Introduction
Psoriatic arthritis, also called psoriatic arthropathy, is suffering interpreted by different authors as a unitary disease [1] or as an association of two diseases – skin psoriasis and arthritis [1, 16].
Psoriasis occurs in about 2% of the population of Europe and North America [6], and arthritis is revealed in 6%-39% of psoriatic patients [6, 7]. Recent European research EuroPSO [3] has shown that skin psoriasis evolves with arthritis in 30% of patients, and in the USA – in 11%.
Psoriatic arthritis produces chronic joint damage and functional joint disorders with significant medical and social costs and an increased rate of morbidity and mortality [6]. It evolves with erosive and destructive joint changes, which are found in about 40 to 60% of patients [6, 9]. However, some clinical peculiarities, especially of clinical variants in the context of their dependence on the state of immune status and genetic predisposition, are not definitively elucidated.
Studies have shown that patients with PsA also suffer from associated comorbidities, including cardiovascular disease, obesity and metabolic syndrome, diabetes, osteoporosis, malignant diseases, non-alcoholic liver disease, depression and anxiety. To ensure an optimal result, the identification of these comorbidities is extremely important.
Given that both psoriasis and myocardial infarction have been associated with metabolic syndrome, it is possible that there is an indirect link between them, although the perception of psoriasis as a cardiovascular risk factor has only recently been proposed.
Cardiovascular diseases in psoriatic arthritis
PsA is associated with an increased risk of developing cardiovascular diseases (CVD). A meta-analysis of 11 studies found an increased risk of CVD by 43% in patients with PsA compared to the general population [13]. The risks of morbidity for myocardial infarction and cerebrovascular diseases were increased by 68% and 22%, respectively. This increased risk is partly independent of traditional cardiovascular risk factors such as diabetes, dyslipidemia and smoking, supporting the idea that PsA is an independent risk factor for cardiovascular (CV) events [13, 14]. In a study in the THIN database in the UK, the risk of CV events incidents in PsA (HR 1.24, CI 95% 1.03-1.49) and psoriasis (HR 1.08, CI 95% 1.02-1.15) without antirheumatic drugs that alter the disease (DMARD) was similar to AR (HR 1.39, CI 95% 1.28-1.50) after the adjustment for age, sex, calendar year and traditional CV risk factors [3, 5]. Chronic inflammation plays a role in atherosclerosis, which is the basic mechanism of CVD [2, 6]. Data from epidemiological studies show an independent association between the severity of PsA-related inflammation and the risk of CVD. Markers of PsA disease activity, including polyarthritis, dactylitis, extensive skin psoriasis and increased inflammatory markers, have been associated with CV clinical events [7]. In addition, patients with PsA tend to have high-risk characteristics for plaque rupture, and the extent of atherosclerotic plaques has been associated with disease activity indices and inflammatory markers [7, 9]. These findings suggest that proper management of CVD in PsA should address both traditional risk factors and aim at better control of inflammation.
Impact of PsA therapies on CV risk
The effects of drugs that are used to treat psoriasis and PsA on the risk of CVD are complex. While some medications may have a beneficial effect on the risk of CVD by suppressing inflammation, others, such as NSAIDs and corticosteroids, have been associated with increased CV risk in the general population and among rheumatic patients [5]. The concept of inflammation suppression as a means of reducing the risk of CVD has been tested in non-rheumatic patients with conflicting results. Two recent studies in high-risk patients showed a reduction in the risk of CVD with inhibition of IL-1 (canakinumab) and colchicine compared to placebo [4, 5]. However, another study with MTX showed negative results [5]. In patients with rheumatic diseases such as PsA, suppression of inflammation is the main purpose of treatment; therefore, it is unethical to conduct similar studies to simply assess the effect of antirheumatic treatments against placebo. Therefore, data on the effect of antirheumatic drugs on the risk of CVD are limited to observational studies or short-term randomized trials controlled with placebo, which evaluated intermediate results by imaging or laboratory biomarkers.
There is growing evidence that treatment with anti-TNFα drugs is associated with a reduced risk of developing CVD in patients with psoriasis and PsA, with an approximately 30% reduction in CV events among patients using anti-TNFα compared to those treated with non-biological DMARD or phototherapy [5,15]. This protective effect can be mediated by reducing vascular inflammation that can eventually lead to inhibition of the progression of atherosclerotic plaque among patients with PsA treated with TNFα inhibitors [5, 15]. Only limited information is available on the effect of other biological DMARD targeting the pathogenic pathways IL-23 and IL-17 on the risk of CVD in patients with psoriasis. Despite initial concerns about the increased risk of CVD that led to early discontinuation of clinical trials with IL-12/23 inhibitor briakinumab [13], recent data supports the CV safety of this class of biological preparations. In a randomized placebo-controlled trial, ustekinumab inhibitor IL-12/23 was more effective than placebo in reducing aortic vascular inflammation in patients with severe psoriasis [15]. Another study showed that inhibition of IL-12/23 resulted in a greater improvement in coronary, arterial and myocardial function than TNFα or cyclosporine inhibition treatments in patients with psoriasis [5]. These improvements in CVD surrogate outcomes can be translated into a lower risk of developing CV events. Data from a meta-analysis of 38 randomized clinical trials based on biological treatment in patients with psoriasis showed a similar overall risk of developing CV events between anti-TNFα and ustekinumab [5, 15]. According to these findings, observational data from patient registries and drug claims databases suggest that the risk of developing CV events is similar in patients using anti-TNFα and ustekinumab [15]. There is limited information about CV risk associated with newer classes of drugs. Secukinumab, an inhibitor of IL-17, improved the coronary flux reserve and left ventricular strain compared to MTX and cyclosporine, indicating an overall beneficial effect on CV function [15]. Short-term safety data from clinical trials of IL-17 and IL-23 inhibitors in patients with psoriasis and PsA show no evidence of increased CV risk, but long-term real-world data is still lacking. [13 ] Finally, there have been recent concerns about the venous thromboembolic risk associated with Janus Kinase inhibitors (JAK) in patients with rheumatoid arthritis (RA); [11] short-term safety data from clinical trials in patients with PsA does not suggest an increased risk of major CV events or thromboembolic events with this class of drugs [15]. However, real-world long-term observational data is needed to accurately quantify cv risk in PsA. In general, these data support the safety and potential cardioprotective effect of TNFα and IL-12/23 inhibitors in patients with psoriasis. Information about newer classes of biological preparations is awaiting further research.
Purpose of the study
To evaluate the relationship of cardiovascular comorbid pathology with the clinical and laboratory characteristics of the evolution of psoriatic arthritis and quality of life to optimize patient management tactics.
Material and methods
In order to achieve the purpose and objectives of the study, a group of 92 patients with psoriatic arthritis was selected, established in accordance with the CASPAR diagnostic criteria (2006). The patients were treated in the rheumatology and arthrology departments of the Republican Clinical Hospital „Timofei Moşneaga” and of the Municipal Clinical Hospital „Saint Trinity” in Chisinau during 2017-2019. In order to achieve the purpose and objectives of the research, type 1 cohort study (prospective study with retrospective components) was planned.
For each patient were recorded the demographic data, the determination of the anthropometric data (height, weight and body mass index or Quetelet index), the parameters of the central hemodynamics – SBP, TAD, the smoking status, the personal and heredo-collateral history of cardiovascular disease. Each patient was examined according to a questionnaire, which included questions about the way of life, the presence of risk factors, the diet, the duration of the disease and the subjective state of the patient. The measurement of blood pressure values was carried out according to the standard method. With the help of the sphygmomanometer, the systolic blood pressure (SBP) and the diastolic blood pressure (DBP) were assessed in accordance with the first and fifth phases of the Korotkoff tones, after a rest period of 5-10 minutes in a horizontal or sitting position, the measurements made at least 2 times in both arms.
The average age of patients with PsA was 42.9±9.6 years, the average duration of psoriasis was 11 (7; 25.8) years, the average duration of PsA was 7 (2; 11.8) years. Among the patients included in the study were 42 (45.7%) men and 50 (54.3%) women. Patient characteristics are shown in Table 1.
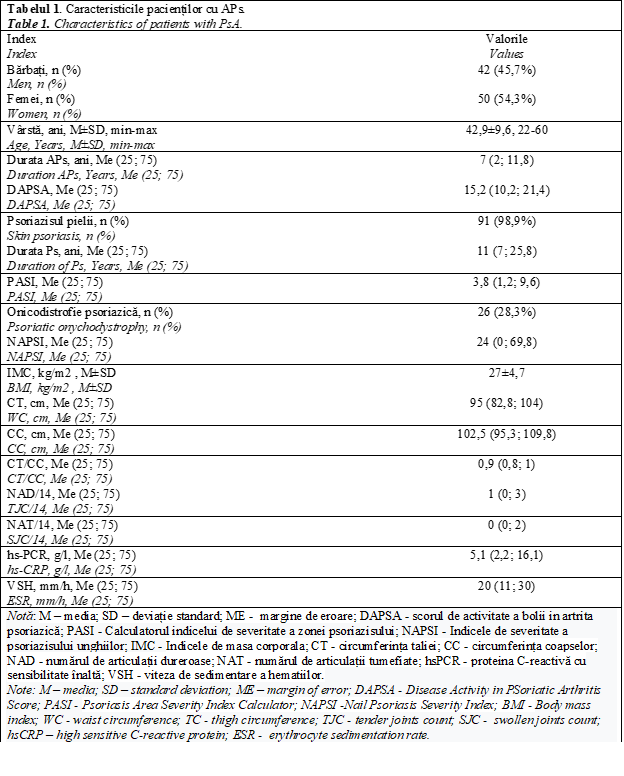
A positive family history of psoriasis was detected in 31 (33.7%) patients. At the time of inclusion in the study, 19 (20.6%) patients had disabilities, of which 15 (16.3%) had disabilities due to PsA, and 4 (4.3%) of patients had a general disease.
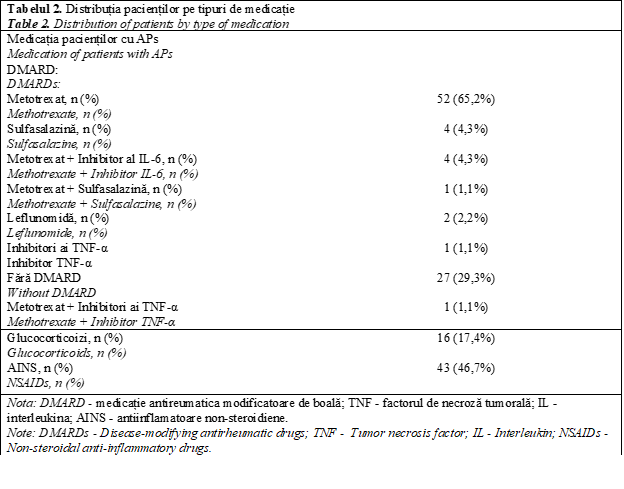
Treatment of patients with PsA was carried out in accordance with the recommendations of the National Clinical Protocol „Psoriatic arthritis in the adult” at the time of the study. The distribution of patients according to the medication is shown in Table 2.
Distribution of patients by activity of PsA when calculating the DPSAA index (Disease Activity in PSoriatic Arthritis): most had moderate activity (14-28) of 33 (42%), high (>28) in 13 (16%) patients, decreased (4-14) – 30 (38%), remission (<4) was observed in 3 (4%) patients.
The distribution of patients according to the activity of cutaneous psoriasis in the calculation of the PASI index was as follows: remission - 7 (8%), mild - 57 (68%), average - 9 (11%) severe - per 11 (13%) patients.
According to the clinical and instrumental methods of the study, the distribution of patients through the involvement of peripheral joints and spine was as follows: polyarthritis was in 63 (68,5%) patients, oligoarthritis - in 19 (20,7%), monoarthritis - 10 (10,9%), axial manifestations including sacroiliitis - in 30 (32,6%) patients with spondylitis - in 23 patients (25%), a combination of sacroiliitis and spondylitis - in 13 patients (14,1%). Patients with isolated axial lesions were absent.
Results
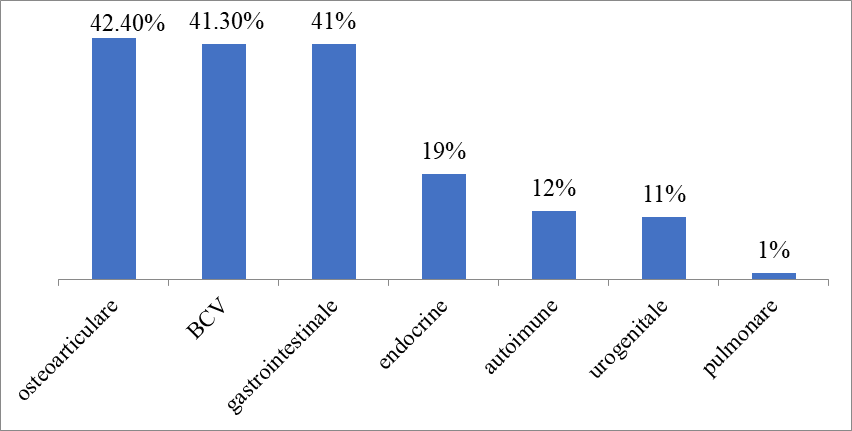
Among patients with PsA, comorbid pathology (CP) was observed in 71 (77.2%) patients. More than one CP was observed in 60.9% (56 out of 92) of patients. The frequency of smoking patients was 31.5% (29 out of 92) of patients. There was no difference in the number of CP between men and women (p>0,05). When comparing the number of CPs in the groups of patients with isolated peripheral arthritis (n = 52) and the combination of peripheral arthritis with axial lesions (sacroiliitis and spondylitis) (n = 40), no statistically significant differences were found (p>0,05) (depending on the sex and age of the group were comparable, p>0,05). CP structure was analyzed in patients with young and middle age PsA (Figure 1).
|
Fig. 1 Structura patologiei comorbide la pacienții cu APs. Fig. 1 The structure of comorbid pathology in patients with APs. |
It was found that other diseases of the musculoskeletal system and connective tissue not associated with psoriasis were observed in 42.4% (39 out of 92) of patients, among which gout was observed in 3.3% (3 out of 92) of patients, OA - in 39.1% (36 out of 92) of patients.
On the second place, with the highest frequency was placed the cardiovascular
In the study conducted by us in the 92 patients with PsA, different subjective and objective symptoms of heart damage were determined. This number does not include persons aged up to 18 and after 60 years, with obesity (BMI>25 kg/m2), diabetes mellitus type I or II, hypertension and ischemic heart disease developed up to the onset of the underlying disease, congenital dyslipidemia, congenital and rheumatic cardiopathy, decompensated cirrhosis of the liver, long-term treatment with glucocorticoids (>1 month) or > 1 mg/kg/body (for 2 weeks).
In the general study group, regarding the psoriatic arthritis, the patients' complaints were limited only to pain or discomfort sensations in the precarious region (12 patients), sensations of collPsAe (11 patients), bouts of heart palpitations (7 patients), dyspnea manifested at moderate and minimal physical exertion (in 11 cases) and peripheral edema of cardiac genesis in 4 patients.
|
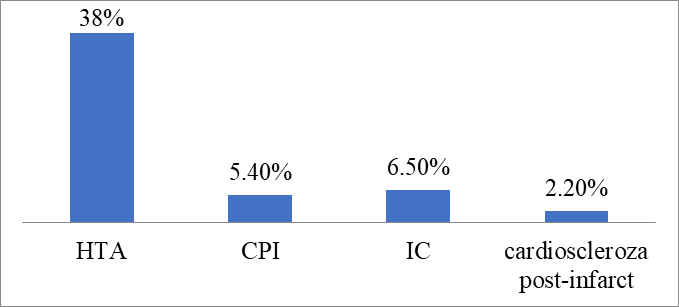
Fig. 2 Structura bolilor cardiovasculare la pacienții cu APs Fig. 2 The structure of cardiovascular disease in patients with PsA |
The most common pathology was hypertension with a frequency of 38% (35 out of 92). With an established diagnosis of coronary heart disease: exertion angina pectoris - at 5.4% (5 out of 92) and postinfarct cardiosclerosis (PICS) in 2.2% (2 out of 92) of patients, chronic heart failure (CHF) in 6.5% (6 out of 92) of patients. Combined cardiovascular pathology was observed in 16.3% (15 out of 92) of patients. Cerebrovascular disorders were detected in 3.3% (3 out of 92).
The electrocardiographic changes detected in patients with PsA, signal the presence of cardiovascular diseases in the early or advanced stage, which can decisively influence the prognosis of the disease. The detection through this routine paraclinical examination of the changes occurred on the electrocardiogram can determine a prompt and correct therapeutic attitude to alleviate cardiovascular disorders, complications that can become aggravating risk factors in the evolution of PsA. Starting from these data, we followed the early detection of cardiovascular complications in patients with PsA by performing a simple, routine paraclinical examination (electrocardiogram), with the establishment of correlations between electrocardiographic changes and clinical-evolutionary type, as well as laboratory, as well as between electrocardiographic changes and the mechanisms by which PsA determines cardiac damage.
In order to elucidate the causes of heart disease, we focused our attention on the presence of a chronological relationship when they appear with the development of joint or tegumentary syndrome or their aggravation, the diminishing of cardiac symptoms and the regression of exacerbations under anti-inflammatory treatment, excluding other associated heart diseases.
In the result of our study at ECG were recorded signs of rhythm and conduction disorders, which were expressed by supraventricular extrasystoles (26% patients) and ventricular (8% cases), paroxysmal tachycardia (in 6% people), atrial fibrillation (8% pts), sinus tachycardia (10% pts), sinus bradycardia (in 16% patients), atrioventricular block of I and II degree (22% cases), right ram block of the Hiss beam (16% pts), anterior left ram block (in 10% pts), complete block of left ram of the Hiss beam (in 8 cases), CLC syndrome (in 4% persons). Signs of left ventricular hypertrophy were determined in 50% of patients with PsA, right ventricle – at 34%, left atrium – at 26%, right atrium – at 10%. Diffuse myocardial changes were also detected by repolarization disorders (64%), QT prolongation (18% sick). Quite frequently (14% patients) the syndrome of early ventricular repolarization was diagnosed. These data are relatively comparable to those of the literature.
Echocardiography is the most used imaging technique in clinical cardiologic practice, bringing useful information on the structure, cardiac and vascular function. In addition, this technique has a direct influence on the diagnosis and therapeutic management of the evaluated patient, being able to dictate the therapeutic decisions, evaluate the response to the initiated therapy, and finally yet importantly provide predictive data on the patient's evolution. The advantages of echocardiography recommend it as a routine imaging technique for diagnosing and tracking most cardiovascular diseases. Two-dimensional (2D) echocardiographic imaging can accurately assess the size of cardiac cavities and main vessels, wall thickness, ventricular function and valves anatomy. Doppler echocardiographic techniques bring information related to blood flow velocity, intracardiac pressures, and hemodynamic characteristics, thus detecting and quantifying stenosis, regurgitations, and other abnormalities of blood flows. Thus, over time, echocardiography has replaced many other technologies with a role in establishing clinical decisions, but also in assessing structural and functional changes after therapeutic interventions.
Therefore, according to the data of the literature, in PsA the damage of the valvular apparatus occurs with the possible formation of valve rheumatic disease. It should be noted that in the result of our study, transient endocarditis was confirmed in a patient with PsA by detecting temporary reduction of diastolic blast amplitude at the apex and in the projection of the mitral valve, and the existence of valvulitis in another patient with such nosology was confirmed echocardiographically by simultaneous dysfunction of the mitral valve cusp and moderate dilation of the left ventricle. In 21 patients were identified ultrasound changes suggestible for valvulopathy, among these people were 12 men and 9 women. In 2 cases, isolated mitral insufficiency was found, in 6 patients - isolated aortic insufficiency. Associated mitral valvulopathy was observed in 4 patients, combined mitral-aortic valvulopathy – in 9 cases. Associated mitral valvulopathy was detected only in women, aortic – it was encountered with equal frequency in men and women. The skin manifestations in patients with valvulopatii were presented with vulgar psoriasis limited to 3 people, disseminated vulgar psoriasis – in 10, exudative psoriasis – in 4 and atypical psoriasis, respectively, in 2 cases.
Thus, the cardiac syndrome in patients with PsA is characterized by the diversity of its manifestations and presents changes in different structures of the heart and aorta. The damage to the myocardium proceeds as a type of myocarditis and cardiomyopathy, similar to the dilated one. In rare cases there may be deposits in cardiac tissues of the eosinophilic protein as one of the localizations of generalized reactive amyloidosis. Myocarditis is characterized by minor symptoms and usually does not lead to heart failure. Adhesive pericarditis is more common in patients with marked changes in the axial skeleton. It correlates with laboratory activity, the presence of systemic manifestations, as well as other cardiac symptoms, and, especially, with aortitis. The deterioration of the valvular apparatus is expressed in the development of organic diseases of the heart. In PsA there is aortic regurgitation, combined mitral-aortic valvulopathy and mitral stenosis. Aortic insufficiency in patients with psoriasis is more common in ankylosing spondyloarthritis and, as a rule, is a consequence of the underlying disease. The genesis of mitral-aortic valvulopathy or associated mitral valvulopathy are probably associated with rheumatic carditis, although it is difficult to exclude the possibility that they may be the result of psoriatic carditis. The most important stigma of cardiac syndrome is aortitis and particularly well correlates with sacroiliitis and psoriatic spondyloarthritis.
Patients with psoriatic arthritis, according to the latest opinions, have an increased risk of cardiovascular morbidity and mortality, particularly through coronary artery disease [1, 2]. According to D.Gladman, the most vulnerable subjects are those with severe and active forms of psoriatic arthritis [4]. In the Republic of Moldova, in the structure of the general mortality of the population, cardiovascular diseases are on the first place, constituting 55,8% of the total number of deaths. In 2019, 444,977 patients with diseases of the circulatory system were registered in the Republic of Moldova (2006 – 353,751). The incidence through diseases of the circulatory system in 2019 was 154.09 per 10,000 population. The control of traditional cardiac risk factors contributes, along with the control of inflammation, to the prevention of cardiovascular events. The high-risk strategy involves both the screening of the general population to identify patients at high risk of developing CVD and the establishment of preventive strategies recommended for patients with high CV risk. The identification of high-risk patients is recommended to be based on the global CV risk assessment by using SCORE (Systematic Coronary Risk Evaluation) risk charts, which meet and correlate the statistical data of several large European prospective studies, and allow the prediction of fatal atherosclerotic events over a period of 10 years. The risk factors taken into account are: sex, age, smoking, systolic blood pressure, total cholesterol (CT) and geographical region (Moldova being part of high-risk populations in Europe). However, cardiovascular prevention measures, although clearly established by medical practice guidelines [6], are insufficiently applied both in the general population [8] and among patients affected by PsA [6, 16].
Therefore, we set out to determine, in the entire group of patients with PsA, the prevalence of traditional cardiovascular risk factors, the level of cardiovascular death risk at 10 years and the rate of treatment and therapeutic control of hypertension (HTN) and dyslipidemia. Thus, patients with high cardiovascular risk were considered those who meet at least one of the conditions: the presence of organic cardiovascular disease, the presence of diabetes mellitus (DM) or a cardiovascular risk of death in the next 10 years of over 5%. The estimation of this risk was also made for patients with PsA, but without diabetes mellitus, based on the SCORE table, which takes into account age and sex, smoking status, blood pressure and cholesterol levels [3]. The variant was used for populations with high cardiovascular risk recommended. In line with EULAR recommendations for inflammatory arthritis [3] and the International Society of Psoriasis and Psoriatic Arthritis [6], the ratio of total cholesterol to HDL-cholesterol was used and the risk was multiplied by 1,5 for patients with SPA who met at least two of the following conditions: long duration of disease evolution, positivity after HLA-B27 and extraarticular manifestations. The most frequently objectified cardiovascular risk factors at the level of the studied group were dyslipidemia, HTA developed after 5 years from the onset of the disease and abdominal obesity, as well as HTA, occurring at 5 years of basic joint disease.
Out of the total number of persons evaluated in the CV screening, in order to identify patients with cardiovascular risk factors, according to the criterion of systolic blood pressure value (SBP), the examined persons were distributed in the following way: with SBP <130 mmHg – 10% and with SBP 130-139 mmHg are 14%, people with SBP 140-159 mmHg constitute 34%. At the same time, the following increased values of SBP were registered: patients with SBP 160-179 mmHg constituted 24% and respectively with SBP ≥180mmHg constitute 18% of the total patients evaluated. According to the analysis of diastolic blood pressure (TAD) data, the examined persons were distributed in the following way: patients with TAD < 85 mmHg constitute 10%, with TAD 85-89 mmHg – 28%, with TAD 90-99 mmHg – 44%, with TAD 100-109 mmHg – 12% and with TAD ≥110mmHg constitute 6% of the total evaluated patients.
According to the results of the analysis of cholesterol data presented for each patient in the general study group with PsA, it results that: 20% of the patients presented the total cholesterol value < 5.0 mmol/l, 18% - the total cholesterol value 5.0-5.9 mmol/l, 54% of the patients presented the total cholesterol value < 5.0 mmol/l, 4% - 7.0-7.9 mmol/l and 4% - ≥ 8.0 mmol/l. Being asked to answer the question of whether they are undergoing antihypertensive treatment, the patients evaluated during the CV screening: 62% of the evaluated persons mentioned that they had never followed antihypertensive treatment, and 38% at the time of the evaluation were undergoing antihypertensive treatment.
The SCORE risk values were calculated according to the SCORE EUROPA High Risk Chart (the risk of fatal CVD at 10 years in the regions of Europe with high risk according to sex, age, systolic blood pressure, total cholesterol and smoking). As a result of the calculations performed, it was found that: patients with the risk score <5,0% - constitute 20%, persons with risk SCORE 5,0-9,9% - constitute 44%, patients with risk SCORE 10,0-14,9% - constitute 28%, and persons with risk SCORE ≥15% - constitute 8%.
The frequent medical checks required for patients with SPA (especially those with highly active forms of the disease) are an opportunity that should not be missed for the detection and correction of cardiovascular risk factors in this subpopulation with increased morbidity and cardiovascular mortality.
Discussions
Patients with PsA of young and middle age are a special category of patients of working age, therefore, a timely evaluation of CP and PsA activity and quality of life is paramount in the management of these patients, given the significant impact of PsA on the quality of life of patients.
Data from the literature on CP evaluation in patients with young and middle age PsA are limited. Overall, CP frequency was comparable to the results of previous studies, despite the fact that the average age of patients in these studies was higher.
In the study, Lubrano et al. [81] (n=144, average age56.6±13.4), at least 1 CP was observed in 104 (72.2%) patients with PsA, which was comparable to the results of their study (71 patients, 77.2%), despite the older age of patients in this study.
In the CP structure of patients with medium and young age PsA prevailed hypertension (38%), obesity (25%), gastrointestinal diseases (41,3%), other diseases of the musculoskeletal system not associated with psoriasis (42,4%). On average, these data were comparable to recently published meta-analysis data, despite the absence of age segregation. The lower incidence of cardiovascular pathology in middle-aged and young patients in the study can be explained by the younger age of patients for the development of this group of diseases. The incidence of cardiovascular disease was high and comparable to the results of a recent study [4, 16], although to date, some studies have generally shown a decrease in the incidence of cardiovascular lesions (less than 5%) in patients with rheumatic diseases compared to the general population [14, 15].
When evaluating the association of CP in patients with SPA with quality of life, it was found that with the increase in the number of comorbid conditions in patients with young and middle-aged PsA, the general state of health (SF-36 questionnaire scale), physical functioning (HAQ-DI) and the quality of life associated with PsA (PsAQoL, p<0.05) deteriorated.
When evaluating the differences between the groups according to the number of CP, it was found that in the group with 2 CP and more, the patients were older, had BMI, CC, CT, lifted, being risk factors for CVD.
Among the clinical indicators, the number of large painful joints was higher in the group of patients with 2 CP or more. In the same group, there was a greater number of enthesitis (p<0.01), NAT (p<0.05), NAD (p<0.01), as well as a greater number of joints with osteophytes (p<0.01), while there were no differences in laboratory work (ESR, hs-PCR, p>0.05). These results suggest an increase in enthesitis and subclinical synovitis, with an increase in the number of CP and the number of joints with osteophytes that increase with age.
Conclusions
In patients with PsA of young and middle age, a high frequency of comorbid pathology was observed: in 60.9% of patients, more than one comorbid pathology was observed, with the highest frequency were recorded diseases of the musculoskeletal system (42.4%), cardiovascular (41.3%) and diseases of the digestive system (41.3%). Due to the high frequency of comorbid pathology in PsA at young and medium age (60.9%), patient management should be carried out by a rheumatologist and internist together with doctors of related specialties for the timely diagnosis and treatment of comorbid diseases.
Competing interests
None declared
Author’s ORCID ID
Lucia Dutca, https://orcid.org/0000-0002-1815-2294
References
Groppa L., Popa S., Rotaru L. et al. Reumatologie și nefrologie. Manual. Lexon Prim, Chișinău, 2018. 462 p.
Protocolul Clinic Național „Artrita psoriazica la adult”, PCN- 295; 2018, pag 3 - 25
Gossec L, de Wit M, Kiltz U, et al. A patient-derived and patient-reported outcome measure for assessing psoriatic arthritis: elaboration and preliminary validation of the Psoriatic Arthritis Impact of Disease (PsAID) questionnaire, a 13-country EULAR initiative. Ann Rheum Dis 2014;73:1012–9
Taylor W, Gladman D, Helliwell P, et al. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum 2006;54:2665–73
Ritchlin CT, Kavanaugh A, Gladman DD, Mease PJ, Helliwell P, Boehncke WH, et al. Treatment recommendations for psoriatic arthritis. Ann Rheum Dis. 2019 Sep;68(9):1387- 94
Taylor WJ. Impact of psoriatic arthritis on the patient: through the lens of the WHO international classification of functioning, health, and disability. Curr Rheumatol Rep. 2021;14:369–374
Kalyoncu U, Ogdie A, Campbell W, et al. Systematic literature review of domains assessed in psoriatic arthritis to inform the update of the psoriatic arthritis core domain set. RMD Open. 2016;2:e000217
World Health Organization. International Classification Of Functioning, disability and health (ICF) [Internet]; [cited 2017 Dec 2]. Available from: www.who.int/classifications/icf/en/
Cieza A, Brockow T, Ewert T, Amman E, Kollerits B, Chatterji S. Linking health-status measurements to the international classification of functioning, disability and health. J Rehabil Med. 2002;34:205–10
Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustün B, Stucki G. ICF linking rules: an update based on lessons learned. J Rehabil Med. 2020;37:212-8
Stucki G, Cieza A, Geyh S, Battistella L, Lloyd J, Symmons D, et al. ICF Core Sets for rheumatoid arthritis. J Rehabil Med. 2020;44 Suppl:87-93
Boonen A, Braun J, van der Horst Bruinsma IE, Huang F, Maksymowych W, Kostanjsek N, et al. ASAS/WHO ICF Core Sets for ankylosing spondylitis (AS): how to classify the impact of AS on functioning and health. Ann Rheum Dis. 2019;69:102-7
Ewert T, Fuessl M, Cieza A, Andersen C, Chatterji S, Kostanjsek N, et al. Identification of the most common patient problems in patients with chronic conditions using the ICF checklist. J Rehabil Med. 2014;44 Suppl:22-9.
van Echteld I, Cieza A, Boonen A, Stucki G, Zochling J, Braun J, et al. Identification of the most common problems by patients with ankylosing spondylitis using the international classification of functioning, disability and health. J Rheumatol. 2017;33:2475-83.
Pariser D, Schenkel B, Carter C, Farahi K, Brown TM, Ellis CN; Psoriasis Patient Interview Study Group. A multicenter, non-interventional study to evaluate patient reported experiences of living with psoriasis. J Dermatolog Treat. 2016;27:19-26.
Feldman SR, Malakouti M, Koo JY. Social impact of the burden of psoriasis: effects on patients and practice. Dermatol Online J. 2014;20(8).