Introduction
Chronic obstructive pulmonary disease (COPD), according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2020 report, is considered a rising public health problem with a significant socio-economic burden [1-4]. The magnitude of the condition is statistically suggested by its fourth place in the structure of death causes worldwide. The negative impact was revealed by the seventh place in the leading causes of disability in high-income countries and the tenth place in low- and middle-income countries, and it is an important cause of hospitalization worldwide. COPD mortality represents about 6% of all the deaths worldwide [4, 5].
The global prevalence of COPD varies by age: approximately 10% among adults aged 40-60 years, 18.8% among subjects aged 60-74 years, and 22.3% among men and 25% among women in the population aged 75 years and older [6-8].
Continuous exposure to COPD risk factors and demographic aging were the responsible predisposing factors for the condition level rising to third place in the structure of the death causes [9, 10]. COPD complications increase the risk of death due to other comorbidities; therefore, the health impact of COPD may be underestimated, considering that 50% of mortality in COPD patients is caused by non-respiratory diseases [5, 11, 12].
Specific to COPD in geriatrics are: (1) higher prevalence in the elderly; (2) higher severity of the disease; (3) a silent clinical picture in the early stages, with the disease being unrecognized and untreated until it progresses to a more severe degree; (4) the association with a large number of comorbidities (average of 9); (5) a higher mortality rate; (6) reduced therapeutic efficacy and (7) a significant quality of life impact [13-18]. Exacerbation of COPD in the elderly consisted of aggravation of the disease, the apparition of other symptoms and worsening of the pre-existing ones, a significant decline in functional and cognitive performance, a reduction in quality of life, and a poor prognosis. As a result, determining the evolution characteristics of COPD in elderly patients is regarded as critical for early COPD diagnosis, assessment of COPD secondary hemodynamic disorders, implementation of effective therapeutic interventions, and reduction of the economic impact on the public health system [11, 14, 19].
The high rate of cardiac comorbidities, installed early with a silent evolution, the existing interrelationship of cardiovascular complications with the severity of COPD, and the increase in exacerbations, hospitalizations, and fatal events due to cardiovascular implements dictate the need for correct diagnosis and management implementation of COPD in the elderly. Therefore, rational, generalizable, and cost-effective strategies were necessary to identify cardiovascular complications, especially pulmonary hypertension and heart failure, in elderly patients with stable or exacerbated COPD in order to reduce the impact of the disease on this group of patients [20-22].
Lately, the detection of hemodynamic impairment in COPD patients presented deficiencies since their non-invasive diagnostic methods did not always provide relevant data and invasive diagnostic methods were difficult to perform, requiring increased possibilities and costs. Highlighting the specific clinical and paraclinical aspects of hemodynamic impairment in COPD patients will allow the elucidation of relevant paraclinical methods for detecting cardiovascular involvement with the application of the adapted treatment strategy.
Timely, accurate diagnosis and subsequent management of PH are very important because, despite therapeutic progress, survival in this group remains suboptimal [12, 15].
Currently, the need to evaluate new biomarkers in COPD has been highlighted, but their implementation in clinical practice has been largely unsuccessful. BNP and NT-proBNP levels have not been adequately studied in patients with lung diseases and cardiac complications, specifically in COPD associated with PH or cor pulmonale, with the goal of estimating prognostic value and mortality risk in these cases [7, 23]. Moreover, data on natriuretic peptides in elderly patients are very rare, and examination of plasma NT-proBNP in elderly patients with COPD in the Republic of Moldova has not been performed.
The goal of the work presented is to perform a diagnostic evaluation of the clinical, objective, and paraclinical status of elderly COPD patients with or without hemodynamic disorders, with a focus on the relevance of NT-proBNP levels in those patients.
Material and methods
To accomplish our purpose, we performed an analytical, observational, case-control study with the use of modern research methods.
The study included 194 elderly patients (≥ 65 years old) who were admitted to the Geriatrics ward of the Ministry of Health Clinical Hospital for inpatient treatment and met the inclusion criteria. The overall study group was divided into 2 subgroups according to the presence of PH: subgroup 1 – 97 patients with COPD without PH (COPD group); subgroup 2–97 patients with COPD and secondary PH (PHCOPD group). The data were collected during the inpatient stay, coded, and statistically processed.
Eligibility criteria
Eligible patients for the study included: (1) patients with chronic obstructive pulmonary disease with various severity degrees (obligatory presence of clinical and paraclinical features); (2) possible associations of hemodynamic disorders in COPD patients; (3) the age of patients older than 65 years; (4) agreeing to and signing the informed consent for inclusion in the study; and (5) integral mental health and intellectual capacities in the patients included in the study.
The study protocol was reviewed and approved by the Research Ethics Committee of PI Nicolae Testemițanu SUMPh nr. 1 on July 12, 2022. Each patient signed a consent form to participate in the study after being fully informed about the study's purpose and objectives, as well as the obligations, benefits, and risks of the investigations carried out in accordance with the study protocol.
Investigation methods
The patients were examined using biochemical methods, instrumental methods (spirometry, pulse oximetry, electrocardiogram, ultrasonography of internal organs, chest x-ray, and transthoracic echocardiography), a functional exam with the 6-minute walk test, a multidimensional assessment of COPD (estimation of dyspnea (modified dyspnea severity scale – mMRC), symptom assessment (COPD assessment test – CAT, COPD clinical questionnaire – CCQ), quantification of the quality of life (respiratory questionnaire of the „Saint George" hospital – SGRQ), and the prognoses determination (BODE index, 6-minute walk test – 6MWT). All patients in the study were evaluated using the survey method.
The volume of the representative sample was calculated in Program F tests – ANOVA (fixed effects, omnibus, one-way analysis; A-priori sample size calculator) – and established the research requirement of 192 patients.
The primary materials of the study were entered into an electronic database and processed on the personal computer using the functions and modules of the programs "Statistical Package for the Social Science" (SPSS) version 16.0 for Windows (SPSS Inc., Belmont, CA, USA, 2008) and Microsoft Office Excel 2019 through descriptive and inferential statistical procedures.
For the comparative analysis of the indicator values, we applied mathematical-statistical techniques (dynamic series indicators, proportional indicators, average values, etc.).
Results
Socio-demographic data
The study groups included 97 (50.0%) patients with pulmonary hypertension secondary to COPD (PHCOPD group) aged 65–90 years and 97 (50.0%) patients with COPD without secondary pulmonary hypertension (COPD group) aged 65–86 years. The study groups were similar according to sex, living environment, social status, living conditions, risk factors (smoking and household pollution), number of comorbidities, general condition, duration of current hospitalization, and number of hospitalizations in the last year (Table 1). Exposure to occupationally harmful substances was more significant in the PHCOPD group (55–56.7%) vs. (38–39.2%) in the COPD group.
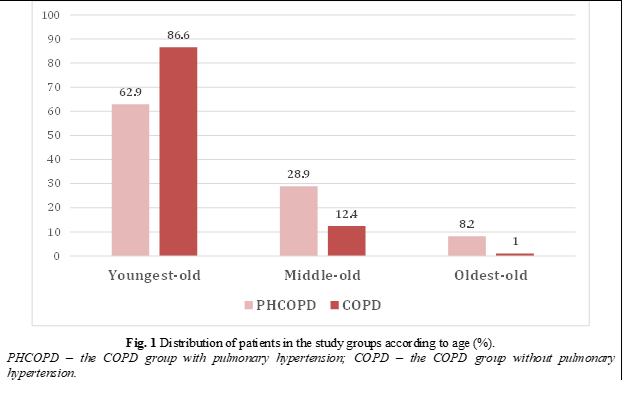
The mean age was statistically significantly higher in the PHCOPD patient group (73.35±0.7 years; p < 0.01) compared to patients in the COPD group (70.32±0.5 years; p < 0.01). In the COPD patients group, youngest-old were statistically significantly more frequently included (84–86.6% vs. 61–62.9%, respectively; p < 0.001), and in the group of patients with PHCOPD – middle-old (28–28.9 % vs. 12–12.4%, respectively; p < 0.01) and oldest-old (8–8.2% vs. 1–1.0%, respectively; p < 0.05) (Fig. 1).
Table 1. Socio-demographic parameters and risk factors in patients in the study groups. | |||||
Parameters | PHCOPD | COPD | p | ||
abs. | % | abs. | % | ||
Gender: - men - women |
65 32 |
67,0 33,0 |
70 27 |
72,2 27,8 |
NS NS |
Living environment: - rural - urban |
85 12 |
87,6 12,4 |
80 17 |
82,5 17,5 |
NS NS |
Social status: - intellectuals - workers - farmers |
27 51 19 |
27,8 52,6 19,6 |
28 55 14 |
28,9 56,7 14,4 |
NS NS NS |
Living conditions: - satisfactory - unsatisfactory |
93 4 |
95,9 4,1 |
93 4 |
95,9 4,1 |
NS NS |
Smoking: - never smoked - ex-smoker - currently smokes |
54 30 13 |
55,7 30,9 13,4 |
54 28 15 |
55,7 28,9 15,5 |
NS NS NS |
Note: PHCOPD – the COPD group with pulmonary hypertension; COPD – the COPD group without pulmonary hypertension; abs. – absolute values; p – probability rate; NS – insignificant. | |||||
The evaluation of the patients autonomy according to the functional estate revealed that patients from the PHCOPD group had statistically more frequent pulmonary and cardiovascular causes of dependence and the IIIA degree of dependence (92.8% vs 73.2%, respectively; p < 0.001), but patients from the COPD group had somatic causes of dependence and the IIIB degree of dependence (24.7% vs 3.1%, respectively; p < 0.001).
Clinical picture
Cough and productive cough were comparable in both the PHCOPD and COPD patient groups. A small amount of morning or evening expectoration was statistically significantly more frequent in the COPD patients group (76–78.4% vs. 5–5.2%, respectively; p < 0.001), but an average amount (48–49.5% vs. 21–21.6%, respectively; p < 0.001) and a high amount (44–45.4% vs. 0%, respectively; p < 0.001) of expectoration throughout the entire day were statistically significantly more frequent in the PHCOPD patients group.
All patients from both study groups complained of dyspnea. The COPD group of patients had expiratory type dyspnea (62–63.9% vs. 36–37.1%, respectively; p < 0.001), dyspnea on mild exertion (64–66.0% vs. 10–10.3%, respectively; p < 0.001), the accentuation of respiratory signs at mild exertion (68–70.1% vs. 13–13.4%, respectively; p < 0.001) and at increased physical effort (13–13.4% vs. 3.1%, respectively; p < 0.01).
The PHCOPD group of patients had mixed dyspnea (60–61.9% vs. 34–35.1%, respectively; p < 0.001), which accentuates on minimal exertion (85–87.6% vs. 33–34.0%, respectively; p < 0.001), wheezing (77–79.4% vs. 16–16.5%, respectively; p < 0.001), accentuation of respiratory signs even during speech (8–8.2% vs. 1–1.0%, respectively; p < 0.05) and minimal exertion (73–75.3% vs. 15–15.5%, respectively; p < 0.001), low-grade fever (28–28.9% vs. 2–2.1%, respectively; p < 0.001) and dysphonia (62–63.9% vs. 12–12.4%, respectively; p < 0.001).
Although both study groups experienced chest pain (89–91.8% in the COPD group vs. 95–97.9% in the PHCOPD group), the COPD group had a more frequent mild degree of chest pain (55–61.8% vs. 9–9.5%, respectively; p < 0.001), while the PHCOPD group reported more frequently moderate (68–71.6% vs. 34–38.2%, respectively; p < 0.001) and severe pain (18–18.9% vs 0–0%, respectively; p < 0.001).
The mean number of comorbidities was also similar in both study groups: 8.4±0.3 (from 3 to 15 comorbidities) in patients from the PHCOPD group and 8.26±0.2 (from 4 up to 14 comorbidities) in patients from the COPD group (p > 0.05).
The objective examination
At the objective examination, the patients of the PHCOPD group had statistically significantly more frequent central cyanosis (19–19.6% vs. 3–3.1%, respectively; p < 0.001), forced body position (73–75.3% vs. 3–3.1%, respectively; p < 0.001), peripheral edema (90–92.8% vs. 70–72.2%, respectively; p < 0.001), emphysematous chest (43–44.3% vs. 9–9.3%, respectively; p < 0.001), hyperresonant percussion sound (97–100.0% vs. 51–52.6%, respectively; p < 0.001), diffuse dry rales, accentuation of the second sound over pulmonary artery (95–97.9% vs. 64–66.0%, respectively; p < 0.001).
The PHCOPD group presented higher mean values of systolic blood pressure (138.57±1.2 mmHg vs. 128.61±1.0 mmHg, respectively; p < 0.001), diastolic blood pressure (84.99±0.6 mmHg vs. 81.93±0.7 mmHg, respectively; p < 0.001), heart rate (75.71±1.2 beats per minute vs. 69.98±1.0 beats per minute, respectively; p < 0.01), respiratory rate (20.91±0.2 cycles per minute vs. 19.62±0.09 cycles per minute, respectively; p < 0.001). On the other hand, the COPD group more frequently presented higher mean values of oxygen saturation (96.79±0.07% vs. 95.36±0.1%, respectively; p < 0.001).
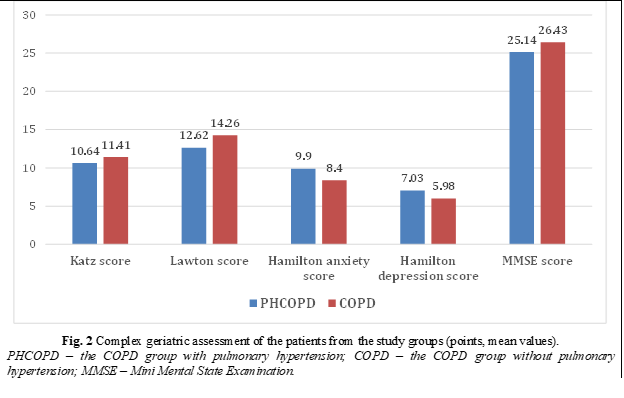
At the complex geriatric assessment, the COPD group of patients showed a higher degree of independence and more clarity of thought. Those facts were revealed by the higher mean values of the Katz score (11.41±0.09 points vs. 10.64±0.1 points, respectively; p < 0.001), of the Lawton score (14.26±0.2 points and 12.62±0.2 points, respectively; p < 0.001), and of the MMSE score (26.43±0.2 points vs. 25.14±0.2 points, respectively; p < 0.001) in the COPD group. On the other hand, the PHCOPD group of patients showed statistically significantly higher mean values of the Hamilton anxiety score (9.90±0.2 points and 8.4±0.3 points, respectively; p < 0.001), of the Hamilton depression score (7.03±0.3 points and 5.98±0.3 points, respectively; p < 0.05), and mild cognitive impairment according to the MMSE test (Fig. 2).
According to the Katz score, independent patients were statistically significantly more common in the COPD group (57–58.8% vs. 30–30.9%, respectively; p < 0.001), but patients with moderate dependence (19–19.6% vs. 2–2.1%, respectively; p < 0.001) were statistically significantly more frequent in the PHCOPD group.
According to the Lawton score, independent patients were statistically significantly more frequent in the COPD group (45–46.4% vs. 13–13.4%, respectively; p < 0.001), but there were statistically significantly more patients with moderate dependence (55–56.7% vs. 24–24.7%, respectively; p < 0.001) in the PHCOPD group.
Although COPD exacerbations were found in all study groups, patients in the COPD group mentioned rare COPD exacerbations (≤ 1) in the previous year statistically significantly more frequently (58–59.8% vs. 13–13.4%, respectively; p < 0.001), and PHCOPD patients mentioned frequent COPD exacerbations (≥ 2) statistically significantly more frequently (84–86.6% vs. 39–40.2%, respectively; p < 0.001).
According to the COPD GOLD classification (2007/2017), the moderate COPD in the COPD group of patients was found statistically more frequently (81–83.5% vs. 11–11.3%, respectively; p < 0.001), but the patients from the PHCOPD group had severe COPD (79–81.4% vs. 16–16.5%, respectively; p < 0.001), very severe COPD (7–7.2% vs. 0–0%, respectively; p < 0.01) and COPD of type D (96–99.0% vs. 89–91.8%, respectively; p < 0.05).
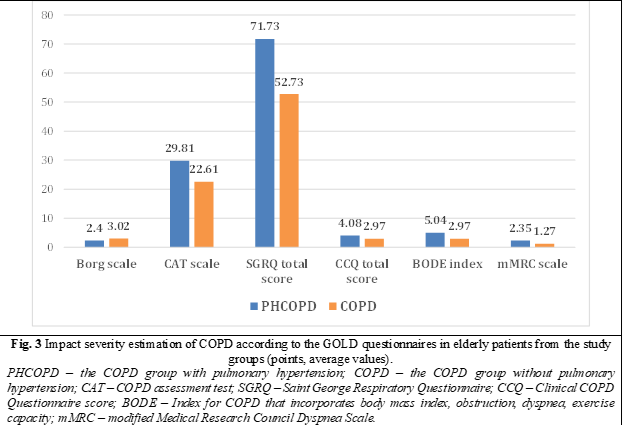
Themultidimensional assessment of COPD found higher average values in the PHCOPD group of patients in comparison with the COPD group of patients. The impact of COPD on health and daily life activities is revealed by the higher value of the CAT scale in the PHCOPD group (29.81±0.5 points vs. 22.61±0.5 points, respectively; p < 0.001). The mean values of SGRQ questionnaire were higher in PHCOPD group, and namely total score (71.73±1.2 points vs. 52.73±1.0 points, respectively; p < 0.001), the SGRQ symptom score (74.63±1.3 points vs. 54.77±0.9 points, respectively; p < 0.001), the SGRQ activity score (75.40±1.1 points vs. 63.87±0.8 points, respectively; p < 0.001), and the SGRQ impact on daily activities score (68.69±1.5 points vs. 45.41±1.4 points, respectively; p < 0.001). The COPD influence on clinical picture and daily living activities was proved by CCQ score, that was higher in PHCOPD group: the CCQ total score (4.08±0.08 points vs. 2.97±0.07 points, respectively; p < 0.001), the CCQ symptom score (4.54±0.08 points vs. 3.17±0.07 points, respectively; p < 0.001), the CCQ functional status score (3.57±0.08 points vs. 2.43±0.08 points, respectively; p < 0.001), and the CCQ mental state score (4.16±0.1 points vs. 3.64±0.1 points, respectively; p < 0.01). The assessment of COPD dyspnea revealed higher mean values in the PHCOPD group according to the BODE index (5.04±0.1 points vs. 2.97±0.1 points, respectively; p < 0.001) and mMRC dyspnea scale (2.35±0.06 points vs. 1.27±0.06 points, respectively; p < 0.001) (Fig. 3).
In the COPD group of patients, the mean value of the Borg scale was statistically significantly higher compared to the PHCOPD group (3.02±0.05 points vs. 2.4±0.05 points, respectively; p < 0.001).
When comparing the mMRC scale, the second (59–60.8% and 28–28.9%, respectively; p < 0.001) and third degrees of dyspnea (33–34.0% and 2–2.1%, respectively; p < 0.001) were found statistically significantly more often in the PHCOPD group.
Although both study groups had similar mean values of the Charlson comorbidity index (CCI) (6.56±0.2 points in the PHCOPD group vs. 6.33±0.2 points in the COPD group), according to the degree classification, patients in the COPD group had a statistically more frequently moderate CCI score (3-4 points) (18–18.6% vs. 8–8.2%, respectively; p < 0.05), whereas patients in the PHCOPD group had a more frequently high CCI score (≥ 5 points) (89–91.8% vs. 79–81.4%, respectively; p < 0.05).
Pre-test patient assessment when performing the 6MWT revealed statistically significantly higher mean values in the PHCOPD group compared to the COPD group according to the following indices: systolic blood pressure (137.32±1.1 mmHg vs. 128.11±0.9 mmHg, respectively; p < 0.001 ), diastolic blood pressure (84.32±0.6 mmHg vs. 81.82±0.6 mmHg, respectively; p < 0.01), heart rate (75.13±1.2 beats per minute vs. 69.77±0.9 beats per minute, respectively; p < 0.001), respiratory rate (20.84±0.2 cycles per minute vs. 19.60±0.09 cycles per minute, respectively; p < 0.001). On the other hand, the mean values of O2 saturation (96.82±0.07% vs. 95.45±0.1%, respectively; p < 0.001), Borg scale (3.01±0.05 points vs. 2.40±0.05 points, respectively; p < 0.001), and walking distance (321.57±4.7 meters vs. 255.19±5.4 meters, respectively; p < 0.001) were higher in patients from the COPD group (Table 2).
The analysis of the post-test data reveals the same tendency of statistically average values, which are higher in the PHCOPD group compared to the COPD group. The mean value of O2 saturation (94.09±0.1% vs. 91.78±0.2%, respectively; p < 0.001) was statistically significantly higher in patients from the COPD group.
Table 2. Parameters before and after the 6-minute walk test at patients from the study groups. | ||||||
Parameters | PHCOPD group pre-test | COPD group pre-test |
p
| PHCOPD group post-test | COPD group post-test | p |
SBP (mmHg) | 137.32±1.1 | 128.11±0.9 | < 0.001 | 151.09±1.2 | 139.07±0.8 | < 0.001 |
DBP (mmHg) | 84.32±0.6 | 81.82±0.6 | < 0.01 | 92.86±0.6 | 90.05±0.4 | < 0.001 |
HR (beats per minute) | 75.13±1.2 | 69.77±0.9 | < 0.001 | 89.43±1.6 | 81.55±1.1 | < 0.01 |
Respiratory rate (cycles per minute) | 20.84±0.2 | 19.60±0.09 | < 0.001 | 28.13±0.8 | 26.76±0.8 | < 0.001 |
SaO2 (%) | 95.45±0.1 | 96.82±0.07 | < 0.001 | 91.78±0.2 | 94.09±0.1 | < 0.001 |
Borg scale (points) | 2.40±0.05 | 3.02±0.05 | < 0.001 | 2.58±0.2 | 2.45±0.07 | < 0.05 |
Walked distance (m) | 255.19±5.4 | 321.57±4.7 | < 0.001 |
| ||
Note: SBP – systolic blood pressure; DBP – diastolic blood pressure; HR – heart rate; SaO2 – blood saturation with oxygen; PHCOPD – the COPD group with pulmonary hypertension; COPD – the COPD group without pulmonary hypertension; p – probability rate. | ||||||
As per the results of the 6MWT test according to the distance walked, the PHCOPD group had lower exercise tolerance (75–77.3% vs. 19–19.6%, respectively; p < 0.001), while moderate exercise tolerance (75–77.3% vs. 21–21.6%, respectively; p < 0.001) was statistically significantly more frequent in the COPD group.
Chronic respiratory failure of different degrees was detected in all patients included in the study. The first degree of respiratory failure was more frequent in patients from the COPD group (60–61.9% vs. 6–6.2%, respectively; p < 0.001), while the second degree of chronic respiratory failure (86–88.7% vs. 37–38.1%, respectively; p < 0.001) and the third degree of chronic respiratory failure (5–5.2% vs. 0–0%, respectively; p < 0.05) were detected statistically more often in the PHCOPD group.
Functional respiratory examination through spirometry revealed statistically lower mean values of the main respiratory indices in patients from the PHCOPD group compared to the COPD group: FEV1 (42.81±0.8% vs. 53.80±0.6%, respectively; p < 0.001), FVC (59.31±1.2% vs. 65.05±0.9%, respectively; p < 0.001), FEV1/FVC (56.17±0.8% vs. 63.53±0.5%, respectively; p < 0.001), and FEF (32.44±1.1% vs. 46.33±1.0%, respectively; p < 0.001) (Table 3).
Table 3. Spirometry parameters (%) before and after the bronchodilation test at patients from the study groups | ||||||
Parameters | PHCOPD group pre-test | COPD group pre-test |
p
| PHCOPD group post-test | COPD group post-test | p |
FEV1 | 42.81±0.8 | 53.80±0.6 | < 0.001 | 45.64±0.8 | 55.90±0.6 | < 0.001 |
FVC | 59.31±1.2 | 65.05±0.9 | < 0.001 | 62.03±1.3 | 67.02±0.9 | < 0.01 |
FEV1/FVC | 56.17±0.8 | 63.53±0.5 | < 0.001 | 57.58±0.8 | 64.03±0.5 | < 0.001 |
FEF | 32.44±1.1 | 46.33±1.0 | < 0.001 | 35.54±1.0 | 46.94±1.0 | < 0.001 |
Note: FEV1 – forced expiratory volume in the first second; FVC – forced vital capacity; FEF – forced expiratory flow; PHCOPD – the COPD group with pulmonary hypertension; COPD – the COPD group without pulmonary hypertension; p – probability rate. | ||||||
Spirometry parameters after the bronchodilator test had the same tendency, with lower mean values in the PHCOPD group, namely FEV1 (45.64±0.8% vs. 55.90±0.6%, respectively; p < 0.001), FVC (62.03±1.3% vs. 67.02±0.9%, respectively; p < 0.01), FEV1/FVC (57.58±0.8% vs. 64.03±0.5%, respectively; p < 0.001), and FEF (35.54 ±1.0% vs. 46.94±1.0%, respectively; p < 0.001).
Laboratory and instrumental examination (electrocardiographic, radiological, echocardiographic, and ultrasonographic examination of internal organs) revealed several parameters occurring statistically significantly more often in the PHCOPD group compared to the COPD group.
The radiological examination found that in the PHCOPD group, there were more frequent susceptible signs for chronic bronchitis (96–99.0% and 81–83.5%, respectively; p < 0.001), susceptible signs for bronchial obstruction (50–51.5% and 9–9.3%, respectively; p < 0.001), and susceptible signs for pulmonary emphysema (34–35.1% and 6–6.2%, respectively; p < 0.001).
Electrocardiography revealed that the patients in the PHCOPD group presented more often with signs of right atrial hypertrophy, such as pulmonary P waves in II, III, aVF, and V1-V2 leads (33–34.0% and 2–2.1%, respectively; p < 0.001) and signs of right ventricle hypertrophy. The signs of right ventricle hypertrophy found more frequently in the PHCOPD group were right axis deviation (76–78.4% vs. 7–7.2%, respectively; p < 0.001), increase in wave amplitude in leads III, aVF, and V1-V2 (75–77.3% vs. 1–1.0%, respectively; p < 0.001) and ST segment depression in leads II, III, aVF, and V1-V2 (40–41.2% vs. 24–24.7%, respectively; p < 0.05).
Echocardiography revealed that the patients in the PHCOPD group presented more often with increased right ventricle wall thickness over 5 mm (93–95.9% vs. 4–4.1%, respectively; p < 0.001), right ventricle dilatation over 26 mm (94–96.9% vs. 3–3.1%, respectively; p < 0.001), and a higher mean pulmonary artery pressure (42.44±1.4 mmHg vs. 19.26±0.2 mmHg, respectively; p < 0.001).
The ultrasonography of internal organs found that dilation of the suprahepatic veins greater than 10 mm (58–59.8% vs. 0–0%, respectively; p < 0.001), dilation of the inferior vena cava greater than 20 mm (57–58.8% vs. 0–0%, respectively; p < 0.001), and venous congestion of the liver (56–57.7% vs. 2–2.1%, respectively; p < 0.001) occurred more frequently in the PHCOPD group.
Polycythemia was found to be more common in the PHCOPD group (20–20.6% vs. 8–8.2%, respectively; p < 0.05), as well as C-reactive protein (7.78±0.9 mg/dL vs. 5.77±0.8 mg/dL, respectively; p < 0.001), fibrinogen (4.23±0.4 mg/dL vs. 3.47±0.09 mg/dL, respectively; p < 0.05), and mean values of NT-proBNP (1807.16±91.5 pg/mL vs. 138.65±8.3 pg/mL, respectively; p < 0.001).
The microscopic examination of sputum in the PHCOPD group revealed increased number of epithelial cells (17.41±0.7 vs. 13.99±0.7 in the visual field, respectively; p < 0.01), macrophages (7.24±0.5 vs. 5.65±0.3 in the visual field, respectively; p < 0.01), and leukocytes (22.16±1.1 vs. 18.69±1.0 in the visual field, respectively; p < 0.01).
Discussions
Therefore, the complex geriatric assessment in the PHCOPD group, compared to the COPD group, revealed statistically significantly more frequent and severe complaints. The cough was more severe, and expectoration was moderate to severe throughout the day. Dyspnea was of mixed type and occurred with minimal physical exertion. The clinical picture in the PHCOPD group was completed by wheezing, accentuation of respiratory signs during speech, minimal physical exertion, low fever, moderate chest pain, and severe chest pain. PH in elderly COPD patients has a negative impact on the clinical picture and an unfavorable impact on daily activities.
The objective examination determined a statistically significant negative impact on the objective health status of elderly PHCOPD patients: lower mean values of SaO2 and statistically significantly higher mean values of blood pressure, cardiac contraction frequency, and respiratory frequency. Patients with PHCOPD had significantly more frequent signs of respiratory system impairment caused by disease severity, hemodynamic alterations, and advanced age, such as peripheral edema, central cyanosis, forced body position, emphysematous ribcage, participation of the rib cage in the act of breathing, widening of the intercostal spaces during inspiration, active participation of additional respiratory muscles in the process of breathing, hypersonic percussive sound, decrease in pulmonary respiratory excursion, diffuse dry rales, prolonged exhalation, and accentuation of the second sound over the pulmonary artery.
The complex geriatric evaluation outlined the repercussions of PH and COPD on quality of life and independence. The mean values of the Katz, Lawton, and Hamilton anxiety scores, the Hamilton depression score, and the MMSE score indicate that the COPD group has a statistically higher prevalence of mild dependence or independence, the absence of anxiety and depression, and the absence of cognitive disorders. Meanwhile, patients in the PHCOPD group had statistically higher rates of moderate dependence, mild cognitive impairment, moderate anxiety, and moderate depression, confirming the impact of the complex COPD on their daily lives.
Clinical functional examination of elderly COPD patients found a moderate degree of COPD (types B and C were statistically significantly more frequent in patients from the COPD group). The severe and very severe degrees of type D COPD are statistically significantly more frequent in patients from the PHCOPD group, thus presenting the correlation between the severity of COPD and hemodynamic disorders in elderly COPD patients.
In the PHCOPD group, the multimodal approach to COPD revealed statistically significantly higher mean values of the CAT scale, SGRQ score, CCQ score, BODE index, and mMRC dyspnea scale; this suggests the impact of COPD on the health status, quality of life, and outcome. The statistically significantly higher mean value of the Borg scale in the COPD group of patients suggests that a physical exertion reserve is available.
The COPD group of patients had statistically significantly more frequent values of 0 and the first dyspnea degree in the evaluation of patients according to the mMRC dyspnea scale, but the PHCOPD group of patients had statistically significantly more frequent second and third degrees of dyspnea.
The 6MWT test revealed that low exercise tolerance was statistically more common in the PHCOPD group and moderate exercise tolerance was statistically more common in the COPD patient group.
Although chronic respiratory failure was diagnosed in all patients in the study groups, the first degree of chronic respiratory failure was statistically significantly more common in the COPD group, but the second and third degrees of chronic respiratory failure were found to occur statistically significantly more often in the PHCOPD group of patients.
At the same time, the PHCOPD patients had more frequent electrocardiographic changes characteristic of right heart damage with right ventricular hypertrophy and right atrial hypertrophy that occur because of PH and the elderly body's reduced capacity to compensate for them.
Furthermore, the PHCOPD group of patients had statistically more frequent echocardiographic changes characteristic of right ventricular affection as a result of the PH secondary to the COPD.
Furthermore, the PHCOPD group had a statistically higher rate of inflammatory response syndrome in blood tests, as well as polycythemia, as a result of bronchial obstruction and its association with pulmonary hypertension. The presence of pulmonary hypertension and right atrial hypertrophy correlated with the increase in the value of natriuretic peptides (NT-proBNP), arguing the necessity of natriuretic peptides evaluation in geriatric patients as an informative and safe diagnostic method. Also, the level of natriuretic peptides correlated with the presence of ultrasonographic signs of right heart failure, such as dilation of the suprahepatic veins more than 10 mm, dilation of the inferior vena cava more than 20 mm, and venous congestion of the liver, a fact that once again recommends the application of the NT-proBNP marker in the diagnostic procedure of elderly patients with COPD complicated by PH.
Conclusions
The comparative complex geriatric evaluation of patients with COPD reveals the presence of the characteristic symptoms in all the patients, but they are much more severe in those from the PHCOPD group, with a more significant impact on the quality of life and a greater deterioration of the assessed paraclinical indices.
Arrhythmias, right ventricular hypertrophy, right atrial hypertrophy, and even right heart failure are more common in elderly patients in the PHCOPD group, which has a negative impact on quality of life, self-care capacity, physical effort capacity, and clinical and paraclinical indices.
Pulmonary hypertension has a significant impact on the clinical aspects of elderly patients with COPD, a fact reflected in the scores of the complex geriatric assessment, the multidimensional assessment scales of COPD, and the 6-minute walk test. Also, the impact can be confirmed by the data of the paraclinical laboratory examination, in which the inflammatory response syndrome and the increase in natriuretic peptides correspond to the data of the ultrasound examination of the heart and internal organs.
The significant negative impact of COPD on elderly patients argues for the need to assess each elderly patient's functional estate at the time of admission for an opportune diagnosis of COPD.
The important impact of PH secondary to COPD requires the mandatory implementation of new techniques of PH diagnosis, like natriuretic peptides.
Abbreviations
COPD – chronic obstructive pulmonary disease; PHCOPD – the group of patients with chronic obstructive pulmonary disease and pulmonary hypertension; COPD group – the group of patients with chronic obstructive pulmonary disease without pulmonary hypertension; GOLD – Global Initiative for Chronic Obstructive Lung Disease; CAT – COPD assessment test; SGRQ – the St George’s Respiratory Questionnaire; CCQ – the clinical questionnaire for COPD; mMRC – Modified Medical Research Council Dyspnea Scale; BODE index – index of body mass, obstruction, dyspnea and exertion; NT-proBNP – B-type natriuretic peptide; 6MWT – the 6-minute walking test; PAP – pulmonary artery pressure; MMSE – mini mental examination test; FEV1 – forced expiratory volume in the first second; FVC – forced vital capacity; FEF – forced expiratory flow; PH – pulmonary hypertension.
Competenig interests
None declared
Authors’ contributions
Both authors contributed equally to the manuscript's writing and have read and approved the final version of the manuscript.
Authors’ ORCID IDs
Ecaterina Luca – https://orcid.org/0000-0002-6782-1829
Nicolae Bodrug – https://orcid.org/0000-0003-0295-1574
References
Corlateanu A. Current approaches to COPD in 2019. Curr Respir Med Rev. 2019;15(2):69-70. doi: 10.2174/1573398X1502191014114230.
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2020 report [Internet]. Long Grove: GOLD; 2020 [cited 2022 Dec 13]. Available from: https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-…
Moscovciuc A, Scaletchi V, Simionica I; Ministry of Health, Labor and Social Protection of Republic of Moldova. [Chronic obstructive pulmonary disease: National clinical protocol (PCN-18)]. Chisinau: The Ministry; 2020. 47 p. Romanian.
Kaur A, Goyal A, Pandhi N. To study the correlation of chronic obstructive pulmonary disease (COPD) assessment test, clinical COPD questionnaire and BODE index in patients of stable COPD. Assam J Intern Med. 2022;12(1):18-23. doi: 10.4103/ajoim.ajoim_21_21.
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2022 report [Internet]. Long Grove: GOLD; 2022 [cited 2022 Dec 13]. Available from: https://goldcopd.org/2022-gold-reports/.
Mathioudakis A, Sivapalan P, Papi A, Vestbo J; DECODE-NET Investigators. The DisEntangling Chronic Obstructive Pulmonary Disease Exacerbations clinical trials NETwork (DECODE-NET): rationale and vision. Eur Respir J. 2020;56(1):2000627. doi: 10.1183/13993003.00627-2020.
Spannella F, Giulietti F, Cocci G, Landi L, Lombardi F, Borioni E, et al. Acute exacerbation of chronic obstructive pulmonary disease in oldest adults: predictors of in-hospital mortality and need for post-acute care. J Am Med Dir Assoc. 2019;20(7):893-898. doi: 10.1016/j.jamda.2019.01.125.
Halpin D, Criner G, Papi A, Singh D, Anzueto A, Martinez F, et al. Global Initiative for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease. The 2020 GOLD Science Committee Report on COVID-19 and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2021;203(1):24-36. doi: 10.1164/rccm.202009-3533SO.
Hawkins N, Virani S, Ceconi C. Heart failure and chronic obstructive pulmonary disease: the challenges facing physicians and health services. Eur Heart J. 2013;34(36):2795-2803. doi: 10.1093/eurheartj/eht192.
Bossone E, D'Andrea A, D'Alto M, Citro R, Argiento P, Ferrara F, et al. Echocardiography in pulmonary arterial hypertension: from diagnosis to prognosis. J Am Soc Echocardiogr. 2013;26(1):1-14. doi: 10.1016/j.echo.2012.10.009.
van Mourik Y, Rutten F, Bertens L, Cramer M, Lammers J, Gohar A, et al. Clinical research study implementation of case-finding strategies for heart failure and chronic obstructive pulmonary disease in the elderly with reduced exercise tolerance or dyspnea: a cluster randomized trial. Am Heart J. 2020;220:73-81. doi: 10.1016/j.ahj.2019.08.021.
Bodrug N, Antonova N, Catană S, Pascari N. [Aspects of the treatment of chronic pulmonary heart disease Bronchopulmonary diseases at the turn of the millennium]. Materials of the scientific-practical conference. Chisinau; 1999. p. 34-36. Romanian.
Siafakas N, Bizymi N, Mathioudakis A, Corlateanu A. EARLY versus MILD Chronic Obstructive Pulmonary Disease (COPD). Respir Med. 2018;140:127-131. doi: 10.1016/j.rmed.2018.06.007.
Mendez-Bailon M, Lawrence-Villalba N, Rosemary-Correa M, Josa-Laorden C, Inglada-Galiana L, Menor-Campos E, et al. Chronic obstructive pulmonary disease in elderly patients with acute and advanced heart failure: palliative care needs-analysis of the EPICTER Study. J Clin Med. 2022;11(13):3709. doi: 10.3390/jcm11133709.
Butorov I, Antonova N, Butorov S, Calancea V. [Clinical-functional state of the myocardium in patients with chronic obstructive pulmonary disease]. In: Scientific Annals of Nicolae Testemitanu State University of Medicine and Pharmacy . Chisinau: Medicina; 2013. Vol. 3. p. 439-444. Romanian.
Martîniuc C, Matcovschi S, Pisarenco S. [Updates in the diagnosis of pulmonary hypertension in patients with chronic obstructive pulmonary disease]. [Public Health Econ Manag Med (Chisinau)]. 2016;(2):26-32. Romanian.
Tsiligianni I, Kocks J. Daytime symptoms of chronic obstructive pulmonary disease: a systematic review. NPJ Prim Care Respir Med. 2020;30(1):6. doi: 10.1038/s41533-020-0163-5.
Calancea V, Matcovschi S, Ghicavii N, Dumitras T, Bodrug N, Cretu A. Peculiarities of cardiac rhythm in stable chronic obstructive pulmonary disease. Eur Respir J. 2017;50(Suppl 61):PA3645.
Diaconu C. [Exacerbation of chronic obstructive bronchopneumopathy in the elderly patient: diagnostic and therapeutic conduct]. [Med Pract]. 2011;6(3):199-202. Romanian.
Labaki W, Xia M, Murray S, Curtis J, Barr R, Bhatt S, et al. NT-proBNP in stable COPD and future exacerbation risk: Analysis of the SPIROMICS cohort. Respir Med. 2018;140:87-9. doi: 10.1016/j.rmed.2018.06.005.
Corlăteanu A. Multidimensional assessment of chronic obstructive pulmonary disease. Chişinău: Medicina; 2017. 178 p. ISBN 978-9975-82-069-1.
Ribeiro S, Cardoso C, Valério M, Machado J, Costa J, Rodrigues C, et al. Confirmatory evaluation of the modified medical research council questionnaire for assessment of dyspnea in patients with chronic obstructive pulmonary disease in Portugal. Acta Med Port. 2022;35(2):89-93. doi: 10.20344/amp.15208.
Chen Y, Chen V, Hollander Z, Leipsic J, Hague C, DeMarco M, et al. C-reactive protein and N-terminal prohormone brain natriuretic peptide as biomarkers in acute exacerbations of COPD leading to hospitalizations. PLoS One. 2017;12(3):e0174063. doi: 10.1371/journal.pone.0174063.

