Introduction
Gout, one of the most frequent types of inflammatory arthritis, is a metabolic disease characterized by the deposition of monosodium urate in different tissues. Monosodium urate is the final metabolite of uric acid, and it is formed in the supersaturated fluids of the body [1, 2]. There a multiple research studies that proved the increasing prevalence of gout in the last decades [12]. Therefore, the latest data shows us 5% of males and 2-3% of females around the world are suffering from hyperuricemia [3, 4]. Only 10% of people suffering from hyperuricemia will develop gout. There is a higher prevalence of gout in elderly people. Subjects older than 75 years old have a prevalence >7% in males and <4% in females [5, 6]. In Republic of Moldova, the following data has been observed: 2,5% of population is affected by asymptomatic hyperuricemia, but morbidity varies between 0,3 – 2,1% [11, 13]. Studies that focused on the natural evolution of gout before the availability of hypouricemic agents showed that up to 25% of subjects with gouty arthritis developed proteinuria, 50% renal dysfunction, and 10-25% developed end-stage kidney disease [7, 8]. The most important site where urate crystals are deposited is in the kidney [9, 10]. Histological changes are particularly frequent and have been noticed in autopsy studies at 75-99% of patients with gout.
Materials and methods
Description of two clinical cases of patients with gout - male and female who were hospitalized in the „Timofei Mosneaga” Republican Clinical Hospital and “Saint Trinity” Municipal Clinical Hospital in 2021.
Results and discussion
1st clinical case
Patient C, male, born in 1959, from Chisinau, Codru, was brought by the Emergency Medical Services to the “Saint Trinity” Municipal Clinical Hospital and admitted in Intensive Care Unit on 28-Jun-2021 with the diagnosis: cardiomyopathy, acute kidney injury of unknown cause. At initial examination – patient in severe condition, with bradyphrenia. Patients complained of dyspnea at mild exertion, severe fatigue, 5-day anuria and generalized edema. From the history collected from relatives, it was discovered that the patient has been diagnosed with gout a few years ago, and was administering treatment only in crisis, usually with non-steroidal anti-inflammatory drugs and painkillers. Patient did not have any history of allergies.
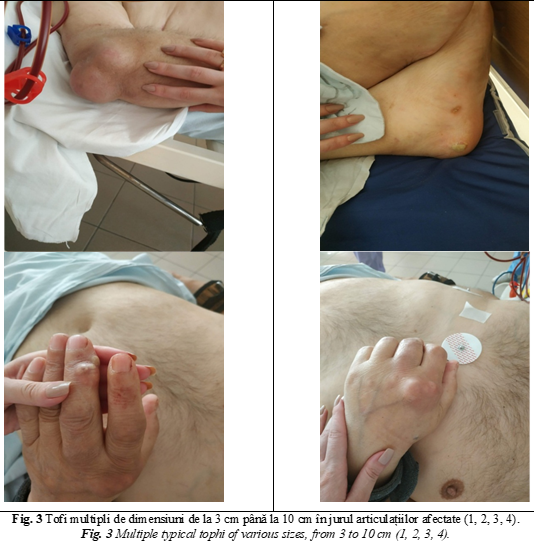
At physical examination: general status serious, bedridden, pale skin, acrocyanosis, severe pitting edema on the upper and lower limbs, multiple tophi up to 10 cm in the elbow regions, and up to 5 cm in the bilateral metacarpophalangeal joints. Lymph nodes not palpable. Difficult nasal breathing, at auscultation of the lung bilateral ronchi. Respiratory rate (RR) – 24 respirations per minute, peripheral oxygen saturation (SpO2) – 90%. Normal precordium, heart sounds of lower intensity, normal heart rhythm. Blood pressure (BP) – 225/110 mmHg Heart rate (HR) – 82 beats per minute. The oral tongue is moist, bloated abdomen, enlarged in volume due to adipose tissue. No signs of ascites and caput medusae. The liver is palpated at the costal margin. Normal stool frequencies. Peritoneal signs are absent. Anuria, bilateral costovertebral angle tenderness. Patient is obnubilated with temporal and spatial disorientation. Pupillary eye reflexes normal.
Presumptive diagnosis: Acute kidney injury of unknown cause. Chronic tophaceous gout. Gout nephropathy. Mixed chronic cardiomyopathy (hypertensive, metabolic, ischemic). Hypertensive crisis (28-Jun-2021). Hypertension grade 3. Chronic heart failure (CHF) grade II NYHA.
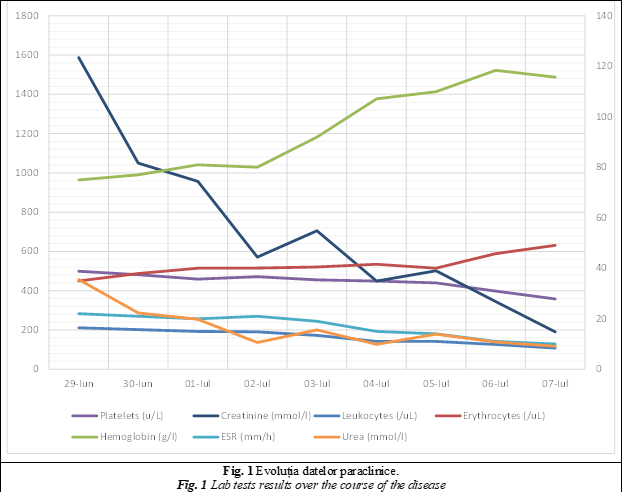
The following lab tests were performed: complete blood count, biochemical tests of the serum. A Folley catheter has been installed. The lab tests are presented in table 1.
Tabelul 1. Datele paraclinice a pacientului. Table 1. Patient lab values. | ||
Componentul investigat Parameter | Rezultatul Results | Valori de referință Reference values |
Leucocite White blood cells | 16,33 /Ul ↑ | 4,00-9,00 |
Eritrocite Red blood cells | 2,58 /Ul ↓ | 3,70-5,00 |
Hemoglobina Hemoglobin | 70 g/l ↓ | 120-160 g/l |
Trombocite Platelets | 502 U/l ↑ | 180-400 U/l |
VSH ESR | 22 mm/h ↑ | 0-12 mm/h |
Ureea Urea | 47,9 mmol/l ↑ | 2,5-8,3 mmol/l |
Creatinina Creatinine | 2230 mmol/l ↑ | 68-115 mmol/l |
Glucoza Glucose | 9,1 mmol/l ↑ | 3,8-5,8 mmol/l |
ALT ALT | 73 U/l ↑ | 0-49 U/l |
AST AST | 88 U/l ↑ | 0-46 U/l |
Acid uric Uric acid | 767,3 mmol/l ↑ | 0,250-0,440 mmol/l |
Notă: VSH – viteza de sedimentare a hematiilor, ALT – alaninaminotrasnferaza, AST – aspartataminotransferaza Note: ESR – erythrocyte sedimentation rate, ALT - alanine aminotransferase, AST – aspartat aminotransferase | ||
On 28.06.2021 the following imaging tests were performed:
abdominal ultrasound – normal rim of the liver, right lobe 170 mm; left lobe 76 mm, homogenous parenchyma. No free fluids in the abdominal cavity. Intrahepatic biliary ducts non-dilated, portal vein 13,5 mm. Deformed gallbladder. Pancreas not visible. Spleen 110 mm x 45 mm. Symmetrical kidneys. Rough kidney border. Right kidney 120 mm x 50 mm, parenchyma 18 mm. Left kidney 120 mm x 55 mm, parenchyma 19 mm. Deformed pyelocalyceal area. Both kidneys with increased echogenicity, and decreased echogenicity in the pyramids. Conclusion: hepatomegaly with moderate diffuse changes in the liver parenchyma. Chronic acalculous cholecystitis. Bilateral deformity of the collector system;
chest x-ray – normal coastal bones. Signs of venous congestions in both lungs. Reactive pulmonary hila. Clear diaphragm. Cardiomegaly. Aortic sclerosis.
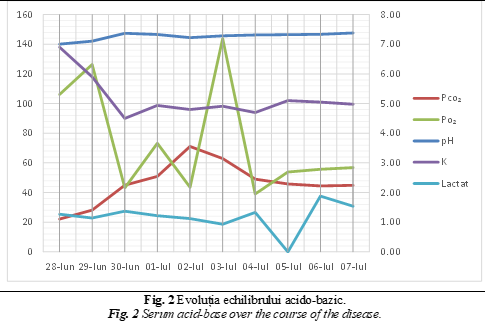
Patient has been consulted by the nephrologist, which established the diagnosis of acute kidney injury of unknown cause, with the recommendation to start acute hemodialysis. Patient was also examined by the rheumatologist with the following diagnosis: tophaceous gout, gouty arthritis, and gouty nephropathy. Acute kidney injury caused by gouty nephropathy with deposition of urate crystals in renal tubules. In the figure 1 and 2 are presented the results of the lab tests during admission.
On 29.06.2021 a repeated X-ray of the chest has been performed: Increased lung pattern due to broncho-vascular. Aortic sclerosis. Dilated heart.
According to the clinical and paraclinical test, the following diagnosis has been established: Intrinsic renal acute kidney injury, followed by gouty nephropathy with deposition of uric acid in the tubules. Hemodialysis (initiated on 29.06.2021). Primary gout, mixed variant, tophaceous chronic gout. Anemia of renal disease grade III. Hypertension grade 3, very high risk. Pectoris angina during exercise, functional class II. Mixed cardiomyopathy (hypertensive, metabolic, ischemic). Heart failure class II NYHA.
The following treatment was applied: the first hemodialysis session was performed on 29.06.2021. The session lasted 120 minutes, blood speed 250 ml/min, ultra-filtrate 500 ml, initial BP 170/90 mmHg. Patient received Sol. Natrium Chloride 0,9% 500 ml, Sol. Heparin 7500 UA, Sol. Glucose 40% - 60 ml. In total patient had 7 sessions of hemodialysis – 29.06.2021; 30.06.2021; 01.07.2021; 03.07.2021; 05.07.2021; 07.07.2021.
Taking into consideration the improvement of the general condition of the patient, he has been transferred to the Nephrology department on 06.07.2021 of the Municipal Clinical Hospital „Saint Trinity”. In the Nephrology department patient received transfusion of red blood cells, Aminoplasmal® 10% - 500 ml; Sol. Calcium chloride 500 mg – 5 ml; Sol. Magnesium chloride 250 mg – 5 ml; Sol. Famotidine 20 mg – 5 ml; Sol. Glucose 20% - 20 ml.
Patient has been discharged from the hospital on 08.07.2021 with the recommendation to continue chronic hemodialysis treatment.
Second clinical case
Patient B., female sex, 47 years old, from Stefan-Voda, admitted to the hospital for routine monitoring and treatment plan on 20.05.2021 in the nephrology department of the Republican Clinical Hospital „Timofei Mosneaga”. The patient complained of lumbar pain on the left side, dysuria, nocturia, slight edema on the lower limbs, marked fatigability, paresthesia. According to the history of the patient: in 2009 patient had a right nephrectomy due to a benign tumor. In 2013, at an ultrasound examination a 1.5 renal stone has been detected. Patient has been admitted in the nephrology department of the Republican Clinical Hospital „Timofei Mosneaga”. During admission it was discovered that patient had hyperuricemia and uricosuria, Proteus Mirabillis 106 CFU/ml at urine culture, with signs of hydronephrosis grade 1 in the left kidney as well as high blood pressure.
The patient has been evaluated by the urologist, who prescribed a conservative treatment (lithotripsy was contraindicated) and monitoring. In 2015 patient has given birth to two female twins. During the pregnancy patient did not administer any drugs for the comorbidities. In 2016 patient has been hospitalized for routine evaluation. A worsening evolution of the disease has been determined - increased blood pressure, decreased glomerular filtration rate to 68 ml/min, hydronephrosis grade II and the presence of bacteriuria, hyperuricemia, hyperuricosuria and the growth of the urinary calculus up to 2,1 cm and discovering of the second urinary calculus of 0,6 cm. In 2019 patient has been brought by the emergency medical services to the Municipal Clinical Hospital „Saint Trinity” in severe condition, with lumbar pain irradiating in the inguinal region, oliguria. After paraclinical evaluation, the patient was diagnosed with left ureter obstruction. A JJ stent has been placed with restoration of urinary flow. After a medical board meeting, it was decided to remove the urinary stone by endoscopic lithotripsy. After the surgical procedure and pharmacological treatment, patient was discharged in a improved state. The last hospitalization has been in May 2020. It was routine admission. Patient has 3 children, G2P2. No known allergies. Past medical history: right nephrectomy (2009), hypertension grade 3, high-risk (from 2013, treatment with Lercanidipine 10 q.d., Moxonidine 0.4 mg q.d.), Diabetes mellitus type 2 (since 2019, initially treated with Metformine 500 mg b.i.d., at the moment treated Insuline Detemir 12 IU morning and 12 IU evening).
Physical examination – active position, hyperstenic body constitution, height – 1,69 cm, weight – 90 kg, body mass index 31,51 – obesity class 1 (WHO). Mild edema on the lower legs, non-pitting. RR 18 /min, vesicular sounds bilateral. Blood pressure 140/90 mmHg, HR – 85 bpm. Palpation reveals mild discomfort on the whole abdomen area, liver +2 cm from the costal rim, spleen is not palpable, stool passing normal. Dysuria, nocturia, oliguria, costovertebral tenderness on the left side.
Diagnosis: Chronic pyelonephritis in exacerbation of the left solitary kidney. Right nephrectomy (2009). Gouty nephropathy. Chronic kidney disease G3 KDOQI (2021). Hyperuricemia. Functional joint insufficiency class I. Mixed chronic cardiopathy (hypertensive, metabolic). CHF class 2 NYHA. Diabetes mellitus type 2. Symmetrical bilateral sensitive polyneuropathy. Obesity class 1. The lab results are presented in table 2 and 3.
Urinalysis: White Blood cells cover the field. Red Blood cells 7/ HPF. Urine culture: Klebsiella Pneumonia 106 CFU/ml. Glomerular filtration rate measurement: GF 91,51 ml/min. 24-h urine protein loss (patient administer diuretics, diuresis 2750). Protein presence positive. Protein 1,0 g/l. Protein in 24 h 2,75 g/l.
Tabelul 2. Rezultatele hematologice. Table 2. Hematologic lab results. | ||||
Componentul investigat Parameter | 21.05.2021 | 24.05.2021 | 27.05.2021 | Valori de referință Reference values |
Leucocite White Blood Cells | 9,52↑ | 9,43↑ | 8,0 | 4,0-9,0/UI |
Eritrocite Red Blood Cells | 5,19↑ | 4,79 | 4,0 | 3,7-5,0/uL |
Hemoglobina Hemoglobin | 13,5 | 13,2 | 13,0 | 120-160 g/l |
Trombocite Platelets | 355,0 | 341,2 | 329,0 | 180-400 u/L |
VSH ESR | 27,0↑ | 25,0↑ | 20,0↑ | 0-12 mm/h |
Notă: VSH – viteza de sedimentare a hematiilor Note: ESR – erythrocyte sedimentation rate | ||||
Tabelul 3. Rezultatele analizelor biochimice. Table 3. Chemistry lab results. | |||
Componentul investigat Parameter | 21.05.2021 | 27.05.2021 | Valori de referință Reference values |
Ureea Urea | 19,5↑ | 10,3↑ | 2,5-8,3 mmol/l |
Creatinina Creatinine | 157↑ | 135↑ | 68-115 mmol/l |
Acidul uric Uric acid | 534,0↑ | 482,1↑ | 155,0-428,0 mmol/l |
Colesterol Cholesterol | 10,0↑ | 9,1↑ | 0-5,2 mmol/l |
Trigliceride Triglycerides | 6,70↑ | 5,98↑ | 0-1,7 mmol/l |
Glucoza Glucose | 7,0↑ | 6,9↑ | 3,8-5,8 mmol/l |
On 23.05.2021 patient performed the following investigations:
abdominal ultrasound: Liver: right lobe 16,8 cm, left lobe 8,7 cm, normal rim, signs of steatosis. Intrahepatic biliary ducts non-dilated. Portal vein 1,1 cm. Splenic vein 0,5 cm. Pancreas: head 3,3 cm, body 1,7 cm, tail 2,5 cm, homogenous structure. Spleen 8,4 x 2,5 cm. Kidney: right – surgically removed, left – 13,4 x 7,0 cm, deformed pyelocalyceal area – 1,6 cm. Multiple calculi up to 2,0 cm with acoustic shadowing. Empty urinary bladder;
computer tomoghrapy of the abdomen and pelvis with contrast medium. Signs of nephrolithiasis of the solitary kidney. Secondary hydrocalycosis grade I-II. Signs of tubulointerstitial nephropathy with moderate nephrosclerosis on the left. Hepatomegaly. Splenomegaly;
electrocardiogram. Sinus rhythm, 85 bpm. Horizontal electric axes.
According to the clinical and paraclinical (laboratory and imaging) test, the following diagnosis has been established: Clinical diagnosis: Chronic pyelonephritis in exacerbation of the left solitary kidney - Klebsiella pneumoniae 106. Right nephrectomy (2009 – benign tumor). Left nephrolithiasis. Left secondary hydrocalycosis grade I-II. CKD G2A1 KDIGO. Hyperuricemia. Mixed chronic compensated cardiopathy (hypertensive, metabolic). Hypertension grade II high risk. Diabetes mellitus type 2. Symmetrical bilateral sensitive polyneuropathy. Diabetic nephropathy stage 1 Mogensen. Mixed dyslipidemia. Obesity class 1. Gouty nephropathy. Chronic kidney disease G3A1 KDIGO. Hyperuricemia. Functional joint insufficiency class I. Mixed chronic cardiopathy (hypertensive, metabolic). CHF class 2 NYHA. Diabetes mellitus type 2. Symmetrical bilateral sensitive polyneuropathy. Obesity class 1.
Patient has received the following treatment during hospitalization - Sol.Ppiperacillin/Tazobactam 4,5 + Sol. Sodium chloride 0,9% 200 ml i/v; Sol. Tiocton 600 mg i/v; Sol. Furosemide 2 ml i/v; Sol. Pantoprazole 40 mg i/v; Fluconazole 150 mg.
Patient is discharged on the 28.05.2021 in better conditions.
Conclusions
Gout is more frequent in males than females – ratio 8:1. Hyperuricemia and gout leads to kidneys affection due to the deposition of monosodium urate monohydrate crystals in the renal interstitial tissue, which leads to chronic inflammation and precipitations of uric acid. These processes cause acute renal injury with urolithiasis, which positively correlates with the degree of hyperuricemia. In women, kidney involvement is more frequent after menopause, but usually it follows the joint involvement, or it affects both system at the same time (renal and articular). In males, due to hyperuricemia, primarily the joints are affected, later it is associated with gouty nephropathy or they develop parallelly.
Competing interests
None declared
Authors' contribution
All authors contributed equally to the research, data analysis, and writing of the manuscript. All authors read and approved the final article.
Authors’ ORCID IDs
Liliana Groppa - https://orcid.org/0000-0002-3097-6181
Serghei Popa - https://orcid.org/0000-0001-9348-4187
Svetlana Agachi - https://orcid.org/0000-0002-2569-7188
Dorian Sasu - https://orcid.org/0000-0002-5832-5954
Larisa Rotaru - https://orcid.org/0000-0002-3260-3426
References
Fathallah-Shaykh S.A., Cramer M.T. Uric acid and the kidney. Pediatr Nephrol. 2014 Jun. 29 (6):999-1008.
Ejaz A.A., Johnson R.J., Shimada M., et al. The Role of Uric Acid in Acute Kidney Injury. Nephron. 2019. 142 (4):275-283.
Dykman D., Simon E.E. Hyperuricemia and uric acid nephropathy. Arch Intern Med. 1987 Jul. 147(7):1341-5.
Borghi C., Rosei E.A., Bardin T., et al. Serum uric acid and the risk of cardiovascular and renal disease. J Hypertens. 2015 Sep. 33 (9):1729-41; discussion 1741.
Avram Z., Krishnan E. Hyperuricaemia - where nephrology meets rheumatology. Rheumatology (Oxford). 2008 Jul. 47(7):960-4.
Kanbay M., Yilmaz M.I., Sonmez A., et al. Serum uric acid independently predicts cardiovascular events in advanced nephropathy. Am J Nephrol. 2012. 36(4):324-31.
Kim Y.J., Kim C.H., Sung E.J., et al.. Association of nephrolithiasis with metabolic syndrome and its components. Metabolism. 2013 Jun. 62(6):808-13.
Emami-Naini A., Eshraghi A., Shahidi S., et al. Metabolic evaluation in patients with nephrolithiasis: A report from Isfahan, Iran. Adv Biomed Res. 2012. 1:65.
Roncal-Jimenez C., Garcia-Trabanino R., Barregard L., et al. Heat Stress Nephropathy From Exercise-Induced Uric Acid Crystalluria: A Perspective on Mesoamerican Nephropathy. Am J Kidney Dis. 2015 Oct 5.
Rotaru L., Groppa L., Pascari-Negrescu A., Agachi S., Chiaburu L. Afectarea renală în gută (revista literaturii). În: Anale științifice ale USMF „Nicolae Testemițanu” „Probleme actuale în Medicina Internă”. Chișinău, 2011, p. 125-129.
Rotaru L., Groppa L., Chiaburu L., Agachi S., Pascal R. Nefropatia uratică la pacienții cu gută. În: Materialele Conferinței Naționale în Medicină Internă în Republică Moldova cu participare internațională. Sănătate publică, nr.2 (2). 2011, p. 46-47.
Zubrițchi N., Rotaru L. Comorbidități în gută. În: Anale Științifice ale USMF „Nicolae Testemițanu”, vol.3, „Probleme actuale în medicina internă”. 2014, p. 175.
Rotaru L., Groppa L., Russu E. et al. Afectarea renală în gută. În: Buletinul Academiei de Științe a Moldovei. Științe Medicăle. Chișinău, 2017, 3(55), p. 62-66.
Ротару Л., Гроппа Л., Агаки С., Кишларь Л., Руссу Е. Поражение почек при подагре. В: Всероссийский конгресс с международным участием Дни Ревматологии в Санкт-Петербурге: Сборник тезисов. Санкт-Петербург, 23-24 сентября 2019, с. 221.

