Introduction
Prostate lithiasis is a common complication of chronic nonbacterial prostatitis (CNBP), commonly encountered in urological practice and which hasn’t been studied extensively in clinical practice. CNBP with complications of lithiasis is often incidentally detected in various areas of the parenchyma during examination of patients with lower urinary tract symptoms (LUTS), having a persistent opacity, usually interpreted as prostate stones [1, 2, 3]. Lithiasis of the prostate is a condition in which calculi are formed in the tissue of the gland or in the excretory ducts [4, 5]. It is assumed that the prostate stone is formed due to a prolonged inflammatory process caused by the precipitation of prostate secretions and calcification of amyloid bodies, intraprostatic reflux
with difficulty urinating, leading to clinical prostatitis [6, 7]. It has been considered that the incidence of prostate stones increases with the patient’s age [6, 8]. However, a number of scientific works have determined a clinical correlation between the prostatic calculi formation and the syndrome of chronic pelvic pain followed by symptoms of the lower urinary tract in young men [8].
Before ultrasound was introduced into practice, the prostatic calculi were almost impossible to diagnose, being based only on digital rectal examination, which found stones in isolated cases [9]. Recently, the number of patients diagnosed with prostate cancer has significantly increased due to the introduction of transrectal ultrasound scanning (TRUS) into clinical practice [10]. According to some authors, up to 80% of prostate stones are found in men over 50.
Many authors report that prostate stones cause nonspecific lower urinary tract symptoms (LUTS) [10, 11], therefore, it was found that prostate stones can ause prostatitis, which leads to and worsens LUTS [12].
Patients with CNBP-associated prostate stones require conservative anti-inflammatory treatment in combination with transurethral incision or resection of the prostate to eliminate bladder obstruction and remove prostate stones
[13]. Stones that cause bladder outlet obstruction (BOO ) and / or stones in benign prostatic hyperplasia can be removed by various methods of transurethral resection [6, 9, 10, 13].
Material and methods
The study is based on clinical and laboratory surveillance and research, performed in 40 patients aged 51-70 years (mean age – 60.5 years) with prostate stones due to PCAB.
The study was carried out within the Department of urology and surgical nephrology, N. Testemitanu State University of Medicine and Pharmacy, and Public Medical Institution Republic and Clinical Hospital „Timofei Moşneaga”.
The study is based on clinical and laboratory observations and studies conducted in 40 patients aged 51 to 70 years (mean age 60.5 years) with prostate stones caused by CNBP.
The study inclusion criteria comprised patients with bladder outlet obstruction, caused by chronic nonbacterial prostatitis with prostate stones, in some cases associated with clinically and paraclinically confirmed benign prostatic
hyperplasia (BPH) and prostate sclerosis (SP). The surgeries were carried out by several endoscopic methods, depending on the anatomical and structural state of the prostate and its adjacent tissues, determined as a causal factor of the present symptoms and the persistence of the disease, in order to obtain the maximum effect. In order to determine the clinical efficacy of endoscopic transurethral resection techniques, as well as the most convenient time and choice for the optimal method to be performed, depending on the patients’ age, their functional body status and gland, comorbidities, a study of parameter changes was conducted, analyzing mean values of the maximum urine flow rate, symptomatic parameters on the scale of urination disorders and quality of life, residual urine and prostate volume prior to surgery, as well as 1 and 3 months after the surgery. In order to remove the bladder outlet obstruction in lithiasis-associated CNBP, taking into account the importance of the evolution of these parameters and determining intra- and postoperative complications, transurethral resection (TUR) and Ho:YAG laser was performed within the established follow-up time.
According to the preoperative examination data, the groups of patients were divided according to the type of surgery performed: transurethral resection (TUR) (n = 10) and Ho: YAG-laser resection of prostate stones.
Results
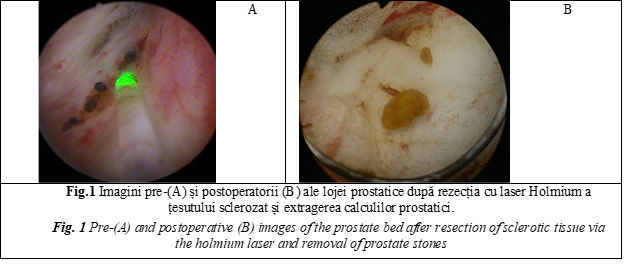
For the first time, 30 patients with complaints of difficulty urinating (bladder outlet obstruction and residual urine) were subjected to transurethral resection of the prostate with a Ho:YAG laser, at an operating mode with pulse energy of 2.3 J and a frequency of 18 Hz, at maximum power of 18.4 W. Laser incisions were performed at 5 and 7 o’clock in the standard quadrant with resection of the sclerotic prostate tissue and removal of prostate stones (Figure 1). The results obtained with Ho: YAG laser transurethral resection of the prostate were compared and determined before the intervention as well as 1 and 3 months after the operation (Table 1). The results obtained via the transurethral resection of the prostate with the Ho: YAG laser were compared and determined before the intervention and 1 as well as 3 months after the surgery (Table 1).
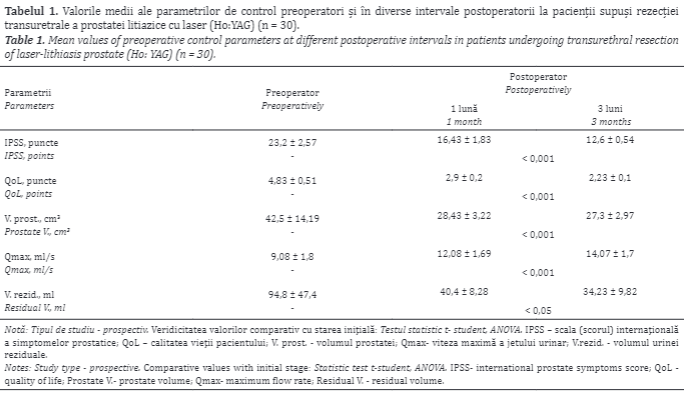
The mean duration of the intervention was 25.7 minutes (from 15 to 35 minutes), while the mean duration of catheterization lasted 12 hours. During a 3- month follow-up, it was found that the mean IPSS has significantly improved from 23.2±2.57 points at the beginning of the study to 12.6±0.54 points after the intervention. The median quality of life parameter also changed from 4.83±0.51 points to 2.23±0.1 points (p <0.001). The maximum urine flow rate improved from 9.08±1.8 ml/s before surgery to 14.07±1.7 ml/s after surgery. No patient required a repeated surgery. The mean residual urine value significantly decreased after surgery (94.8±47.4 ml versus 34.23±9.82 ml; p <0.001). After tissue resection with the Ho: YAG laser, prostate volume also decreased from 42.5±14.19 cm3 to 27.3±2.97 cm3 after surgery
Commonly, the frequency of complications of Holmium laser resection is low. The following intraoperative complications were found: perforation of the prostate capsule - 1 case, damage of the bladder neck walls during fragmentation - 1 case, haemorrhage - 1 case, damage to the urethral meatus - 1 case, incomplete perforation in the trigone area of the bladder - 2 patients. Repeated transurethral reoperation was required to remove the remaining prostate tissue - 1 patient. Postoperatively, the following complications were
determined: transient urinary incontinence over 3 weeks - 2 patients, stress urinary incontinence - 1 patient, bladder mucosa injury occurred in 1 case with larger prostate, 1 patient suffered a bladder neck incision due to the bladder stricture. Orchiepididymitis also occurred.
Urinary incontinence usually resolved spontaneously within 3 weeks. Symptoms of irritation were present in 28% of patients within 1 month after surgery and in 10% within 3 months. However, the symptoms commonly went away on their own and were treated with non-steroidal anti-inflammatory drugs. According to specialized literature, these complications are typical for Ho: YAG laser resection and patients should be properly informed to achieve good postoperative interaction [14, 15, 16].
Another endoscopic method of treatment, namely, the transurethral resection of the prostate (TURP) with removal of stones, was performed in 10 patients with prostatic calculi due to CNBP (Figure 2). A comparative analysis of the
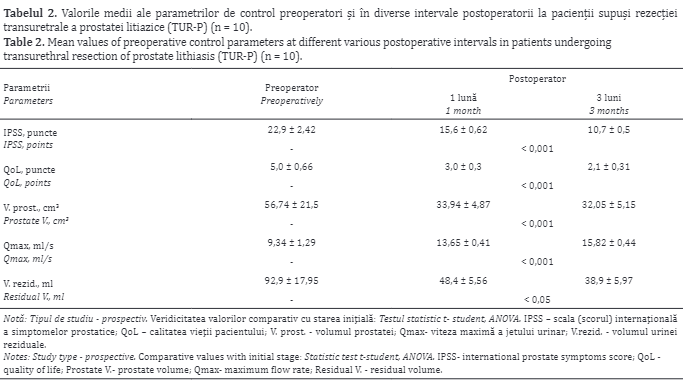
changes in the following parameters was performed: Qmax, IPSS, QoL, prostate volume and residual volume, as well as by determining their evolution in the same periods (before and at 1 and 3 months after surgery). The dynamic changes in patients’ subjective symptoms (IPSS and QoL), as well as of the objective parameters (Qmax, volume of residual urine and prostate) are shown in Table 2.
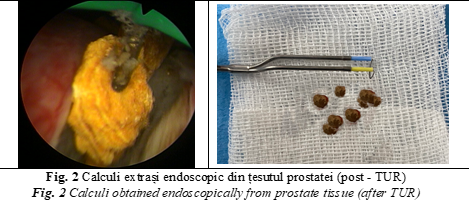
The main TURP methods applied to patients were the transurethral incision of the prostate (TUIP), transurethral resection of the prostate (TURP), subtotal resection of the prostate, and a combination of these methods. Incision and transurethral resection of the prostate, aimed at regulating the restraining organ processes, which were underlying the disease clinical evolution, were performed by minimally removal of prostate tissue. Thus, the causal factor of secretion retention was eliminated via incision or transurethral resection, whereas the stagnant content of glandular ducts was eliminated by open surgery (Figure 2).
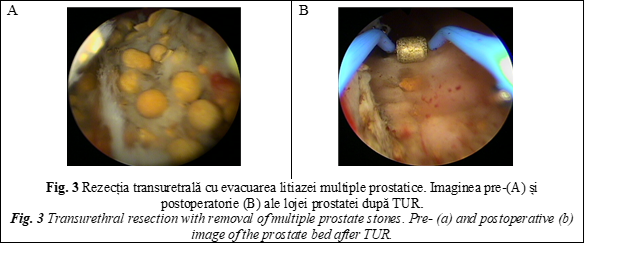
If multiple calculi or sclerotic foci were found within the prostate, the subtotal resection was performed to remove the whole organ tissue, as well as of the detected calculi (Fig. 3).
The mean surgery duration was 35 minutes; the mean time of bladder atheterization was 24 hours. During the follow-up, it was found that the mean IPSS value improved from 22.9±2.42 to 10.7±0.5 points. The quality of life ndex also improved from 5.0±0.66 points to 2.1 ± 0.31 points (p <0.001). Qmax improved from 9.34±1.29 ml/s to 15.82±0.44 ml/s after the intervention. The mean residual urine value decreased from 92.9±17.95 ml to 38.9±5.97 ml (p
<0.001). Following the Ho: YAG laser resection, there was also a decrease in prostate volume from 56.74±21.5 cm3 to 32.05±5.15 after surgery.
All patients in the early postoperative period showed no complications and almost no bleeding was recorded. However, during the first follow-up examination, a significant improvement in subjective symptoms, an increase in Qmax
indicators and the lack of residual urine were revealed (Table 2).
Consequently, transurethral resection of lithiasis in chronic nonbacterial prostatitis showed a high clinical efficiency, manifested with significant recovery of micturition. The high values of efficacy and safety allow considering these methods as effective treatment in lithiasis-associated CNBP.
The main advantage of TUIP over TURP, are particularly appropriate for younger patients, but which needs to be considered in the elderly as well, due to a lower rate of retrograde ejaculation. If, in TURP, the frequency of retrograde ejaculation is about 50-95%, then in TUIP this value sharply decreases, reaching even less than 10%. Since the operation length is relatively shorter in TUIP, hydroelectrolytic disturbances are not encountered or mentioned in any important study. TUIP as a method of treatment is performed much faster than TURP and requires a significantly less amount of liquid for washing. Severe bleeding requiring blood transfusion is extremely rare in patients with TUIP [15, 16, 17, 21, 22].
Therefore, the clinical efficacy of holmium laser resection (Ho: YAG) and monopolar transurethral resection of the prostate (TURP) are comparable. However, unlike TURP, the holmium laser resection is not limited by prostate volume and can be carried out in various gland sizes. At the same time, this method provides a lower risk of bleeding during the intra- and postoperative period, excluding the „water intoxication” syndrome, helping reduce the occurrence of infectious and inflammatory complications by shortening the time of the urethral catheterization and the period of patient’s hospital stay. At the same time, we consider that holmium laser resection of the prostate is an effective and safe surgical approach of BOO, caused by CNBP, as well as of
its consequences, followed by rapid recovery of urine quality and may be available to all categories of patients. Based on the obtained results, we conclude that the use of laser resection is possible in patients with various-sized prostate glands, provided that the technical possibilities of using a morcellator are available. Laser interventions can also be performed in patients with coagulopathies, chronic renal failure, chronic dialysis, and obstructive CNBP. Laser resection has some additional benefits due to less blood loss and shorter urethral catheterization time. The incidence of complications of Ho: YAG laser resection is generally low. These relevant successful results of Ho: YAG resection have been reported by several clinical centres [11, 18, 19, 20].
One of the disadvantages of Ho:YAG is the operating time if compared to TURP, which is faster then Ho:YAG operation technic. The comsumtion time needed for laser resection is significantly higher due to the removal of resected tissue or stones (bulky or multiple), since the size of the removed fragments is limited by the size of the urethra. To overcome the difficulties encountered in Ho: YAG resection, a transurethral morcellator model was created. Thus, the change in the resection technique enabled to fragment the
removed tissue inside the bladder. This allows the complete extraction (middle and lateral lobes of the prostate) of the prostate tissue together with the prostate stones, without dividing the removed tissue into smaller parts, a processes requiring a longer time duration. As a result, the possibility of tissue removal increases, while the manipulations are minimally invasive. Absolute contraindications for transurethral resection via holmium laser include the patient’s severe condition, the decompensated condition of the vital organs, and presence of acute inflammatory diseases, which are no exception and are characteristic of any other elective surgery. The intervention cannot be carried out if it is technically impossible to insert the resectoscope through the urethra into the bladder (ankyloses of the hip joints, pronounced and enlarged urethral stricture). A relative contraindication is the presence of a microcyst in the patient, which can interfere with the safety of tissue fragmentation.
Therefore, the choice of optimal treatment of lithiasis in bladder outlet obstruction also depends on the technical equipment of the clinic, the patient’s will, the presence of recurrent complications, the drugs that the patient administers.
Conclusions
1. Transurethral endoscopic interventions are the methods of choice in the surgical treatment in lithiasis-associated CNBP, regardless of the size, volume and location of prostatic calculi, as well as in other possible pathologies (BPH, SP, etc.).
2. Transurethral incision and resection are effective and safe surgical methods in treatment of patients with lithiasis-associated CNBP, followed by a lower incidence of injuries, complications and significantly lower mortality rate,
showing the same effectiveness as those used before.
3. Laser transurethral endosopic interventions (laser resection and enucleation), being both minimally invasive and safe treatment methods, can be used as an alternative surgical approach to standard monopolar TURP in patients with lithiasis-associated CNBP, as well as in cases of BOO with lower urinary tract symptoms. Laser resection is characterized by a less invasive and traumatic nature, lack of haemorrhagic complications, urinary incontinence and “water intoxication syndrome”, showing an immediate (instantaneous) response, and being characterized by objective and subjective improvement of patients’ condition, without diminishing its efficiency if compared to patient’s outcomes found after TURP. Holmium laser resection is not limited to the size of the prostate and is likely to be carried out in patients with lithiasis-associated CNBP of various sizes and volume and in those for whom
transurethral electroresection or open adenomectomy is contraindicated, especially in patients taking anticoagulants, or those at high risk of developing cardiovascular complications. The incidence of late complications is lower and less pronounced compared with TURP.
4. Transurethral endoscopic treatment includes a variety of methods including transurethral incision and resection, laser incision and resection that are recommended for complications of BOO-associated CNBP and which minimize
their risk, being considered minimally invasive and safer for the patient. Choosing them correctly, depending on the BOO caused by the consequences of untreated CNBP, which increases the successful rate of interventions and minimizes the risk of complications. The high efficiency and low invasiveness of endoscopic interventions enabled to expand the indications for their use, and in some cases to become the methods of choice in treatment of a number of urological diseases and their complications. It is considered that patients with CNBP suffering from urinary disorders (like BOO), should be first suspected of prostate sclerosis , stones, etc. Due to the recent implementation and equipping the urology clinics with minimally invasive technologies, most
patients with BOO caused by CNBP should undergo an endoscopic treatment.
Competing interests
None declared
Authors’ contribution
Both authors contributed equally to the research, data analysis, and writing of the manuscript. Both authors read and approved the final article.
Authors’ ORCID IDs
Artur Colța, https://orcid.org/0000-0002-1291-1237
Vitalii Ghicavîi, https://orcid.org/0000-0002-2130-9475
References
Bedir S., Kilciler M., Akay O. et al. Endoscopic treatment of multiple prostatic causing urinary retention. Int. J. Urol., 2005; 12 (8): 693-695.
Cao J. J., Huang W., Wu H. S., Cao M., Zhang Y., Jin X. D. Prostatic calculi: Do they matter? Sexual medicine reviews, 6(3), 482-491, 2018.
Fei X., Jin W., Hua S., Song, Y. Prospective study on association of prostatic calcifications with clinical symptoms and results of treatment in men with type III prostatitis. Scientific reports, 7(1), 1-6, 2017.
Geavlete P. A. Endoscopic Diagnosis and Treatment in Prostate Pathology: Handbook of Endourology. pg 218. Academic Press; 1st edition. January 26, 2016.
Geavlete P., Niţă G., Persu C., Geavlete B. Endoscopic Treatment of Prostatic Lithiasis. In Endoscopic Diagnosis and Treatment in Prostate Pathology. Academic Press. pp. 195-202, 2016.
Geramoutsos I., Gyftopoulos K., Perimenis P. et al. Clinical correlation of prostatic lithiasis with chronic pelvic pain syndromes in young adults. European urology, 45(3), 333-338, 2004.
Grigore N., Pîrvuţ V., Mihai I., Haşegan A. Prostate Lithiasis. Acta Medica Transilvanica, 22(2), 2017.
Hyun J. S. Clinical significance of prostatic calculi: a review. The world journal of men's health, 36(1), 15-21, 2018.
Kim S. H., Jung K. I., Koh J. S. et al. Lower urinary tract symptoms in benign prostatic hyperplasia patients: orchestrated by chronic prostatic inflammation and prostatic calculi? Urologia internationalis, 90(2), 144-149, 2013.
Kim W. B., Doo S. W., Yang W. J., Song, Y. S. Influence of prostatic calculi on lower urinary tract symptoms in middle-aged men. Urology, 78(2), 447-449, 2011.
Park S. W., Nam J. K., Lee S. D., Chung M. K. Are prostatic calculi independent predictive factors of lower urinary tract symptoms? Asian Journal of Andrology,12(2), 221, 2010.
Popescu N., Dragoescu P. O., Tiu C. Correlation of sonografic findings with clinical presentation and surgical management of prostatic lithiasis. Ultraschall in der Medizin-European Journal of Ultrasound. 28(S 1), P-14-3, 2007.
Priyadarshi V., Sehgal, N. A completely calcified prostate. Urology annals, 8(4), 468, 2016.
Shoskes D. A., Lee C. T., Murphy D., Kefer J., Wood H. M. Incidence and significance of prostatic stones in men with chronic prostatitis/chronic pelvic pain syndrome. Urology, 70(2), 235-238, 2007.
Гусейнов Ф. И. Камни предстательной железы у больных аденомой и раком простаты. Автореферат дисс. канд. мед. наук. Москва, 2013
Soric T. et al. Clinical and biochemical influence of prostatic stones. Urologia internationalis. 2017, Volume 98, Issue 4: 449-455.
Venyo A. K. G. Prostatic calculi: a review of the literature. 2012
Wang H., Ma M., Qin F., Yuan, J. The influence of prostatic calculi on lower urinary tract symptoms and sexual dysfunction: a narrative review. Translational Andrology and Urology, 10(2), 929, 2021.
Yucel C., Budak S. Association between large prostate calculi and prostate cancer. Archivio Italiano di Urologia e Andrologia, 90(3), 181-183, 2018.
Гусейнов Ф. И. Камни предстательной железы у больных аденомой и раком простаты. Автореферат дисс. канд. мед. наук. Москва, 2013.
Джапаров Ж.Т., Усупбаев А.Ч. и др. Доброкачественнaя гиперплазия предстательной железы в сочетании с хроническим калькулезным простатитом. Вестник КРСУ. 2017. Том 17. №10, c. 26-28.
Усович А.К., Краснобаев, В. А. Особености структурной организации мышечной ткани и образование конкрементов в простате человека. Новости хирургии. 2012. Т. 20. №4., c.81-86.

