.1080/01652176.1986.9694067.
Eniukov IS. [Methods, algorithms, programs for multidimensional statistical analysis]. Moscow: Finansy i statistica; 1986. 231 p. Russian.
Petri A, Sabin K. [Medical statistics at a glance]. Moscow: GEOTAR-MED; 2003. 141 p. Russian.
Filippov IuA, Krylova OO, Rudenko AI, inventors. Method of treatment of pain syndrome in patients with chronic pancreatitis. Ukraine patent № 63463 A 61N 2/02. 2011.
Filippov IuA, Krylova OO, Yagmur VB, inventors. Method for correcting disorders of the glutathione system in patients with chronic pancreatitis. Ukraine patent № 63469 A 61K 39/06. 2011.
Filippov IuA, Krylova OO, Lukinov GV, inventors. Method for correcting the state of the immune system in patients with chronic pancreatitis. Ukraine patent № 63468 A 61K 37/02. 2011.
Kovalchuk LV, Gankovskaia LV. [Immunocytokines and local immunocorrection]. Immunologiia.1995;(3):4-7. Russian.
Whitcomb DC. Mechanisms of disease: advances in understanding the mechanisms leading to chronic pancreatitis. Nat Clin Pract Gastroenterol Hepatol. 2004;1(1):46-52. doi: 10.1038/ncpgasthep0025
Muniraj T, Aslanian HR, Farrell J, Jamidar PA. Chronic pancreatitis, a comprehensive review and update. Part I: epidemiology, etiology, risk factors, genetics, pathophysiology, and clinical features. Dis Mon. 2014;60(12):530-550. doi: 10.1016/j.disamonth.2014.11.002.
Esposito I, Hruban RH, Verbeke C, Terrise B, Zambonif G, Scarpag A, et al. Guidelines on the histopathology of chronic pancreatitis. Recommendations from the working group for the international consensus guidelines for chronic pancreatitis in collaboration with the International Association of Pancreatology, the American Pancreatic Association, the Japan Pancreas Society, and the European Pancreatic Club. Pancreatology. 2020;20(4):586-593. doi: 10.1016/j.pan.2020.04.009.
Singh VK, Yadav D, Garg PK. Diagnosis and management of chronic pancreatitis: a review. JAMA. 2019;322(24):2422-2434. doi: 10.1001/jama.2019.19411.
Gardner TB, Douglas AG, Forsmark CE, Sauer BG, Taylor JR, Whitcomb DC. ACG Clinical Guideline: Chronic Pancreatitis. Am J Gastroenterol. 2020;115(3):322-339. doi: 10.14309/ajg.0000000000000535.
Zion O, Genin O, Kawada N, Yoshizato K, Roffe S, Nagler A, et al. Inhibition of transforming growth factor-beta signaling by halofuginone as a modality for pancreas fibrosis prevention. Pancreas. 2009;38:427-435. doi: 10.1097/MPA.0b013e3181967670.
Demir IE, Tieftrunk E, Maak M. Friess H, Ceyhan GO. Pain mechanisms in chronic pancreatitis: of a master and his fire. Langenbecks Arch Surg. 2011;396(2):151-160. https://doi.org/10.1007/s00423-010-0731-1.
Fregni F, Pascual-Leone A, Freedman SD. Pain in chronic pancreatitis: a salutogenic mechanism or a maladaptive brain response? Pancreatology. 2007;7(5-6):411-22. https://doi.org/10.1159/000108958.
Fregni F, Potvin K, Dasilva D, Wangd X, Lenkinskid RE, Freedmanc SD, et al. Clinical effects and brain metabolic correlates in non-invasive cortical neuromodulation for visceral pain. Eur J Pain. 2011;15(1):53-60. doi: 10.1016/j.ejpain.2010.08.002.
Stevens T, Conwell DL, Zuccaro G. Pathogenesis of chronic pancreatitis: an evidence-based review of past theories and recent developments. Am J Gastroenterol. 2004;99(11):2256-2270. doi: 10.1111/j.1572-0241.2004.40694.x.
Sarles H, Bernard JP, Gullo I. Pathogenesis of chronic pancreatitis. Gut. 1990;31:629-632 doi: 10.1136/gut.31.6.629.
de Las Heras-Castaño G, García-Unzueta MT, Domínguez-Diez A. Fernández-González MD, García-de la Paz AM, Mayorga-Fernández M, et al. Pancreatic fibrosis in rats and its response to antioxidant treatment. JOP. 2005;6(4):316-24.
Singh N, Bhardwaj P, Pandey RM, Saraya A. Oxidative stress and antioxidant capacity in patients with chronic pancreatitis with and without diabetes mellitus. Indian J Gastroenterol. 2012;31(5):226-231. https://doi.org/10.1007/s12664-012-0236-7.
Zhang H, Neuhöfer P, Song L, Rabe B, Lesina M, Kurkowski MU, et al. IL-6 trans-signaling promotes pancreatitis-associated lung injury and lethality. J Clin Invest. 2013;123(3):1019-31. doi: 10.1172/JCI64931.
Manohar M, Verma AK, Venkateshaiah SU, Sanders NL, Mishra A. Pathogenic mechanisms of pancreatitis. World J Gastrointest Pharmacol Ther. 2017;(1):10-25. doi: 10.4292/wjgpt.v8.i1.10.
Muller-Pillasch F, Menke A, Yamaguchi H, Elsasser HP, Bachem M, Adler G, et al. TGF beta and the extracellular matrix in pancreatitis. Hepatogastroenterology. 1999;46(29):2751-6.
Pires IS, Hammond PT, Irvine DJ. Engineering strategies for immunomodulatory cytokine therapies - challenges and clinical progress. Adv Ther (Weinh). 2021;4(8):2100035. https://doi.org/10.1002/adtp.202100035.
Krylova O.O. Clinical and morphological variants of chronic pancreatitis: the main pathogenetic links, diagnostic algorithm and substantiation of the principles of treatment of patients, Herald of Pancreatic Club, 2015;4(29):51-55. Ukrainian